Amid a Rise in Confirmed Cases of Measles, Dr Toni Hazell Emphasises the Importance of Recognising This Highly Contagious Infection in Nine Top Tips for Primary Care
| Read this Article to Learn More About: |
|---|
| concerns about a possible measles outbreak in Londonthe complications of measles, and how to make a diagnosisvaccine hesitancy, and talking to parents who are unsure about vaccination.Reflect on your learning and download our Reflection Record. |
In 2022, there were 54 confirmed cases of measles in England, whereas in the first half of 2023, there have already been 128 cases.1 Two-thirds of these cases occurred in London, but there has been at least one case in every region of the UK.1
UK Health Security Agency (UKHSA) modelling shows that there are now significant concerns about a large outbreak in London and smaller outbreaks in specific populations elsewhere in the UK.1 Groups at risk include younger people aged 19–25 years (babies born in 1998, the year that Andrew Wakefield’s measles, mumps, and rubella [MMR] paper was published, are now 25 years old), people from undervaccinated communities, and those who are susceptible to measles and have travelled overseas.1
Those who watched Professor Chris Whitty’s briefings during the COVID-19 pandemic may remember how we all got a bit obsessed with the R number. If R is below one, each case of an infection produces less than one secondary case, so the number of infected people declines; conversely, if R is greater than one, cases will increase, as each person infects at least one more.In relation to COVID-19, the R numbers discussed were generally below five;2 the R number for measles is generally cited as somewhere between 12 and 18, and it is therefore extremely infectious.3
This article recaps the signs, symptoms, complications, and management of measles, covering vaccine hesitancy and evidence on the safety of vaccination, in nine top tips for GPs.
1. Take Measles and its Complications Seriously
A key trope of antivaxxers is that the infections that healthcare professionals aim to protect people against through vaccination are harmless ‘rites of passage’ of childhood, and that it is healthier for children to acquire the infections and fight them naturally.4 This is categorically untrue for measles. In developed countries, 10–20% of those who catch measles will experience some sort of complication, and the complication rate is probably higher in developing countries.5 Some complications of measles are shown in Box 1.5
| Box 1: Complications of Measles5 |
|---|
| Susceptibility to opportunistic infection is increased for a period of several weeks to months, and this effect may last up to three years after the person has recovered from measles, as the measles virus suppresses the reaction of the immune system to other pathogens.Many organ systems may be affected, but respiratory and gastrointestinal complications are the most common.Secondary infections of the respiratory tract include:otitis media (7–9% of cases).pneumonitis.tracheobronchitis.pneumonia (1–6% of cases).Central nervous system complications include:convulsions (about 1 in 200 cases).encephalitis (about 1 in 1000 cases).subacute sclerosing panencephalitis (SSPE)—a rare but serious degenerative disease of the central nervous system involving seizures and a decline in motor, cognitive, and behavioural function. It affects about 1 in 25,000 people with measles. SSPE is 16 times more common in children who contract measles at a very young age (less than 1 year). SSPE occurs a median of 7 years after exposure to the virus, although it may occur as late as three decades afterwards, and is invariably fatal.Diarrhoea affects about 8% of cases and may cause dehydration. Stomatitis is another complication of the digestive tract.Blindness can result from measles keratoconjunctivitis or other ocular complications, and occurs mainly in children with vitamin A deficiency. Measles is a leading cause of childhood blindness globally.© NICE 2022. Measles: what are the complications? NICE Clinical Knowledge Summary. NICE, 2022. Available at: cks.nice.org.uk/topics/measles/background-information/complications All rights reserved. Subject to Notice of rights. NICE guidance is prepared for the National Health Service in England. All NICE guidance is subject to regular review and may be updated or withdrawn. NICE accepts no responsibility for the use of its content in this product/publication. See www.nice.org.uk/re-using-our-content/uk-open-content-licence for further details |
Subacute sclerosing panencephalitis (SSPE) deserves a particular mention here because, unusually, it presents some years after the initial diagnosis of measles.5 A patient with SSPE will present with seizures and a decline in motor, cognitive, and behavioural function around 7 years after their measles infection, and the condition is always fatal.5 If a patient presents with these symptoms, it is worth asking if they have ever had measles, and if they are vaccinated.5
Medical writers around the world could spend years trying to describe what a nasty infection measles is, and they would not come close to the simplicity of Roald Dahl’s description of the death of his daughter Olivia:6
‘Olivia, my eldest daughter, caught measles when she was seven years old. As the illness took its usual course I can remember reading to her often in bed and not feeling particularly alarmed about it. Then one morning, when she was well on the road to recovery, I was sitting on her bed showing her how to fashion little animals out of coloured pipe-cleaners… I noticed that her fingers and her mind were not working together and she couldn’t do anything.
“Are you feeling all right?” I asked her.
“I feel all sleepy,” she said.
In an hour, she was unconscious. In twelve hours she was dead.’
2. Learn to Recognise a Case of Measles
Despite the fact that there are nearly 300,000 licensed doctors in the UK,7 as well as a growing number of other healthcare professionals, it is likely that most will never have seen a case of measles. To see measles regularly, a healthcare professional would need to have been working before 1968, when around 80% of the population contracted measles during childhood.8
Signs and Symptoms
Measles has a prodromal phase, which occurs about 10–12 days after exposure to the virus and lasts for 2–4 days before the rash appears.9 Symptoms include conjunctivitis and those of any viral infection—fatigue, malaise, cough, and a runny nose. During this period, the fever increases to 39°C before decreasing. A maculopapular erythematous rash starts on the face and behind the ears, and then spreads to the torso, limbs, and peripheries (see Figure 1).9 This is a key differentiator from other rashes, such as that of scarlet fever,10 which start on the torso. The rash fades after 5–7 days.9 The patient may also have Koplik spots on the buccal mucosa—these 2–3-mm wide red spots with a white centre are pathognomonic for measles (see Figure 2).9
Figure 1: Measles Rash

Figure 2: Koplik Spots
.jpg)
Risk Factors
Risk factors for contracting measles include being unvaccinated and in contact with a case of measles.9 Those who are vaccinated can occasionally contract the infection (known as a breakthrough case), but this is unusual and causes fewer infections, and the symptoms are usually milder.9
3. Manage Suspected Measles in Primary Care by Isolating Patients and Notifying the Local Health Protection Team
If the patient is systemically unwell enough to need a referral to secondary care, healthcare professionals must make it clear that they suspect measles, as there may be arrangements in place to keep them separate from other patients.11 Similarly, if someone with suspected measles visits the practice, it is necessary to find them somewhere other than the waiting room to wait.12
Public Health Management
Clinicians are required to notify their local health protection team about any suspected case of measles, which will arrange to take swabs.12 Vulnerable contacts will be assessed for possible post-exposure prophylaxis, so if clinicians happen to know that there is a pregnant woman or an immunocompromised person in the household, this is useful information to pass on.12 Healthcare professionals can find their local health protection team using this search tool.13
Disease Management in Primary Care
Management of measles in primary care is entirely symptomatic, and includes rest, adequate fluid intake, and use of paracetamol and ibuprofen for symptom relief.11 Aspirin should be avoided in children aged younger than 16 years.11 The infected person should stay away from school, nursery, or work for at least 4 days after the initial development of the rash, and should avoid contact with infants and those who are not fully immunised, pregnant, or immunosuppressed.11 If there are any signs of complications, medical attention should be sought; these may include shortness of breath, a temperature that cannot be controlled, seizures, drowsiness or an alteration in level of consciousness.11
4. Understand Current Guidance on Reimbursement for Childhood Vaccinations
The 2021/22 GP contract removed exception reporting for vaccinations while maintaining an 87% threshold for Quality and Outcomes Framework points for MMR and introducing a potential clawback of item of service payments for practices that do not maintain an 80% uptake.14 This means that, if parents cannot be persuaded to vaccinate their children, practices will lose out financially through no fault of their own, with concerns raised that some will lose tens of thousands of pounds.14 At the time of writing, calls for payment at lower tiers or the re-introduction of exception reporting for those who refuse have not yet been heeded. This is likely to entrench health inequalities, with practices in areas of high vaccine refusal and a more mobile population (often areas of deprivation) feeling that they cannot afford to spend time trying to increase uptake, as that time will not be resourced.14
5. Be Aware of Myths Linking Vaccination to Autism
In 1998, Andrew Wakefield and colleagues published a paper in The Lancet suggesting that the MMR vaccination was associated with behavioural regression and autism.15 Although the article was disputed almost immediately and later retracted, the damage was done, and MMR uptake rates started to fall.15 It was later revealed that Wakefield had significant conflicts of interest and stood to gain financially from the increased use of single vaccines.16 This is discussed in much more detail in a previous Guidelines in Practice article on vaccination myth-busting.16
The UK has never met the World Health Organization (WHO) target of 95% coverage with two doses of the MMR.17,18 This is the level considered necessary to achieve and maintain measles elimination.17 The UK came close in 1994, with 92% uptake of the vaccine but, after publication of the Wakefield paper, uptake fell to around 80%.17 It improved in the 2000s and early 2010s and, by 2017, the WHO declared that the UK had eliminated measles, with first-dose coverage reaching 95%.17 However, uptake fell steadily from then, declining more sharply during the COVID-19 pandemic (see Figure 319); in England, it currently stands at 89.5% for the first dose and 85.6% for the second dose, with lower figures in London (82.5% for the first dose at 2 years of age, and 74.1% for both doses at 5 years of age).17 Certain populations have particularly low uptake, and these are being targeted with education campaigns, often involving religious leaders.17,20
Figure 3: MMR Vaccine Coverage at Age 24 Months in the UK, 2009–202219
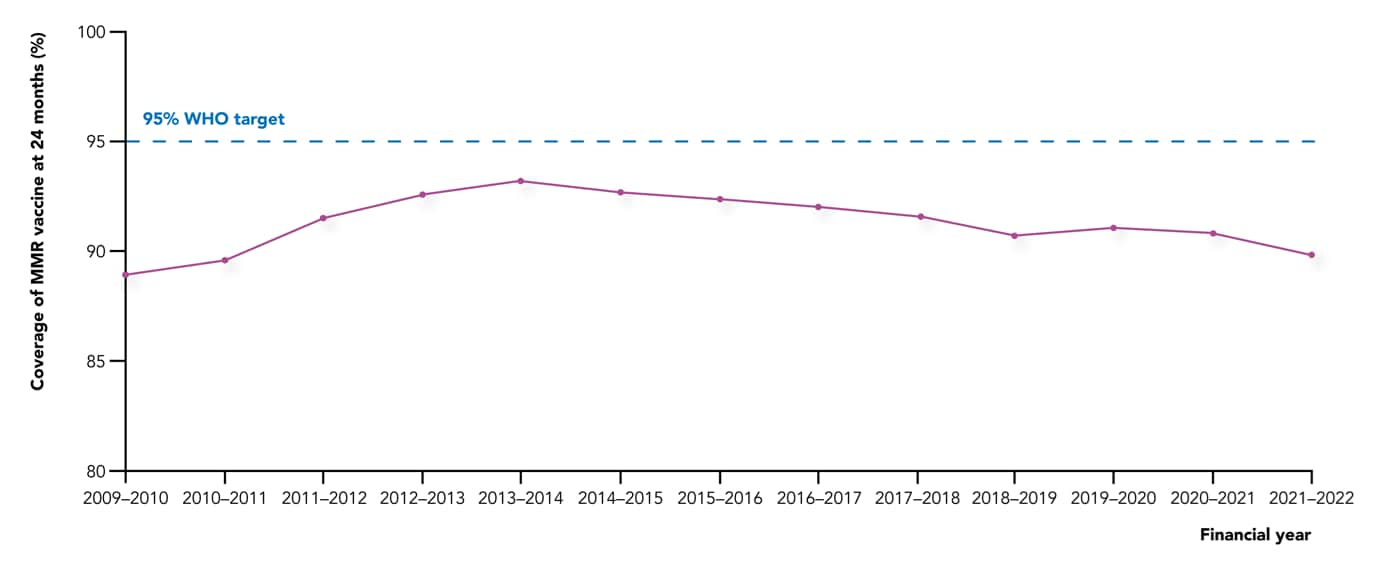
Contains public sector information licensed under the Open Government Licence v3.0.
6. Recognise that Vaccine Hesitancy is still Prevalent
Vaccine hesitancy is significantly related to organised campaigns on social media, including misinformation campaigns that start from outside the UK, particularly from Russia.21 Some studies have indicated a link between the likelihood of receiving the COVID-19 vaccine and the quality of the news articles that an individual liked or shared on X (formerly known as Twitter).22 There have been calls for social media companies to be more proactive in taking down antivaccination content in an attempt to combat the current situation,23 in which some people may be in an online ‘echo chamber’ of people with similar antivaccination views, and are therefore not exposed to accurate information. Some social media platforms have announced that they will reject antivaccination advertisements, and that searches on measles or vaccine safety will now only show links to reputable public health organisations.23
7. Tackle Vaccine Hesitancy with Evidence when Possible
When trying to advise a parent who doesn’t want their child to be vaccinated against measles, it is helpful to know if they are vaccine hesitant or a ‘vaccine denier’. The WHO defines vaccine deniers as ‘people who have a very negative attitude towards vaccination and are not open to a change of mind no matter the scientific evidence’.24 Vaccine deniers are a small subgroup of the wider vaccine hesitancy continuum, and any attempt to change their views will likely fail. The WHO advises that, in a discussion with a vaccine denier, the target audience is the public who are listening to the debate, and the aim is to strengthen their resilience against antivaccine rhetoric.24 In the context of primary care, this target audience may be the other parent or any other adult who is in the room, but if you speak to a true vaccine denier alone, then you are probably wasting your time. Those who are vaccine hesitant, however, may be persuaded, so it is important that clinicians have the facts at their fingertips.
8. Signpost Patients to Data on the Safety of Vaccination
The measles chapter of the UKHSA Green book has a list of useful points that could form the basis of a discussion with a parent who is still worried about autism, including:25
- children who have had the MMR vaccine do not have an increased risk of autism compared with unvaccinated children
- symptoms of autism are not clustered around the period after the vaccination
- when Japan discontinued the MMR vaccine in 1993, the incidence of autism continued to rise
- there is no correlation between autism rates and vaccine coverage
- no vaccine virus can be detected in children with autism.
9. Appreciate the Legal Situation if Two Parents Disagree
Children are often brought for vaccination by one parent, and practices do not generally contact the other parent to ask for their permission. However, the situation is different if it is known that someone with parental responsibility does not want the child to be vaccinated. In that case, even though vaccination is in the best interest of the child, practices cannot vaccinate unless a court order has been obtained.26,27
Summary
Measles is a potentially fatal disease that is easily preventable—it is tragic that antivaccination sentiment may contribute to a large outbreak and potentially some deaths. Clinicians need to be able to recognise measles, treat the patient in front of them, inform public health, and encourage vaccination to prevent future outbreaks.