Thermo Fisher Scientific argues that mRNA-based COVID-19 vaccines merely hint at the mRNA-based applications that are already in the works
SPARTA Biodiscovery hopes their invention will play a role in burgeoning field of COVID-19 vaccines, among other technologies using nano-formulations, by helping researchers look at individual particles. [Mirela Gherban/Getty Images]
The unbelievably fast development of the mRNA-based COVID-19 vaccine was a testament to 70 years of diligent research into RNA biology. When this research was put to the sternest test—fighting a global pandemic—it succeeded. COVID-19 vaccines were developed that succeeded in mitigating the risk of severe infection and hospitalization.
However, even at their best, the original COVID-19 vaccines offer limited protection. As a World Health Organization article on these vaccines indicated, they “provide at least some protection from infection and transmission, but not as much as the protection they provide against serious illness and death.” This is why scientists are gearing up for a second generation of better, safer mRNA-based COVID-19 vaccines.
Scientists are also pursuing applications such as mRNA-based vaccines for other infectious diseases such as influenza and respiratory syncytial virus (RSV) disease. Yet other applications include mRNA-based therapeutics for fighting cancer.
Second-generation COVID-19 vaccines
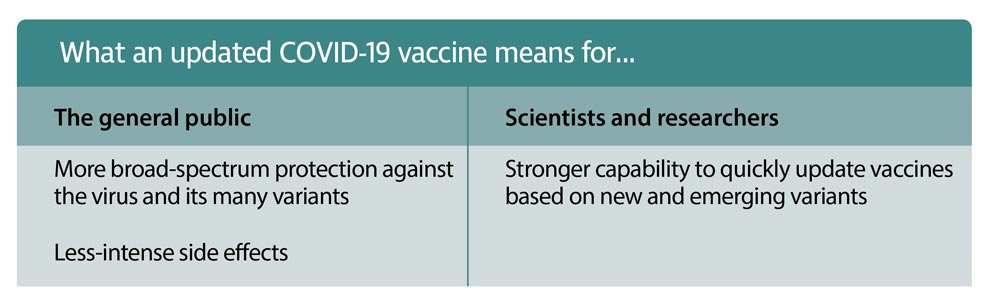
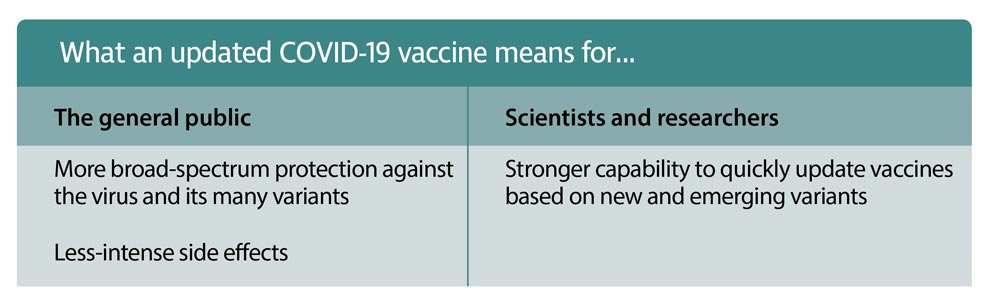
A standout feature of second-generation COVID-19 vaccines is broad-spectrum protection against new and emerging variants (Table). To build vaccines that have this kind of polyvalency, scientists must identify and exploit the common ground that exists across the genomes of all (or most) SARS-CoV-2 variants.
Another kind of polyvalency is to be found in vaccines that span COVID-19 and other infectious diseases. For example, Pfizer and
BioNTech announced a Phase I trial of a combined COVID-19 and influenza vaccine in November 2022. Similarly, Moderna has several mRNA vaccine cocktails in preclinical development: COVID-19/influenza, influenza/RSV, and influenza/RSV/SARS-CoV-2.
On top of the list of improvements is the reduction of vaccine side effects. A contributor to the side effects of COVID-19 vaccines is double-stranded RNA (dsRNA). This undesirable byproduct is formed during in vitro transcription. Because dsRNA is present in most viral infections, it’s inflammatory to the human body.
Removing dsRNA currently involves chromatography purification, a process that is not just expensive, but can also reduce yield and decrease mRNA integrity. Scientists are now searching for a way to reduce and control the appearance of dsRNA, such as using chaotropic agents during in vitro transcription to, in theory, create a suitable environment to prevent dsRNA formation.
Vaccines for influenza and RSV
Influenza and RSV disease have persisted among humans for thousands of years and continue to be burdens on immunocompromised populations, such as children and the elderly. Influenza is particularly challenging. There are myriad variants and seasonal mutations that put a strain on vaccine efforts. The problem partially stems from current vaccine development methods, which utilize dead or inactivated forms of the virus that, when injected, stimulate an immune response to fight the disease.
Since there are yearly variants and seasonal mutations to consider, it can be difficult for vaccine researchers to predict what strain will be most prevalent for an upcoming flu season. If their predictions are wrong, the vaccine will not provide optimal protection.
Other notable challenges posed by traditional flu vaccine methods are production time frames and manufacturing limitations. The time between choosing a vaccine strain and developing/delivering that vaccine is short—so short, in fact, that it cannot accommodate unexpected delays.
Fortunately, mRNA-based vaccines can solve these issues. As in the development of mRNA-based COVID-19 vaccines, the development of mRNA-based flu vaccines involves searching the genomes of disease-causing strains to identify commonalities that can be harnessed to stimulate an immune response. Ultimately, scientists can create a “universal” vaccine that protects against several strains at once and is better at keeping up with emerging variants.
This kind of development has helped Moderna and Pfizer initiate clinical trials for novel mRNA flu vaccines. Moderna is now conducting two Phase III trials of an mRNA-based flu vaccine called mRNA-1010. Pfizer is developing a quadrivalent flu vaccine based on a nucleoside-modified mRNA, or modRNA, called qIRV.
Advances in mRNA technology are also enabling the development of vaccines that can protect against illnesses that have never had a vaccine. One such illness is RSV disease, which evaded vaccine development and protective measures for decades. A disastrous vaccine clinical trial in the 1960s led to the deaths of two children and a number of hospitalizations. Besides having a fraught history, RSV vaccines have struggled to target RSV’s fusion (F) glycoprotein, which is notoriously complicated.
With emergent mRNA technology surrounding COVID-19, targeting RSV’s tricky F glycoprotein has become easier. Because of this, Moderna has entered into a Phase III clinical trial for its RSV vaccine, mRNA-1345. It is encapsulated by the same lipid nanoparticles that encapsulate Moderna’s COVID-19 vaccines, and it targets the prefusion F glycoprotein of both RSV-A and RSV-B subtypes.
Anticancer drugs based on mRNA
Besides improving the prevention and treatment of infectious diseases, mRNA technology is proving useful in fighting certain cancers. However, it is undoubtedly more complicated to create a cancer vaccine than a flu vaccine because cancer presents differently in different patients, even if they have the same type of cancer.
Luckily, success is on the horizon. Moderna has created an experimental cancer vaccine that relies on mRNA to fight melanoma. More specifically, when combined with Merck & Co.’s renowned immunotherapy, Keytruda, this cancer vaccine reduced the risk of recurrence or death in patients with stage III/IV melanoma by 44% compared with Keytruda alone, according to results from the Phase IIb KEYNOTE-942 trial.
In this study, each administered mRNA vaccine was first tailor-made to the patients’ tumors. Samples of the tumor and healthy tissue were analyzed to decode their genetic sequences so that scientists could identify mutant proteins associated with the cancer. That crucial information was then used to create a vaccine for that specific patient, all in eight weeks.
After injection, the vaccine spurred an immune response causing the body to produce exact copies of the mutant proteins for the immune system to recognize and destroy. While this breakthrough applies only to melanoma, the same approach is being studied for other highly mutated cancers like lung, pancreatic, and bladder cancer, as well as some breast cancers.
The success of this trial is not just monumental, it’s also opening new doors to use mRNA therapeutics to treat other complex diseases such as multiple sclerosis, muscular dystrophy, and cystic fibrosis.
At present, we have little to no viable treatment options for these conditions because they are genetic. Those who suffer from these diseases typically have some deficiency or mutation in a key protein responsible for an important biological function. An mRNA-based therapeutic that is persistent and codes for the defective or missing protein(s) can correct the patient’s condition or, at the very least, improve it greatly. The mRNA therapeutic would instruct patient cells to produce the missing or defective protein.
Unlike gene therapy, mRNA-based therapies don’t permanently alter a patient’s DNA. That makes mRNA a safer alternative, avoiding potential side effects that are typical of gene therapies. Additionally, the fact that mRNA does not alter a person’s DNA may help patients overcome any hesitancy toward taking mRNA-based therapeutics.
We’re already seeing mRNA innovations on the horizon. Scientists are discovering how to make mRNA vaccines safer and more efficient. They are creating even more mRNA vaccines that protect us from life-threatening diseases, and they are exploring the development of mRNA therapeutics. Because of these advancements, it won’t be long until mRNA technology is broadly accessible worldwide.
SPARTA Biodiscovery hopes their invention will play a role in burgeoning field of COVID-19 vaccines, among other technologies using nano-formulations, by helping researchers look at individual particles. [Mirela Gherban/Getty Images]
The unbelievably fast development of the mRNA-based COVID-19 vaccine was a testament to 70 years of diligent research into RNA biology. When this research was put to the sternest test—fighting a global pandemic—it succeeded. COVID-19 vaccines were developed that succeeded in mitigating the risk of severe infection and hospitalization.
However, even at their best, the original COVID-19 vaccines offer limited protection. As a World Health Organization article on these vaccines indicated, they “provide at least some protection from infection and transmission, but not as much as the protection they provide against serious illness and death.” This is why scientists are gearing up for a second generation of better, safer mRNA-based COVID-19 vaccines.
Scientists are also pursuing applications such as mRNA-based vaccines for other infectious diseases such as influenza and respiratory syncytial virus (RSV) disease. Yet other applications include mRNA-based therapeutics for fighting cancer.
Second-generation COVID-19 vaccines
A standout feature of second-generation COVID-19 vaccines is broad-spectrum protection against new and emerging variants (Table). To build vaccines that have this kind of polyvalency, scientists must identify and exploit the common ground that exists across the genomes of all (or most) SARS-CoV-2 variants.
Another kind of polyvalency is to be found in vaccines that span COVID-19 and other infectious diseases. For example, Pfizer and
BioNTech announced a Phase I trial of a combined COVID-19 and influenza vaccine in November 2022. Similarly, Moderna has several mRNA vaccine cocktails in preclinical development: COVID-19/influenza, influenza/RSV, and influenza/RSV/SARS-CoV-2.
On top of the list of improvements is the reduction of vaccine side effects. A contributor to the side effects of COVID-19 vaccines is double-stranded RNA (dsRNA). This undesirable byproduct is formed during in vitro transcription. Because dsRNA is present in most viral infections, it’s inflammatory to the human body.
Removing dsRNA currently involves chromatography purification, a process that is not just expensive, but can also reduce yield and decrease mRNA integrity. Scientists are now searching for a way to reduce and control the appearance of dsRNA, such as using chaotropic agents during in vitro transcription to, in theory, create a suitable environment to prevent dsRNA formation.
Vaccines for influenza and RSV
Influenza and RSV disease have persisted among humans for thousands of years and continue to be burdens on immunocompromised populations, such as children and the elderly. Influenza is particularly challenging. There are myriad variants and seasonal mutations that put a strain on vaccine efforts. The problem partially stems from current vaccine development methods, which utilize dead or inactivated forms of the virus that, when injected, stimulate an immune response to fight the disease.
Since there are yearly variants and seasonal mutations to consider, it can be difficult for vaccine researchers to predict what strain will be most prevalent for an upcoming flu season. If their predictions are wrong, the vaccine will not provide optimal protection.
Other notable challenges posed by traditional flu vaccine methods are production time frames and manufacturing limitations. The time between choosing a vaccine strain and developing/delivering that vaccine is short—so short, in fact, that it cannot accommodate unexpected delays.
Fortunately, mRNA-based vaccines can solve these issues. As in the development of mRNA-based COVID-19 vaccines, the development of mRNA-based flu vaccines involves searching the genomes of disease-causing strains to identify commonalities that can be harnessed to stimulate an immune response. Ultimately, scientists can create a “universal” vaccine that protects against several strains at once and is better at keeping up with emerging variants.
This kind of development has helped Moderna and Pfizer initiate clinical trials for novel mRNA flu vaccines. Moderna is now conducting two Phase III trials of an mRNA-based flu vaccine called mRNA-1010. Pfizer is developing a quadrivalent flu vaccine based on a nucleoside-modified mRNA, or modRNA, called qIRV.
Advances in mRNA technology are also enabling the development of vaccines that can protect against illnesses that have never had a vaccine. One such illness is RSV disease, which evaded vaccine development and protective measures for decades. A disastrous vaccine clinical trial in the 1960s led to the deaths of two children and a number of hospitalizations. Besides having a fraught history, RSV vaccines have struggled to target RSV’s fusion (F) glycoprotein, which is notoriously complicated.
With emergent mRNA technology surrounding COVID-19, targeting RSV’s tricky F glycoprotein has become easier. Because of this, Moderna has entered into a Phase III clinical trial for its RSV vaccine, mRNA-1345. It is encapsulated by the same lipid nanoparticles that encapsulate Moderna’s COVID-19 vaccines, and it targets the prefusion F glycoprotein of both RSV-A and RSV-B subtypes.
Anticancer drugs based on mRNA
Besides improving the prevention and treatment of infectious diseases, mRNA technology is proving useful in fighting certain cancers. However, it is undoubtedly more complicated to create a cancer vaccine than a flu vaccine because cancer presents differently in different patients, even if they have the same type of cancer.
Luckily, success is on the horizon. Moderna has created an experimental cancer vaccine that relies on mRNA to fight melanoma. More specifically, when combined with Merck & Co.’s renowned immunotherapy, Keytruda, this cancer vaccine reduced the risk of recurrence or death in patients with stage III/IV melanoma by 44% compared with Keytruda alone, according to results from the Phase IIb KEYNOTE-942 trial.
In this study, each administered mRNA vaccine was first tailor-made to the patients’ tumors. Samples of the tumor and healthy tissue were analyzed to decode their genetic sequences so that scientists could identify mutant proteins associated with the cancer. That crucial information was then used to create a vaccine for that specific patient, all in eight weeks.
After injection, the vaccine spurred an immune response causing the body to produce exact copies of the mutant proteins for the immune system to recognize and destroy. While this breakthrough applies only to melanoma, the same approach is being studied for other highly mutated cancers like lung, pancreatic, and bladder cancer, as well as some breast cancers.
The success of this trial is not just monumental, it’s also opening new doors to use mRNA therapeutics to treat other complex diseases such as multiple sclerosis, muscular dystrophy, and cystic fibrosis.
At present, we have little to no viable treatment options for these conditions because they are genetic. Those who suffer from these diseases typically have some deficiency or mutation in a key protein responsible for an important biological function. An mRNA-based therapeutic that is persistent and codes for the defective or missing protein(s) can correct the patient’s condition or, at the very least, improve it greatly. The mRNA therapeutic would instruct patient cells to produce the missing or defective protein.
Unlike gene therapy, mRNA-based therapies don’t permanently alter a patient’s DNA. That makes mRNA a safer alternative, avoiding potential side effects that are typical of gene therapies. Additionally, the fact that mRNA does not alter a person’s DNA may help patients overcome any hesitancy toward taking mRNA-based therapeutics.
We’re already seeing mRNA innovations on the horizon. Scientists are discovering how to make mRNA vaccines safer and more efficient. They are creating even more mRNA vaccines that protect us from life-threatening diseases, and they are exploring the development of mRNA therapeutics. Because of these advancements, it won’t be long until mRNA technology is broadly accessible worldwide.