The sugar substitute is known for its potential to lower blood pressure and blood sugar, but some research suggests it may disrupt more than the gut microbiome
Stevia, known for its zero calories and potential benefits, such as lowering blood pressure and blood sugar, is often considered an excellent substitute for sugar. However, is this sweetener—used by Paraguayans for over a thousand years and by the Japanese for several decades—truly free from side effects?
Stevia Is Excreted, but Liver Problems May Pose Issue
Generally, stevia is thought to be metabolized and excreted without accumulating in the body.
Stevia’s sweetness comes from steviol glycosides. Steviol glycosides are a group of substances, among which stevioside and rebaudioside A are the two most common in commercial products.
Our stomachs and upper small intestines cannot break down or absorb steviol glycosides. Therefore, ingested steviol glycosides enter the lower gastrointestinal tract intact. In the colon, gut bacteria break down steviol glycosides into steviol, a process completed within 24 hours. Subsequently, most of the steviol is rapidly absorbed into the bloodstream through the intestinal wall, while any unabsorbed steviol is excreted in feces. The steviol entering the bloodstream is further metabolized into steviol glucuronide in the liver and ultimately excreted in the urine. This is why human experiments have shown no detectable levels of steviol in the blood after consuming steviol glycosides, while steviol glucuronide is detected in urine, and steviol is found in the feces.
“Factors like diet, medication use, or individual differences could potentially impact the metabolism of stevia and its metabolites,” said Lisa Young, an adjunct professor of nutrition in the Department of Nutrition and Food Studies at New York University and a registered dietitian nutritionist, in an email interview with The Epoch Times. She noted that while rare, some individuals may experience adverse reactions or intolerance to steviol, which “could cause gastrointestinal symptoms, allergic reactions, or other health concerns.”
Additionally, she emphasized the crucial role of the liver in the metabolism of stevia, indicating that liver diseases or impaired liver function may impact this process. “Individuals with liver diseases or those taking medications that affect liver function may need to exercise caution regarding the consumption of stevia.”
Potential Impact of Stevia on Gut Microbiome
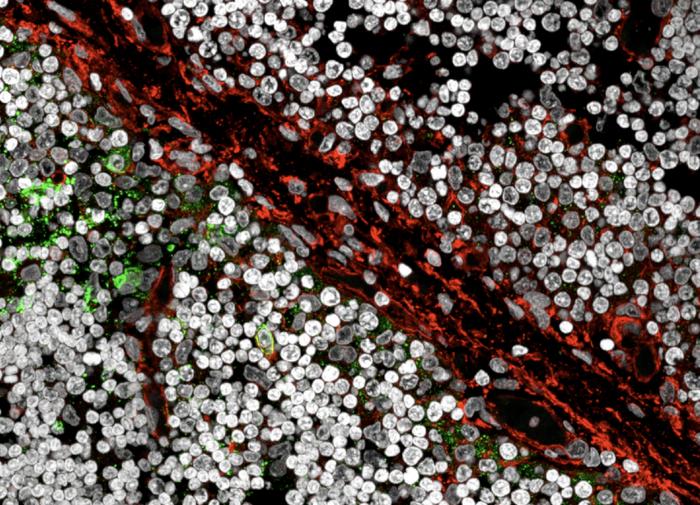
Some in vitro and animal experiments have found that stevia or steviol may potentially impact the gut microbiome.
An animal study published in Nutrients in 2019 revealed that, compared to those only drinking water, rebaudioside A consumption altered the gut microbiome composition in mice. However, Ms. Young noted that while the hindgut microbiome of mice and humans share some similarities, many bacteria present in the mouse gut are absent in humans. Therefore, there are certain limitations to animal studies
A study conducted by Israeli scientists in 2020 revealed that stevia and steviol do not possess bactericidal properties. However, they may potentially interrupt communication among Gram-negative bacteria in the gut, leading to gut microbial imbalance. Additionally, steviol may also exhibit inhibitory effects on the competition among gut bacteria
Lactobacillus reuteri is often incorporated into food as a probiotic. In an earlier study, stevioside and rebaudioside A were found to inhibit the growth of six strains of Lactobacillus reuteri, with the inhibitory effects varying depending on the specific strain.
An in vitro experiment published in the journal Genes in 2019 suggested that in a simulated human intestinal environment, steviol decreased the population of Bifidobacteria (healthy bacteria), hindered the degradation of bacterial food, and concurrently led to an increase in colonic pH.
Another in vitro experiment, published in the Journal of Agricultural and Food Chemistry in 2019, demonstrated that sweetener products containing steviol glycosides and erythritol altered the structure and diversity of the human gut microbiome to some extent. However, the study concluded that, overall, there was no negative impact on the gut microbial community due to the consumption of stevia.
A review published in Microbiology in 2022 indicated that current knowledge about stevia’s impact on the gut microbiome has primarily come from in vitro and animal studies. Due to a lack of randomized clinical trials conducted in human populations, there is no definitive evidence to elucidate how stevia influences the gut microbiome, and further research is needed.
Ms. Young noted that the impact stevia has on the gut microbiome remains an active area of research, and conclusions may vary. However, she emphasized that “most studies face limitations in terms of biological relevance because it is challenging to directly apply tested concentrations to human exposure levels.”
Gastrointestinal Discomfort Caused by Stevia-Based Products
The adverse effects of stevia-based products often do not stem from steviol glycosides.
As steviol glycosides are several hundred times sweeter than sucrose, most stevia-based products on the market are not 100 percent pure steviol glycosides. Instead, they often consist of a blend of steviol glycosides and some sugar alcohols. For example, you might find a combination of 1 percent steviol glycosides and 99 percent erythritol. These products are commonly found in supermarkets, usually as white crystalline powders, their appearance resembling that of granulated or powdered sugar.
Ms. Young stated that erythritol, present in stevia-based products, is recognized by the U.S. Food and Drug Administration (FDA) as generally recognized as safe (GRAS). However, excessive consumption can result in side effects such as bloating, cramps, flatulence, or diarrhea. Additionally, the inclusion of other substances like sugar alcohol in stevia products may also cause adverse effects, especially for individuals sensitive to these additives.
There are eight types of sugar alcohols approved by relevant regulatory authorities for use as sweeteners in food, including erythritol, hydrogenated starch hydrolysates, lactitol, isomalt, mannitol, maltitol, sorbitol, and xylitol. Some individuals may experience various gastrointestinal discomforts after consuming these substances.
Specifically, sugar alcohol substances may increase gas production after fermentation by bacteria in the gut, contributing to bloating in the gastrointestinal tract. Additionally, these substances can lead to the retention of water in the small intestine, causing abdominal discomfort. Sugar alcohols also impose a greater osmotic load on the gut, leading to increased water concentration in the colon and resulting in loose stools. Moreover, the fermentation of sugar alcohols in the gut may impact the intestinal environment by altering the gut microbiome and its metabolism, influencing the intestinal immune barrier, and potentially increasing the risk of a so-called “leaky gut.”
However, it is important to note that there is a significant variation in symptoms among those who consume sugar-alcohol substances. Factors such as the type of sugar alcohol, the amount ingested, the consumption of food alongside the substance, and the intestinal ability to reabsorb water can all lead to different outcomes. Moreover, people with lower gastrointestinal tolerance or those with intestinal diseases tend to experience more symptoms than healthy people.
The substances present in stevia-based products may also impact cardiovascular health.
A review published in Nature Medicine in 2023 highlighted a link between erythritol consumption and an increased risk of adverse cardiovascular events (including death or nonfatal heart attacks or strokes) and the formation of thrombosis. The researchers stated that further research on the long-term safety of erythritol is warranted. However, it is important to note that some controversy surrounds this study.
Potential Impact of Stevia on the Brain and Nervous System
Scientists have also assessed the potential impact of stevia and its metabolites on the brain and nervous system. However, due to medical ethical considerations, these studies are primarily conducted through animal experiments.
The previously mentioned 2019 animal study suggested that the consumption of stevia may impact the dopamine reward system in the brain.
In 2020, two clinical doctors jointly published a case report, suggesting for the first time a potential association between the symptoms of restless legs syndrome (RLS) and the consumption of stevia. A patient developed symptoms of RLS while using stevia, and these symptoms resolved after discontinuation. Several months later, upon a trial reintroduction of stevia, the RLS symptoms reappeared within two days. The doctors proposed that stevia might selectively reduce dopamine levels in specific regions of the brain, or the intake of stevia could affect iron absorption. Both factors are considered significant contributors to RLS.
In addition to potentially affecting the dopamine system, animal experiments have shown that stevia may also influence memory.
Researchers at the University of Southern California published a study in 2022 where they provided juvenile rats with either artificial sweeteners or water with added stevia for a month and then tested their memory. The results revealed that both artificial sweeteners and stevia impaired the rats’ memory compared to those only drinking water. These rats were less likely to remember objects or navigate through mazes successfully. A study conducted by Filipino researchers in 2015 revealed that mice consuming stevia or two other artificial sweeteners (aspartame and sucralose) showed no significant difference in their learning ability in a water maze compared to mice drinking only water. However, mice consuming stevia exhibited higher levels of cell death in the hippocampus. Another study also conducted in the Philippines in 2014 found that mice with a higher intake of stevia, compared to those only drinking water, exhibited a longer duration of reaction when subjected to heat, suggesting that stevia might inhibit the sensitivity of the mice’s nervous system.
Stevia May Disrupt Endocrine Function and Affect Immunity
In the body, steviol glycosides are first metabolized into steviol, which possesses a steroid-like structure. Therefore, researchers suspect that stevia may act as an endocrine disruptor.
For instance, a cell experiment demonstrated that a certain concentration of steviol could disrupt the endocrine function of human sperm cells and also impact cell viability.
Another study found that stevia consumption led to changes in the number of immune cells in the lymph nodes of mice. Compared to mice drinking only water, those consuming stevia showed an increase in the count of two types of immune cells and a decrease in another type. Additionally, there were varying degrees of changes in some hormones within the mice’s bodies.
In 2020, Brazilian researchers published an in vitro study in Immunopharmacology and Immunotoxicology, revealing that exposure to steviol led to a decrease in human lymphocyte quantity, accompanied by gradual DNA damage and structural changes. Therefore, the study proposed that, under certain concentrations and conditions, steviol exhibits cytotoxic, genotoxic, and mutagenic effects. An earlier study also suggested that, although steviol glycosides seem not to exhibit cytotoxicity, steviol itself possesses mutagenic properties.
Safety of Stevia in Human Studies
However, the experiments mentioned above, which indicate the effects of stevia or its metabolites, were not conducted on humans. In other words, the experimental conditions and subjects differ from those of the human body.
Per Bendix Jeppesen, who is currently studying stevia extract as an anti-diabetic drug and as a healthy sweetener and is an associate professor in the department of endocrinology and diabetes at Aarhus University in Denmark, told The Epoch Times that stevia is safe, stating, “It is the most researched sweetener in the world.” He elaborated: “The European Food Safety Authority (EFSA) are using 10 years to go through all materials. All kinds of studies and publications have been really looked into and they gave this permission (to use stevia).”
Mr. Jeppesen also pointed out, “Cell studies will never be able to replace in vivo studies as animal or human intervention studies.” This is because, in in vivo studies, the human body functions as a whole organism, with different organs working together, whereas in cell studies, it typically involves cells from a specific organ and cannot fully reflect the overall complexity of the organ.
Jan Geuns, a professor in the Department of Biology at Katholieke Universiteit Leuven in Belgium, who has researched stevia for many years, expressed in an email to The Epoch Times that extensive experiments have been conducted on animals as well as healthy subjects. Throughout the process, “we hoped to find other metabolites than steviol or steviol glucuronide. However, no other metabolites could be found.” He also pointed out that steviol glycosides and their metabolites do not accumulate in the human body.
Mr. Geuns also mentioned that “steviol glycosides are not easily absorbed in cells and, therefore, cell studies have nothing to do with the way steviol glycosides behave in man.” Additionally, he explained that once excreted from the body, steviol glucuronide continues to be further degraded by microorganisms, including those in the soil, and does not accumulate in the environment. “This cannot be said about compounds like sucralose, which has recently been proven to be carcinogenic and which is accumulating in surface waters and occurs in tap water.
“I think that sufficient studies have been done on the safety of steviol glycosides (and stevia),” he concluded.
A 2021 review recognized the safety of stevia, citing as primary evidence its historical use in the Paraguayan population for over 1,500 years and decades-long consumption by the Japanese without any reported side effects.
A study published in Nutrition Today in 2015 proposed that there were over 200 studies at that time confirming the safety of stevia. Additionally, a review published in 2023 in the journal Molecules also asserted that most existing human experiments suggest the safety of stevia consumption for the general population—“Although neither the applicability of stevioside in children, pregnancy, nor lactation has been evaluated, preclinical and clinical evidence of its safety allows it to be recommended, respecting the [acceptable daily intake