
Although they are more commonly associated with causing disease and, at times, devastating pandemics, viruses have also played an important role in human evolution – and without them you wouldn’t be here at all.
The Mabuya lizards that live in the Andes mountains of Colombia are not like other reptiles. While the majority of reptiles lay eggs with hard shells, some Mabuya species give birth to live young. Crucially, the mothers have placentas: specialised organs for feeding the developing young inside their bodies.
Placentas are more commonly associated with mammals like mice and humans: we are placental mammals. But other kinds of animal have also evolved placentas. And in 2001 zoologists Martha Patricia Ramírez-Pinilla and Adriana Jerez of the Industrial University of Santander in Bucaramanga, Colombia, revealed that Mabuya lizards have extremely advanced placentas, not too dissimilar from ours.
While this was surprising enough for a reptile, which typically lay leathery eggs, the real revelation came 16 years later, when Ramírez-Pinilla teamed up with geneticist Thierry Heidmann of Gustave Roussy in Paris, France and his colleagues. They found that the lizards have a gene that is essential for the formation of the placenta, and that gene came from a virus.
Within the last 25 million years, the ancestors of the lizards were infected by a virus that incorporated some of its own DNA into their genome. But instead of being harmed, the lizards somehow co-opted the viral DNA and used it to develop their first placentas. Thanks to the virus, the lizards evolved a new organ.
“The genomic acquisition coincided with the shift from non-placental to placental lizard,” says Heidmann.
The unusual thing about this story, however, is that it is not unusual. About a tenth of the human genome comes from viruses, and that viral DNA has played crucial roles in our evolution. Some of it was the source of the mammalian placenta. Other bits are involved in our immune response against disease and in the formation of new genes. Without viruses, humans could not have evolved.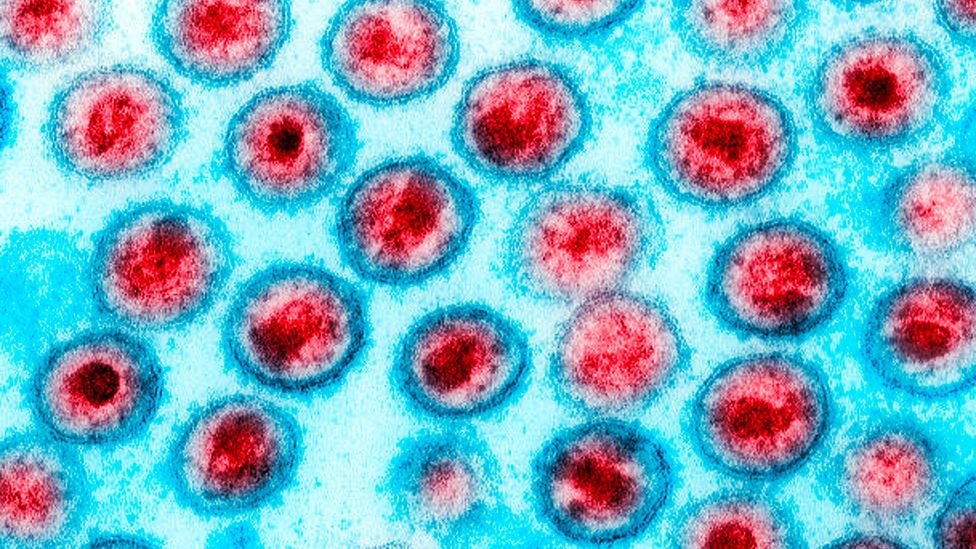
There are four known retroviruses that infect humans, including HIV-1 – viruses like this have helped to shape our evolution
Viruses are so simple that many biologists do not regard them as fully alive. Each virus is essentially a microscopic package of genetic material. They can only reproduce by infecting living cells: they subvert the cell’s machinery to make copies of themselves. In doing so they often make their hosts ill.
Viruses that insert their own genetic material into the host’s genome are called retroviruses. Their nature was first understood in the 1960s and 1970s, although some had been isolated decades before. Following a suggestion in 1964 that some viruses might copy their own genetic material into the DNA of their hosts, researchers identified DNA of viral origin in the genomes of chickens.
Despite being a large and diverse group of viruses, only four retroviruses are currently known to infect humans. All were discovered in the 1980s: human T-lymphotropic virus 1 (HTLV-1), which causes a form of cancer, along with the closely related HTLV-2; and human immunodeficiency virus (HIV) types 1 and 2, which cause Aids.
If a retrovirus infects a cell in a person’s lungs or skin, that may be bad news for the person, but it has limited consequences for our species’ evolution as this DNA is not passed onto the next generation. However, sometimes a retrovirus gets into the germline: the cells that give rise to eggs and sperm, where viral DNA can be passed onto our offspring. These pieces of viral DNA are called endogenous retroviruses or ERVs. It is these heritable bits of viral DNA that can change the course of evolution.
ERVs everywhere
The sheer scale of human ERVs was revealed when the first draft of the human genome was published in 2001. “It turned out there was a huge amount of viral sequence,” says Heidmann. About 8% of the human genome consists of ERVs.
Some of them are truly ancient. One study in 2013 identified an ERV on the human chromosome 17 that is at least 104 million years old and probably older. That means it is the result of a virus infecting a mammal deep in the era when dinosaurs ruled the Earth. The ERV is only found in mammals with placentas, so it may have integrated soon after placental mammals split from their marsupial cousins
ERVs aren’t confined to mammals and reptiles, either. “All vertebrates have endogenous retroviruses,” says molecular virologist Nicole Grandi at the University of Cagliari in Italy.
Most human ERVs are not unique to our species but can also be found in at least some other primates, such as chimpanzees. This means they got into primate genomes millions of years ago, long before our own species evolved, and we then inherited them from our ape ancestors.
Some ERVs help the immune system to target cancerous cells
Curiously, there is no evidence of new ERVs entering the human genome in the last few thousand years. The only retroviruses our species currently has to deal with are HTLV and HIV, says Grandi, and neither has been reported to infect germline cells. “Currently we cannot see active endogenisation in humans,” says Grandi.
This is in stark contrast to some other species. Koalas are currently being invaded by koala retrovirus (KoRV), DNA from which is found in some populations of koalas but not others. Koala geneticists are therefore able to watch “a genome invasion in real time“.
Origin of the placenta
Human ERVs were originally thought of as inactive “fossil sequences” or part of the genome’s “junk DNA”. However, in common with a lot of supposed junk DNA, it turns out that many human ERVs are active. (Learn about the crucial role junk DNA may play in this article by David Cox.)
The most studied ERVs in the human genome are called HERV-W, first described in 1999. They encode proteins called syncytins, which are found in the placenta. Just like in the Mabuya lizards, these viral genes are essential for the placenta to form.
This link between viruses and the placenta makes sense when you consider what syncytins actually do. These proteins have the ability to fuse two or more cells into one. When they were viral proteins, they were used by the virus to fuse with the outer membrane of a cell and thus infect it. This fusion ability has been co-opted by the placenta. By fusing cells from the mother and cells from the embryo, the placenta can transfer nutrients to the embryo and extract wastes.
And it’s not just humans. Similar syncytin proteins are found in other apes like gorillas. More recent studies have shown that retroviruses have infected mammals repeatedly throughout their evolutionary history, so different groups of mammals often have different syncytins derived from different retroviruses.
“We hypothesise that in fact there was a founding ERV capture 150 million years ago, which led to the emergence of placental mammals,” says Heidmann. Since then, repeated infections seem to have overwritten that original ERV, so it cannot be found in any living mammal. The Mabuya lizard study was important because it demonstrated that the lizards only acquired placentas after first acquiring the ERV from a virus – suggesting the same thing happened in the ancestor of all placental mammals. “It gave the demonstration of the link between acquisition of a placenta and acquisition of a syncytin,” says Heidmann.
A few koala populations, such as those on Kangaroo Island, a free of the koala retrovirus while others are being invaded by the disease
Beyond the Genome
It has been 20 years since the Human Genome Project was “completed”, but this enormous effort to sequence and map the human “book of life” was only just the beginning. Far from closing the question of what makes our bodies tick and why they do so differently, research on the human genome has revealed a far more complex picture than anyone could have imagined. Beyond the Genome examines just how far our understanding of our genetics has come in the past two decades.
The story of syncytins and the placenta is one of the most dramatic examples of viral DNA affecting evolution. It is particularly noteworthy because a complete viral gene has survived in the human genome and encodes a protein. Many other ERVs do not encode proteins, but they still have functions.
Some play a role in stem cells: the multipurpose cells found in developing embryos. Some stem cells are pluripotent, meaning they can develop into any type of cell in the body, from neurons to muscle fibres.
A family of retroviruses called HERV-H are essential for pluripotency. However, they do not code for proteins. Instead, the HERV-H sequences are copied onto molecules called RNAs, and these keep the cell pluripotent. “If they are suppressed, then the cell morphology changes and it loses the ability to maintain its undifferentiated state,” says virologist Christine Kozak of the National Institute of Allergy and Infectious Diseases in Bethesda, Maryland.
Other ERVs regulate the activity of genes, and therefore control bodily processes. For example, our bodies use an enzyme called amylase to break down carbohydrates like starch in our food. “We have amylase in the pancreas and we have amylase in the mouth in the saliva,” says Grandi. The amylase gene is activated in the salivary gland by a DNA sequence called a promoter – which comes from an ERV.
The viruses that keep us healthy
Unsurprisingly, given that ERVs come from viruses, many scientists are interested in their role in health and disease. One such example was described in 2022 by researchers led by Cédric Feschotte, a molecular biologist and geneticist at Cornell University in Ithaca, New York. The team was trying to find an instance in humans of a phenomenon already well-known in other animals – sometimes, ERV genes code for proteins that can be co-opted by the immune system and used to fight off other viruses. The target viruses can be closely related to the virus that gave rise to the ERV in the first place, or only distantly related. Feschotte says antiviral proteins from ERVs have been studied in mice, chickens and cats. “But to my knowledge there was no examples of that in the human genome,” he says.
https://emp.bbc.com/emp/SMPj/2.51.0/iframe.html
Could ancient viruses emerge once again?
The team scanned the known ERVs in the human genome and identified hundreds of sequences that could potentially encode antiviral proteins. Then they zeroed in on one gene called Suppressyn, which encodes a protein similar to those that make up the outer envelopes of viruses. The Suppressyn protein blocks retroviruses from entering cells, because it binds to receptors on the cell outer membrane that the viruses would themselves use to get into the cell. Feschotte compares it to inserting a broken key into a lock, preventing anyone from unlocking the door.
Suppressyn is mostly found in the placenta and developing embryo. This suggests its original use was to prevent retroviruses from infecting embryos, which have very weak immune systems. “It’s protective of the germline rather than of the organism as a whole,” says Feschotte.
But he believes that ERVs probably do a lot more in our immune system. “We have 1,500 candidates,” he says. “That’s a lot of genes.” While many geneticists still think of ERVs as inert or defective, that’s misleading. “They are decaying but they still make RNA and they still make a lot of proteins,” says Feschotte. “We need to take a good look at that.” And the picture is still emerging – a study published in April 2023 found that some ERVs help the immune system to target cancerous cells.
Do ERVs make us ill?
But while they can protect us from disease, it would not be surprising if some ERVs might also be responsible for producing negative health affects in humans too. “There’s really a lot of interest right now in the possibility that human ERVs can be associated with disease,” says Kozak. “At this point there’s a lot of suggestive evidence but no smoking gun.”
Humans are truly a mosaic species – around 8% of our genome comes from viruses
For Feschotte, it’s key to think through exactly what the ERVs are doing – and we haven’t always got it right. “Ever since endogenous retroviruses were discovered, people were trying to tie those to cancer,” he says. That’s because the first ones discovered in animals were causing cancer. Funders “poured tonnes of money” at ERV research in the hope that it would uncover mechanisms of cancer and thus potential treatments. “Many people came back empty-handed.”
The key point is that human ERVs are not capable of forming viruses, which could then infect other cells. “In the mouse there is plenty, and in the chicken there is plenty,” says Feschotte. “They cause all kinds of disease.” But human ERVs have been brought under a great level of control by the rest of the genome, so do not cause viral infections.
“It’s a lot more subtle and probably about gene regulation or dysregulation, I think,” says Feschotte. Because ERVs are so widely distributed in the human genome, they can coordinate the activities of multiple genes that are separated by huge expanses of sequence. Many bodily processes need genes to be turned on and off in precise sequences, and ERVs play a big role in controlling that. “Now we’re revisiting the role of these things in disease, but through different mechanisms.”
The role of ERVs in disease is shrouded for now. But what is clear is that they are an engine of evolution. By inserting new bits of DNA throughout our genome, viruses have spurred massive changes to our genetic make-up. Once ERVs are in place, they can trigger the duplication or deletion of swathes of DNA – and if the changes are beneficial, they spread. No animal, including humans, would exist in its current form without them.
The final lesson is that humans are truly a mosaic species. Many of us have some DNA, around 2% of our genome, from Neanderthals. Some populations also have some DNA from another extinct hominin group, the Denisovans. And all of us get around 8% of our genome from viruses.
“If you think about the human gene catalogue, it’s kind of almost an existential question,” says Feschotte. Around 20,000 protein-coding genes are known, and a comparable quantity of our DNA comes from viruses. “It’s kind of mind blowing.”