Key Points
Question Can immune checkpoint therapy treat high-risk oral precancerous disease to prevent progression to oral squamous carcinoma?
Findings This phase 2 nonrandomized controlled trial treated 33 patients with high-risk oral proliferative verrucous leukoplakia with the programmed cell death 1 protein inhibitor nivolumab and demonstrated variable lesion regression by size and degree of dysplasia in response to therapy, while 27% of patients developed invasive oral cancer after nivolumab. All whole-exome sequenced patients who progressed to develop cancer had 9p21.3 chromosomal loss.
Meaning Nivolumab showed potential clinical activity in this immune checkpoint therapy trial for high-risk oral precancerous disease; future trials should prioritize cancer-free survival end points and biomarker stratification.
Abstract
Importance Proliferative verrucous leukoplakia (PVL) is an aggressive oral precancerous disease characterized by a high risk of transformation to invasive oral squamous cell carcinoma (OSCC), and no therapies have been shown to affect its natural history. A recent study of the PVL immune landscape revealed a cytotoxic T-cell–rich microenvironment, providing strong rationale to investigate immune checkpoint therapy.
Objective To determine the safety and clinical activity of anti–programmed cell death 1 protein (PD-1) therapy to treat high-risk PVL.
Design, Setting, and Participants This nonrandomized, open-label, phase 2 clinical trial was conducted from January 2019 to December 2021 at a single academic medical center; median (range) follow-up was 21.1 (5.4-43.6) months. Participants were a population-based sample of patients with PVL (multifocal, contiguous, or a single lesion ≥4 cm with any degree of dysplasia).
Intervention Patients underwent pretreatment biopsy (1-3 sites) and then received 4 doses of nivolumab (480 mg intravenously) every 28 days, followed by rebiopsy and intraoral photographs at each visit.
Main Outcomes and Measures The primary end point was the change in composite score (size and degree of dysplasia) from before to after treatment (major response [MR]: >80% decrease in score; partial response: 40%-80% decrease). Secondary analyses included immune-related adverse events, cancer-free survival (CFS), PD-1 ligand 1 (PD-L1) expression, 9p21.3 deletion, and other exploratory immunologic and genomic associations of response.
Results A total of 33 patients were enrolled (median [range] age, 63 [32-80] years; 18 [55%] were female), including 8 (24%) with previously resected early-stage OSCC. Twelve patients (36%) (95% CI, 20.4%-54.8%) had a response by composite score (3 MRs [9%]), 4 had progressive disease (>10% composite score increase, or cancer). Nine patients (27%) developed OSCC during the trial, with a 2-year CFS of 73% (95% CI, 53%-86%). Two patients (6%) discontinued because of toxic effects; 7 (21%) experienced grade 3 to 4 immune-related adverse events. PD-L1 combined positive scores were not associated with response or CFS. Of 20 whole-exome sequenced patients, all 6 patients who had progression to OSCC after nivolumab treatment exhibited 9p21.3 somatic copy-number loss on pretreatment biopsy, while only 4 of the 14 patients (29%) who did not develop OSCC had 9p21.3 loss.
Conclusions and Relevance This immune checkpoint therapy precancer nonrandomized clinical trial met its prespecified response end point, suggesting potential clinical activity for nivolumab in high-risk PVL. Findings identified immunogenomic associations to inform future trials in this precancerous disease with unmet medical need that has been difficult.
Introduction
Oral leukoplakia refers to a white plaque of variable cancer risk, having excluded other conditions, and affects up to 5% of the global population,1 but only a small proportion of leukoplakia lesions will undergo malignant transformation.2 Degree of epithelial dysplasia, lesion size, and tobacco history all influence the transformation rate.3 Proliferative verrucous leukoplakia (PVL) defines an aggressive subtype with a malignant transformation rate exceeding 10% per year, characterized by heterogeneous or verrucous lesions involving multiple oral subsites.4–6 To date, no therapies have been shown to change the natural history of this severe oral precancerous disease,7–9 reflecting a critical unmet medical need.
Studies of the immune landscape led to pivotal trials of anti–programmed cell death 1 protein (PD-1) therapy in recurrent/metastatic head and neck squamous cell carcinoma.10–13 Our prior retrospective study revealed a cytotoxic T-cell–rich immune microenvironment in PVL.14 These findings together with immunosurveillance studies in the context of lung premalignancy and of various immune-oncology interventions in preclinical models15–18 provided strong rationale for investigating PD-1/PD-1 ligand 1 (PD-L1) axis blockade in oral precancerous disease. Here we report the first (to our knowledge) trial to evaluate the safety and clinical activity of preventive anti–PD-1 therapy among patients with high-risk PVL.
Methods
Study Population
This was an open-label, single-group phase 2 trial conducted at the Dana-Farber Cancer Institute in Boston, Massachusetts (trial protocol in Supplement 1). Patients with high-risk oral leukoplakia defined by any of the following criteria were eligible: PVL with multifocal (≥2), contiguous 3 cm or greater, or a single lesion 4 cm or greater in largest diameter (2-3-4 rule) with epithelial dysplasia (any degree); PVL with 4-quadrant oral cavity involvement; at least 1 localized leukoplakia with moderate dysplasia, or erythroleukoplakia for which surgery was indicated but not feasible or the patient refused. Patients were 18 years or older and had an Eastern Cooperative Oncology Group performance status of 2 or lower. A history of surgically treated carcinoma in situ (CIS) or early-stage oral squamous cell carcinoma (OSCC) (American Joint Committee on Cancer Staging Manual, eighth edition, stages I or II) was permitted. Participants defined their race and ethnicity by self-identification. This was assessed given the potential for variation in interpreting the results of the study based on a majority of participants from 1 ethnic group and/or race given the epidemiology of the disease and the treatment center’s regional participant demographics. The trial was approved by the Dana-Farber/Harvard Cancer Center institutional review board (18-387), conducted in accordance with the Declaration of Helsinki and Good Clinical Practice Guidelines, and registered nationally (NCT03692325). This study followed the Transparent Reporting of Evaluations With Nonrandomized Designs (TREND) reporting guideline.
Treatment
Following written informed consent, participants received nivolumab (480 mg intravenously) on day 1 of a 28-day cycle for 4 cycles. Immunosuppressive medications and doses of corticosteroids greater than 20-mg prednisone equivalent daily were prohibited unless used for immune-related toxicity management.
Assessments
Three weeks prior to the first dose of nivolumab and at monthly visits, patients underwent digital intraoral color photography to capture all leukoplakia lesions. Bidimensional measurements were obtained from up to 3 target lesions (per patient) as determined by 1 of 5 oral medicine investigators. Screening and posttreatment biopsies were performed by the same oral medicine investigator for consistency. Fresh tissue biopsies from all target lesions were mandatory at baseline and 30 days after the final dose of nivolumab. Pathologic specimens from each biopsy were examined by 2 experienced oral pathologists (V.Y.J. and K.S.W.) blinded to outcome data (or a third in cases of any scoring discrepancy). New or suspicious nontarget lesions or changes in target lesions could trigger rebiopsy at any point.
Response was assessed according to a modified composite scoring system (van der Waal classification)19 (eFigure 1 in Supplement 2). The sum of target lesion point scores (both clinical and pathologic) yielded a composite score. The percent change in composite score before and after treatment determined best overall response. Major response (MR) was a decrease of more than 80%, partial response (PR) a decrease of 40% to 80%, stable disease (SD) was neither an MR or PR, and progression of disease (PD) was defined as an increase of 10% or greater in the composite score or a CIS or OSCC diagnosis. Patients were followed up with clinical examinations every 3 to 4 months until study withdrawal or up to 5 years.
Safety
Safety evaluations included laboratory and adverse event (AE) assessments (National Cancer Institute Common Terminology Criteria for Adverse Events, version 5.0).20 For patients who developed grade 3 or intolerable grade 2 immune-related AEs (irAEs), nivolumab treatment could be interrupted, delayed, or discontinued; certain grade 4 irAEs required discontinuation. AEs were captured up to 3 months after completion of nivolumab treatment.
Statistical Analysis
The primary end point was best overall response (MR + PR rate) as defined by the percent change in clinical-pathologic composite score. A 2-stage Simon optimal design was used. When more than 5 of 33 patients who were eligible and began protocol treatment had disease in response (assuming >1 patient with disease in response among the first 16 patients), there was 84.3% power to rule out a 10% and detect a 25% response rate (using a 1-sided exact binomial test, type I error rate of 10%). A response rate of 25% was targeted when considering the cumulative risk of serious irAEs.21
Secondary end points included safety and cancer-free survival (CFS), defined as the time from trial registration to OSCC or death due to any cause (participants alive without oral cancer were censored at last assessment). Based on studies of PD-L1 expression14,22 and somatic 9p21 copy-number loss in advanced OSCC, lung, and other tumors,23,24 we conducted secondary analyses to evaluate the association of pretreatment dysplastic tissue PD-L1 expression and 9p21.3 deletion status with outcomes. Exploratory analyses included immunogenomic profiling using multiparametric flow cytometry and whole-exome sequencing (WES) detailed in the eMethods in Supplement 2.
The primary clinical activity population included all eligible patients who began protocol treatment. Response rate was summarized as a proportion with a corresponding 2-stage 95% CI. The distribution of CFS was estimated using the Kaplan-Meier method. Logistic regression and Cox proportional hazard models were used to estimate odds ratios (ORs) for best overall response and hazard ratios (HRs) for CFS, respectively. Fisher exact test was used to compare somatic copy-number alterations (SCNAs) and genomic subsets (2-sided). Wilcoxon signed rank test (paired data) and Wilcoxon rank-sum test (independent) were used to analyze both circulating and tissue-based immune profiling parameters (2-sided), using a Bonferroni-Dunn correction for tests of multiple comparisons. Data as of September 30, 2022, were analyzed. Data analysis used R, version 4.3.0 for Windows (R Foundation for Statistical Computing). A 2-sided P ≤ .05 indicates statistical significance.
Results
Between January 10, 2019, and December 13, 2021, the trial enrolled 33 patients. All began protocol treatment and were included in analyses (Figure 1A). Median (range) age was 63 (32-80) years, with a slight majority of female individuals (18 [55%]), and many were smokers (16 [48%]) (Table 1). Eight (24%) had a history of surgically treated early-stage OSCC. Median (range) disease-free interval for those with a head and neck cancer prior to trial entry was 10.5 (0.3-195.0) months. A median of 4 cycles of therapy were received (12% of patients received fewer than all 4 doses).
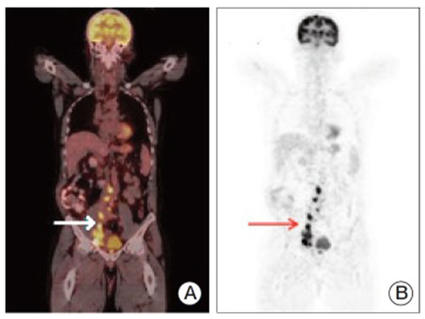
Twelve patients (36%) (95% CI, 20.4%-54.8%) demonstrated a best overall response of MR or PR, with 3 (9%) demonstrating a greater than 80% reduction in composite score (Table 2). Among individual patients, 2 (6%) had complete resolution of at least 1 target lesion. Sixteen (48%) had SD, and 4 patients (12%) had a best response of PD (Figure 1B and D). Three of the patients with a best response of PD developed OSCC in a target lesion identified on their end-of-treatment biopsy, and the other experienced an increase in the severity of dysplasia in a buccal gingiva target lesion resulting in greater than 20% composite score increase. No patient developed CIS. Six additional patients with a best response other than PD later developed OSCC (eTable 1 in Supplement 2); of note, 6 of the 9 who developed OSCC had a history of early-stage OSCC, and 3 of 12 responders (25%) later developed OSCC. Among the 9 patients with an OSCC event, median (range) time from trial registration to a first OSCC event was 6.6 (1.3-24.3) months, and median time from the last dose of nivolumab to the development of OSCC was 3.7 months. Eight of 9 events were in target lesions.
At a median (range) follow-up of 21.1 (5.4-43.6) months, median CFS had not been reached (NR) (95% CI, 24.3 months to NR) with a 2-year CFS of 72.8% (95% CI, 52.6%-85.5%) (Figure 2). There were 9 CFS events (27.3%) and no deaths (all OSCC events). No clinical or pathologic features appeared to be associated with CFS except a history of early-stage OSCC (HR, 13.53; 95% CI, 3.3-55.5) (eTable 2 in Supplement 2). The median CFS for patients with a prior oral cavity cancer diagnosis was 1.3 months (95% CI, 6.2-12.1), and for patients without a history of OSCC, the median was not reached.
Fatigue was the most common AE (18 [55%]), followed by oral pain (11 [33%]) and diarrhea (9 [27%]) (eTable 3 in Supplement 2). Seven patients (21%) developed grade 3 to 4 AEs, which later resolved. One patient without a cardiac history had atypical chest pain after a half-marathon after cycle 1 and had an elevated troponin T level; cardiologic evaluation clarified a low suspicion for immune-related myocarditis, and the patient resumed treatment. Two patients developed immune-related hepatitis. One patient developed immune-related colitis 5 months after completion of therapy.
All pretreatment dysplastic specimens were evaluable for PD-L1 combined positive score (CPS) testing. Scores ranged from 0 to 80 (eFigure 2A and B in Supplement 2), with 22 (67%) demonstrating a CPS of 1 or greater. No significant difference was observed in PD-L1 CPS scores among responders vs nonresponders (12.5 vs 5, P = .21), and patients with CPS 20 or greater vs less than 20 were not significantly more likely to respond (OR, 4.29; 95% CI, 0.83-25.94) (eTable 4 in Supplement 2).
Multiparametric flow on paired dysplastic tissue before and after treatment revealed that CD8+ T cells showed greater activation (CD69) and immune checkpoint LAG3 coexpression after treatment, with increased LAG3 expression among patients with pretreatment 9p21.3 loss of heterozygosity profiles. Among paired peripheral blood samples, PD-1 expression on both circulating CD4+ and CD8+ T cells decreased significantly (both adjusted P < .001), while CD38 increased on CD8+ T cells (adjusted P < .001) (supporting data in eFigure 2C in Supplement 2).
A subset of 23 patients (70%) had adequate tissue for WES. Twenty pairs of paired peripheral blood and oral dysplastic tissue passed quality controls. Pretreatment median (range) tumor mutational burden was 3.4 (1.4-8.0) mutations per megabase and was similar regardless of response (3.6 vs 2.8, P = .63) and among patients who developed cancer vs not (3.9 vs 2.9, P = .51) (Figure 3A). Genomic driver alterations were similar in patients who developed OSCC vs not. Missense mutations in PIK3CA were common. SCNAs revealed a range of complex allelic-imbalance profiles, primarily focal deletions, most frequently observed at 1q44 (Figure 3B). Only 9p21.3 deletion yielded statistically significant differences between patients who developed OSCC and those who did not. Of 10 patients whose pretreatment tissue sequencing showed 9p21.3 copy-number loss, 6 (60%) later developed OSCC, whereas none of the 10 patients without 9p21.3 loss developed OSCC (P = .01).
Discussion
We present the first (to our knowledge) trial demonstrating the potential efficacy of PD-1 immune checkpoint blockade among patients with high-risk oral precancerous disease. Our data suggest that PD-1 inhibition may yield clinical-pathologic regression in some patients. While some chemoprevention trials have yielded short-term responses to reverse or mute oral carcinogenesis, no therapeutic agents have demonstrated an improvement in CFS, and rates of progression to cancer range from 10% to 30%.7–9,25–28
PVL is an uncommon variant of leukoplakia, occurring in less than 1% of adults, which is aggressive and challenging to treat29,30 largely due to nonhomogeneous, multifocal lesions, and with the histologic hallmarks being corrugated hyperkeratosis and verrucous hyperplasia with variable dysplasia.5,31,32 Some degree of dysplasia was required in our trial with the aim of selecting the highest-risk lesions. Our previous retrospective cohort of patients with PVL suggested a 2-year CFS of 82%.14 In the present trial, we observed a 2-year CFS of 73%; however, we designed the trial with stringent entry criteria, requiring biopsy-proven dysplasia and permitting a history of OSCC. Notably, CFS was a secondary end point in our trial, and the sample size and median follow-up time were limited. It is plausible that our preliminary CFS rate would have been similar without immunotherapy exposure, supporting the need for randomized data. Three patients who had a response during the trial later developed OSCC, suggesting that our scoring system and response definitions may not adequately predict CFS. The prognostic impact of tumor size may not be readily generalizable to precancerous lesions, and a 1-tier change in histopathology (degree of dysplasia) may not be an optimal outcome measurement. As compared to prior chemoprevention trials, our rate of progression to cancer (27%) was comparable,7–9,25–28 while response was defined in prior studies primarily based on lesion size and not histologic change.
Of 9 OSCC events, 6 (67%) were among patients with prior early-stage OSCC with a short median time to failure (<4 months). Including patients with prior cancer events added some heterogeneity to the trial population, but we thought it was important to include them given their recurrence risk.33 Exclusion of patients with prior oral cancer has been implemented in some chemoprevention studies,27,28,34,35 but in the Erlotinib Prevention of Oral Cancer (EPOC) trial,7 60% of patients had prior OSCC. That study followed a prevention-adjuvant therapy convergent design36 under the assumption that high-risk patients with oral premalignant lesions and resected cancers share molecular alterations for prevention and could be studied in similar settings.23,37,38 The cancer events among the patients in the current trial were most often pT1 lesions, but structured follow-up may have identified cancers earlier with a bias toward earlier biopsy. Longer follow-up in a larger randomized trial design will be needed to identify a time-to-event or survival benefit. It is unclear whether immunotherapy favorably affects the pathologic severity of future oral cancer events.
We acknowledge that novel pathologic criteria were required to evaluate clinical activity in this first oral precancer immune checkpoint therapy (ICT) prevention trial, as more traditional response criteria would not apply. We chose a modified composite scoring method to quantify response as a function of lesion size and dysplasia across multiple sites, recognizing that analyzing percent changes in composite score can be limited by small sample size and variability in scores. To limit interobserver variability, we required digital intraoral photography with bidimensional measurements and structured pathologic examination among 2 to 3 oral pathologists. We recognize that distinguishing mild dysplasia from hyperkeratosis can be subject to interpretation, and most of the cohort (73%) had mild dysplasia at baseline. Further, we observed a mix of lesion size and/or histologic changes in response to therapy among individual patients. We appreciate that multifocal lesions may have affected response assessments, but we would not expect spontaneous clinical regression in PVL in the absence of an effective therapy. A time-to-event CFS end point may be more generalizable and have broader clinical applicability. It is also worth noting that the trial population had limited racial and ethnic diversity, and many patients traveled to our center for treatment, which introduced some component of socioeconomic bias. This not only has potential treatment outcome implications, but also may influence tolerance and affordability.
A major concern for this ICT trial was safety, as we treated patients who did not have documented oral cancer. Frequently reported AEs were in line with prior head and neck cancer study populations more broadly.10–13 We observed some increase in grade 3 to 4 AEs (21.2%), although we permitted a history of autoimmune disease, and all higher-grade irAEs resolved in time with no deaths. These findings need to be weighed carefully against the potential for clinical activity, given concern for a narrow therapeutic risk-benefit ratio.
Patients with PD-L1 CPS scores of 20 or greater in PVL were not more likely to respond (as has been observed in advanced OSCC11), but this could be due to sample size limitations and/or scoring criteria (CPS is validated on invasive cancers); future studies will need to explore this further. Circulating CD4+/CD8+ T cells displayed significantly increased CD38 and reduced PD-1 expression following treatment, confirming on-target blockade of PD-1 and T-cell activation. An immune phenotype indicative of activation and/or reinvigoration was also observed on CD8+ T cells in oral dysplastic lesions, where surface expression of CD69 and LAG-3 were elevated in posttreatment samples.
Genomic studies of precancers have been limited by adequate tissue availability from small biopsies. Therefore, prior studies generally assessed single genes and/or allelic-imbalance using microsatellite markers, detecting 9p21.3 loss of heterozygosity in approximately 45% of patients with PVL, depending on the number of markers used.39 To our knowledge, this is the first study using WES in PVL, which revealed a range of complex SCNA and allelic-imbalance profiles. Recent data from several groups have found that 9p deletions encompassing 9p21 are significant and selective predictors of ICT resistance in advanced OSCC and lung cancer.23,24,40,41 This may be due to deletions encompassing the type I interferon gene cluster,42 which is often co-deleted with the tumor suppressor CDKN2A, highlighting a key mechanism of immune evasion.43 In our immunogenomic studies, only pretreatment 9p21.3 deletion yielded statistically significant differences: 6 of 10 patients with 9p21.3 deletion in baseline biopsies later developed cancer. We have previously shown that 9p21.3 copy-number loss is generally a focal event in oral precancer44 and associated with an immune-cold signal in OSCC23 that is enhanced by larger deletions extending to the telomeric band at 9p24.1.40 We speculate that resistance to the PD-1 inhibitor in this aggressive oral precancerous disease trial may have arisen during ICT resulting from increasing 9p deletion size to encompass 9p24.1, leading to low expression of the therapeutic target (PD-L1) and other immune gene depletion.23,40,45 PD-L1 is encoded by the CD274 gene, which is located on 9p24.1, close to 9p21, and is often co-deleted in advanced human papillomavirus–negative head and neck squamous cell carcinoma and lung cancers.42,44
Limitations
This study has limitations. We thought it was important to include patients with prior cancer events given their risk but recognize that this added some heterogeneity to the study population. This trial was single group and single center, using a novel clinical and pathologic scoring system to assess immunotherapy response in a hard-to-study oral precancer population. A lack of randomization or use of a time-to-event end point is another limiting factor to acknowledge.
Conclusions
We report the first (to our knowledge) nonrandomized clinical trial of ICT in patients with precancerous disease, specifically patients with high-risk oral precancer, to mitigate progression to OSCC. This trial met its primary response end point, but few patients had complete lesion regression. Other studies using immunotherapy to treat patients with high-risk oral premalignant lesions are ongoing.46,47 Recognizing the limitations and complexity of measuring treatment outcomes in precancer trials, for the first time, we demonstrate potential clinical activity and acceptable safety with the use of ICT in a population with high-risk precancer. A next step would be to consider a larger, precision immunotherapy randomized clinical trial favoring CFS as a primary outcome and stratified by prior history of early-stage treated OSCC and 9p21.3 loss.
Source: JCO