Recent research reveals that Neanderthals commonly hunted the extinct straight-tusked elephant, challenging previous notions of their social organization and survival strategies
Finds in Eastern Germany indicate that Neanderthals accumulated large quantities of meat and fat, or gathered in bigger groups for the consumption of elephants.
New research conducted by a team consisting of members of Johannes Gutenberg University Mainz (JGU), the Leibniz-Zentrum für Archäologie (LEIZA), also based in Mainz, and Leiden University in the Netherlands has found that Neanderthals extensively hunted the now extinct straight-tusked elephant (Palaeoloxodon antiquus).
The study has recently been published in the journal PNAS. The researchers closely examined the bones of elephants that are approximately 125,000 years old and that were discovered in Gröbern in Saxony-Anhalt and Taubach in Thuringia, Germany, decades ago. They were able to identify cut marks made by stone tools used by the Neanderthals that indicate that the animals must have been hunted before they were extensively butchered.

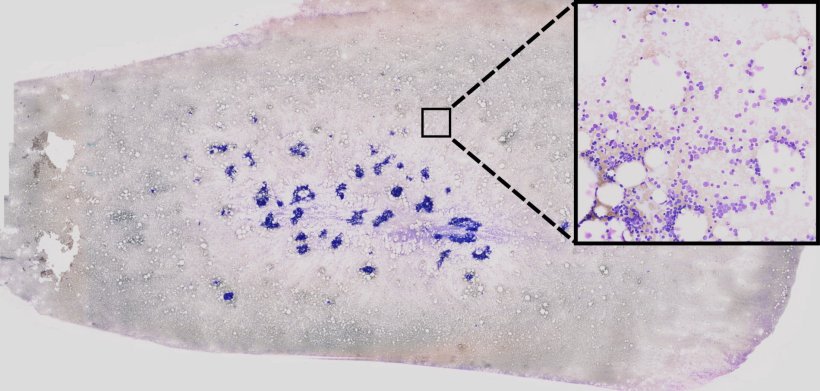
The pelvic bone of a Palaeoloxodon antiquus found in Gröbern.
The pelvic bone of a Palaeoloxodon antiquus found in Gröbern. Credit: Lutz Kindler, LEIZA
It was two years ago that the same team during the analysis of bones found at the Neumark-Nord site, in a former lignite mine in Saxony-Anhalt, discovered the very first evidence that Neanderthals actively hunted straight-tusked elephants, the largest terrestrial mammals of the Pleistocene. This study was published in Science Advances in early 2023.
“The results of the more recent examination of the bones from Gröbern and Taubach now show that the hunting of these elephants by Neanderthals was not an isolated phenomenon but must have been a more regular activity,” emphasized Sabine Gaudzinski-Windheuser, Professor of Prehistoric and Protohistoric Archaeology at JGU and Director of the Archaeological Research Center and Museum of Human Behavioral Evolution MONREPOS in Neuwied, an institute run under the aegis of LEIZA. Gaudzinski-Windheuser was extensively involved in the investigation of the bones from Gröbern and Taubach as well as the previous study of the bones from the Neumark-Nord site.

Incisions some 5 millimeters in length made by Neanderthals on the Palaeoloxodon antiquus pelvic bone from Gröbern.
Incisions some 5 millimeters in length made by Neanderthals on the Palaeoloxodon antiquus pelvic bone from Gröbern. Credit: Lutz Kindler, LEIZA
The yield of a straight-tusked elephant bull would have been sufficient to cover the daily calorie requirements of 2,500 Neanderthals
Palaeoloxodon antiquus roamed the landscapes of Europe and Western Asia 800,000 to 100,000 years ago. With shoulder heights of up to four meters and body masses of up to 13 tons, the European straight-tusked elephant was the largest land-living animal at the time, significantly larger than today’s African and Asian elephants and even bigger than the extinct woolly mammoth.
“We have estimated that the meat and fat supplied by the body of an adult Palaeoloxodon antiquus bull would have been sufficient to satisfy the daily calorie intake of at least 2,500 adult Neanderthals,” explained Gaudzinski-Windheuser. “This is a significant number because it furnishes us with new insights into the behavior of Neanderthals.”
Dr. Lutz Kindler documenting fragments of Palaeoloxodon antiquus teeth discovered in Taubach. Credit: Wil Roebroeks, Leiden University
So far, for instance, research has generally assumed that Neanderthals gathered in groups of no more than 20 individuals. However, the information now obtained in relation to the systematic exploitation of straight-tusked elephants indicates that Neanderthals must have gathered, at least temporarily, in larger groups or mastered techniques that allowed them to preserve and store large quantities of foodstuffs – or both.
In a follow-up project, the researchers hope to learn more about how Neanderthals hunted these massive elephants and how their hunting activities impacted these and other prey animals as well as their environments.