One Piece of the Puzzle
1/13
Your body shape can say quite a bit about your health. But it’s important to remember that it’s just one factor. People of all shapes and sizes can be healthy — or at risk for problems like heart disease or diabetes. You should see your doctor for regular checkups to test your blood pressure, cholesterol, and other measures of your health.

Ectomorph
2/13
One system separates body shapes into “somatotypes.” The ectomorph type has a narrower frame, thinner bones, and smaller joints, and may be flatter in the chest and butt. Think of the typical build of a distance runner, fashion model, or ballerina. Though you may look skinny and find it hard to put on weight, you can have more body fat than you think, especially as you age. That’s because your body often processes food quickly, which makes it harder to build muscle.

Endomorph
3/13
This somatotype usually has more body fat and muscle, smaller shoulders, shorter limbs, and larger bone structure. Think of football linemen, shot put throwers, or curvier women. You may gain weight easily, especially in your lower belly and hips, and find it harder to lose. This may be in part because your body is more likely to store “high carb” foods as fat instead of burning them.

Mesomorph
4/13
This somatotype has an athletic, strong build with wide shoulders, a narrow waist, and low body fat. Think of the typical build of sprinters or soccer players. Because you’re naturally strong and lose and gain weight easily, your body type is well-suited to muscle-building activities like bodybuilding.

Pear Shape
5/13
It combines a slimmer “ectomorph” upper body with an “endomorph” lower body. People with this shape have extra fat in the hip and thigh area. It’s more common among women, and it may be part of the reason they often live longer than men. That could be because belly fat, more common in men, is linked to more health problems than lower-body fat. One study found that in some cases fat in the hips and thighs was linked to lower odds for some diseases.

Apple Shape
6/13
Also called a “beer belly,” it means you have more fat stored around your stomach, while your lower body stays thin. It’s more common in men, and it’s worse for your health than the pear shape. That’s because belly fat is often a sign that you have more fat deeper inside, around your internal organs, as opposed to just beneath the skin. That kind is more closely linked to heart disease, cancer, type 2 diabetes, and high cholesterol.
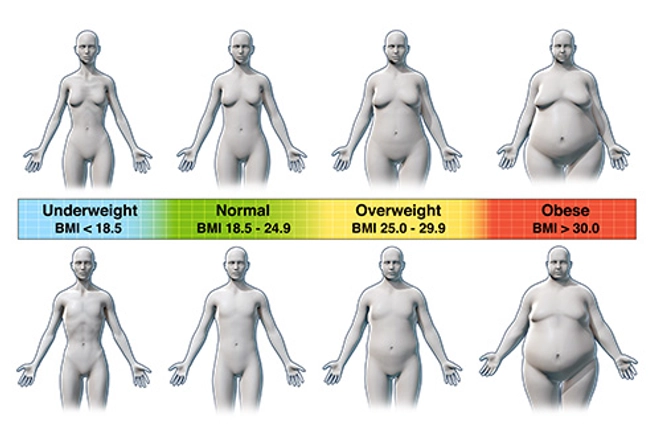
Body Mass Index (BMI)
7/13
Doctors don’t rely on body shape alone to know how healthy you are. They use a few tools to measure how much body fat you have, and BMI is one of them. It’s a number calculated from your height and weight. A score of 25 or more suggests you’re overweight; 30 or more points to obesity. But it doesn’t measure body fat directly or tell you where in your body the fat tends to live.

Waist Size
8/13
This is a simple way to measure how much fat you have around your belly, which can tell you your odds for health problems, like heart disease and type 2 diabetes. To check yours, line up a measuring tape with your belly button and wind it once around. (Don’t suck in your stomach when you measure.) In women, 35 inches or more is a sign of too much belly fat. In men, it’s 40 inches. These numbers may vary slightly if you have a very large body size.

Waist-to-Hip Ratio
9/13
It’s another way to gauge the fat around your midsection. Measure your waist just above your belly button and divide that by the measure of your hips at their widest point. Anything greater than 0.85 for women or 0.9 for men puts you in the danger zone for health problems. Is it a better measure than just your waist size? The research isn’t clear. But many studies suggest that both do a good job of predicting health risks.

Bigger Thighs, Better Health?
10/13
Scientists studied about 3,000 adults for more than 12 years and found those whose thighs measured less than 24 1/2 inches were more likely to have heart disease and other health problems. And the problem got worse as thighs got thinner. However, the study didn’t track whether the people’s thighs were larger because of fat, muscle, or both, so it’s hard to tell why they were better off.

Arm Yourself
11/13
When doctors kept track of 4,000 men between ages 60 and 79 to figure out their body composition, they found that along with slimmer waists, bigger arms seemed to predict longer life and better health. Those who had larger mid-arm muscle measurements lived longer. It may simply be that muscular arms reflect a healthier lifestyle, but the muscle itself may also help.

Exercise to Stay in Shape
12/13
Often, your body shape is something you’re born with. But no matter what you look like, there are lots of things you can do to be healthy. Exercise can help you get rid of deeper fat and build muscle, even if your weight stays the same. And if you lose weight, regular workouts can help you keep it off. Try to get at least 30 minutes of moderate exercise on most days of the week. Building muscle with weights or yoga can also help.

Eat for a Healthy Body Shape
13/13
Trans fats and sweetened foods and drinks seem to boost belly fat. Eat a diet focused on vegetables, fruits, and whole grains. And look for lean protein like skinless chicken, fish, eggs, beans, and low-fat dairy.



