Updated results from a large clinical trial confirm that, for some people with bladder cancer that can be removed with surgery, receiving immunotherapy immediately afterwards is an effective treatment.
In 2021, initial results from the same trial led the Food and Drug Administration (FDA) to approve the immune checkpoint inhibitor nivolumab (Opdivo) as a post-surgical (adjuvant) treatment for people with what is called high-risk bladder cancer.
That approval was based on data showing that, compared with treatment with a placebo, giving nivolumab for a year after surgery doubled the amount of time people lived without their disease recurring in or near the bladder or elsewhere in the body, a measure called disease-free survival.
The updated results, presented on February 17 at the 2023 American Society of Clinical Oncology (ASCO) Genitourinary Cancers Symposium, included about 3 years of follow up. These results showed that people who received nivolumab had a median disease-free survival of 22 monthsExit Disclaimer, compared with about 11 months for those who received a placebo.
The picture looked even better for people whose tumors express a protein called PD-L1, which interacts with another protein targeted by nivolumab. That group of patients had a median disease-free survival of more than 52 months.
In the trial, nivolumab was given for a maximum of 1 year, said Matt Galsky, M.D., from the Icahn School of Medicine at Mt. Sinai, who presented the updated results at the ASCO symposium.
“If you’re just suppressing cancer with a treatment, then potentially, once treatment stops, the cancer starts to grow again,” he said. The long-term survival free of disease seen in some of the study participants “might indicate that [immunotherapy] is actually eradicating the cancer in some patients.”
A lingering risk of recurrence
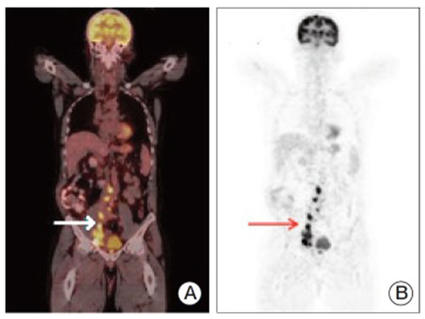
Bladder cancer that has invaded the bladder muscle or nearby lymph nodes can potentially be cured by surgical removal of the bladder and lymph nodes. But, in more than half of people who have this type of surgery, called radical cystectomy, cancer cells have already spread (metastasized) elsewhere in the body.
These deposits of metastatic cancer “are too small to be seen on [an imaging] scan,” said Dr. Galsky. “But over time those cancer cells grow and divide. And we want to try and avoid that if possible,” he explained.
The main strategy that clinical trials have tested to prevent bladder cancer from recurring, either at or near the original tumor or at distant locations, has been adjuvant therapy: chemotherapy or immunotherapy drugs given after surgery.
Chemotherapy regimens based on the drug cisplatin are known to shrink tumors in people with bladder cancer that has metastasized at the time it’s diagnosed, explained Andrea Apolo, M.D., of the Genitourinary Malignancies Branch in NCI’s Center for Cancer Research. So these regimens are often used in bladder cancer that can be surgically removed, either before surgery (called neoadjuvant therapy) or afterward, as adjuvant therapy.
But many people can’t tolerate cisplatin, she added. “And a lot of people prefer not to get chemotherapy because of the side effects,” she said.
Researchers have been searching for other adjuvant therapy options. A previous clinical trial tested a different immunotherapy called atezolizumab (Tecentriq) as an adjuvant therapy, but it did not improve disease-free survival.
So for many years, explained Dr. Galsky, most people, following surgery for bladder cancer, underwent observation instead of adjuvant therapy. Observation is following patients with frequent imaging to try to catch a recurrence as early as possible.
But when a previous study found that nivolumab could shrink tumors in people with more advanced bladder cancer, researchers decided to test the drug as an adjuvant treatment in people without detectable metastases.
Preventing disease recurrence for years
The CheckMate 274 trial, which was funded by Bristol Myers Squibb and Ono Pharmaceutical, enrolled more than 700 people with high-risk, muscle-invasive bladder cancer who had undergone extensive surgery. Participants were eligible if they had received neoadjuvant cisplatin-based chemotherapy but not if they had received any adjuvant treatment.
The researchers randomly assigned trial participants to receive up to a year of treatment with either nivolumab or a placebo. At the time of the ASCO presentation, participants had been followed for a minimum of 31 months.
The incidence of side effects observed during the longer follow-up period was about the same as that seen during the initial 6 months of treatment. Around 18% of people who received nivolumab had at least one serious side effect, compared with 7% of those who received the placebo. Three of the 353 people who received nivolumab died of side effects attributed to the drug.
Overall, after a median follow up of 36 months, people who received nivolumab lived about twice as long without their disease progressing than those who received a placebo.
At the time of the initial publication, there was some evidence that people whose tumors expressed PD-L1 were benefitting more from nivolumab than those whose tumors lacked PD-L1. But it was too early to calculate their median disease-free survival.
With the longer follow up, the researchers found that people whose tumors expressed PD-L1 lived more than twice as long without their disease progressing than the group as a whole.
“These results were impressive but not necessarily unexpected, given what we know about that protein and how [it] might relate to sensitivity to [nivolumab],” Dr. Galsky said.
However, he added, “for all patients in the study, there was a benefit from [receiving] immunotherapy.” Under FDA’s approval, nivolumab can be used for anyone with high-risk bladder cancer, regardless of whether their tumors express PD-L1.
Pinpointing who needs adjuvant therapy
CheckMate 274 participants will continue to be followed to see if those who received nivolumab live longer, a measure called overall survival.
The overall survival data will matter, explained Dr. Apolo. “We know we overtreat a lot of patients with adjuvant therapy,” she said. That is, many people who receive it may have been cured with surgery alone. “But we don’t know yet how to pinpoint who those people are.”
If it turns out that there’s no overall survival improvement from adjuvant immunotherapy, it would make more sense to wait until a cancer recurs or metastasizes to give it, she explained.
A planned NCI-supported trial will soon be looking at whether blood tests for circulating tumor DNA could predict which high-risk patients having surgery for bladder cancer actually need adjuvant therapy and who could safely skip it, Dr. Galsky said.
Although CheckMate 274 didn’t find that treatment with nivolumab decreased participants’ overall quality of life, those who received the drug did experience more side effects and the treatment caused several deaths. “So, if we can identify patients who absolutely don’t need treatment, that certainly makes sense,” said Dr. Galsky.
Other immunotherapy drugs are also being tested as adjuvant treatments for patients with high-risk bladder cancer, Dr. Apolo said. For example, NCI researchers recently finished treating participants in a trial called AMBASSADOR, which is comparing pembrolizumab (Keytruda) with observation after surgery.
In the future, researchers are also interested in testing whether giving nivolumab both before and after surgery can reduce the risk of recurrence even further, Dr. Galsky explained. A recent study found that giving pembrolizumab both before and after surgery reduced the risk of recurrence for some people with melanoma, an aggressive type of skin cancer.
“We’ll see if we see the same thing with bladder cancer,” Dr. Galsky said.