Proponents say that taking nonhallucinogenic doses of a psychedelic may deliver psychological perks, but much more research is needed, and we simply can’t draw conclusions yet.
Potential Health Benefits of Microdosing Psychedelics
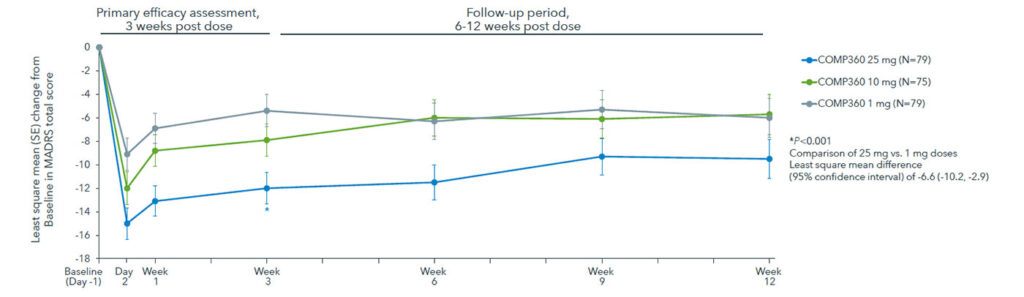
Early trials have pointed toward some benefits of psychedelic therapy.
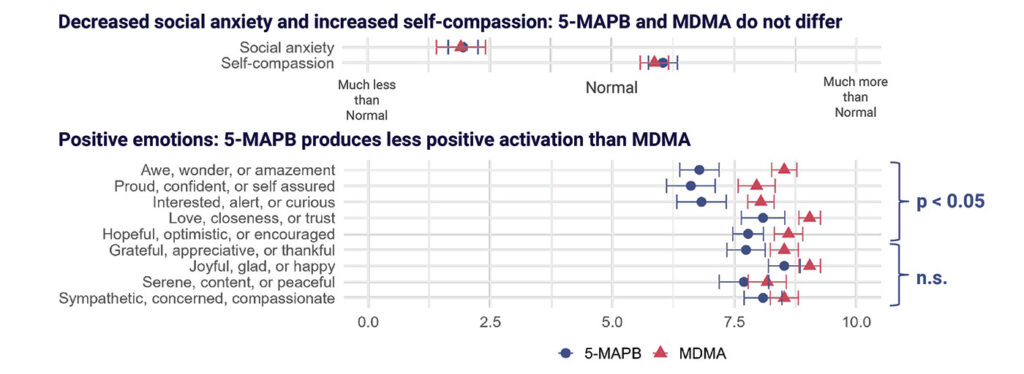
Psychedelic therapy as a possible treatment for conditions like depression, post-traumatic stress disorder, substance abuse, eating disorders, and more seems potentially promising. And microdosing — in theory, a method of taking psychedelics in nonhallucinogenic doses — may deliver some psychological benefits. That said, it is vastly underresearched in the already complex field of psychedelic therapy and, in many cases of certain psychedelics, is illegal in the United States.
Here’s what we know about microdosing right now. (Hint: It’s not much.)
An Overview of Psychedelic Therapy
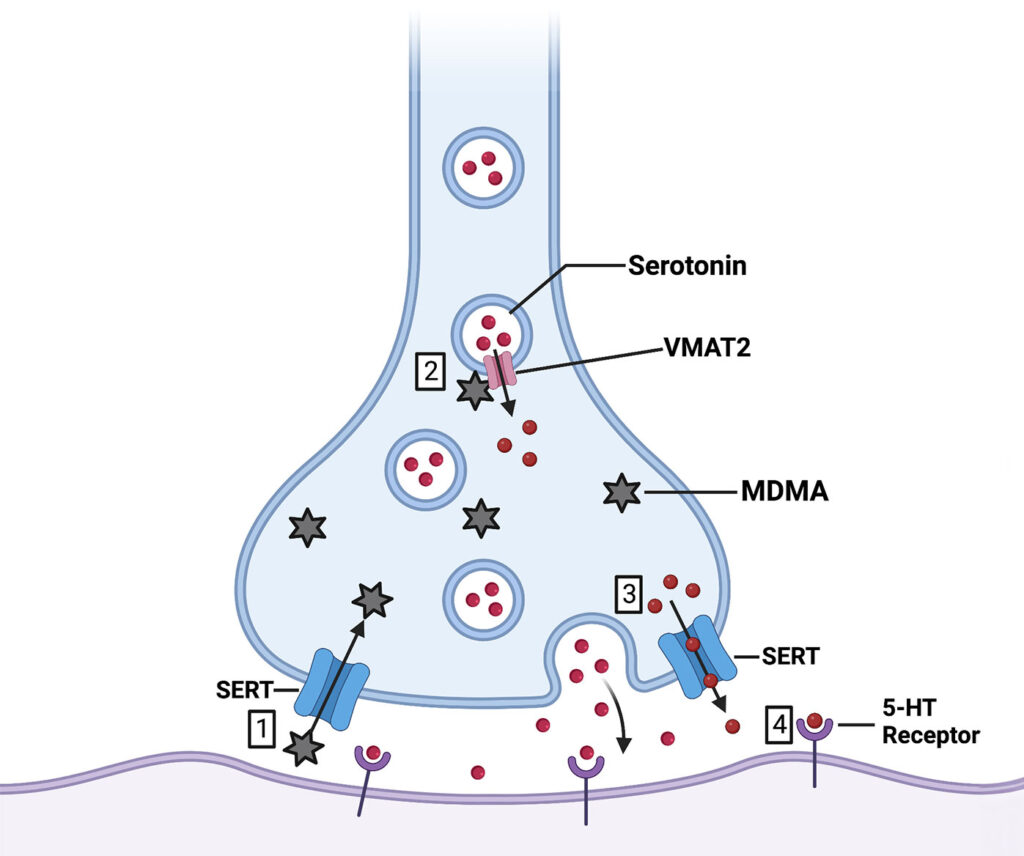
Here’s the main idea: Under the guidance of healthcare practitioners, often in clinical trials only, patients may take therapeutic doses of psychedelic substances, such as psilocybin (from “magic mushrooms”), LSD, MDMA, or ketamine, to experience a conscious-altering trip and potentially enact brain changes that affect the way they think, helping to pull them out of their psychological condition.
However, there are several downsides to psychedelic therapy, including legal complexities, potential side effects, adverse psychological challenges, and the extent of treatment, which requires lengthy and multiple sessions to possibly take effect.
In psychedelic therapy, some patients may not want to hallucinate — and that’s where a microdosing approach comes in.
It’s important to note that this article serves only as an informational resource about what we know on microdosing to date. Everyday Health is not in any way condoning the illegal use of psychedelic drugs for therapeutic or recreational purposes.

What Is Microdosing?
Microdosing psychedelics does not have an officially recognized medical definition or dosage amount, according to Harvard Health Publishing. But as the name suggests, microdosing is generally considered to mean taking less than the dosage needed to create hallucinogenic effects, per one research article. Though at this point, there are more questions than answers.
In one explanation from her own research, Harriet De Wit, PhD, a professor of psychiatry and behavioral neuroscience at the University of Chicago, describes microdosing as “taking very low doses of these drugs, about one-tenth of what you’d take to trip, and you take this dose every three to four days over an extended period of time.” For instance, you may need 100 micrograms (mcg) to get high; microdosing would be in the 10 to 20 mcg range.
According to most published research, microdosing is in reference to LSD, though there are also anecdotal reports of microdosing with psilocybin and MDMA, Dr. De Wit says. In theory, these low doses don’t cause hallucinogenic effects, but the goal behind microdosing is that taking small doses may change your brain under the radar, while you’re fully conscious and aware, and with the hope that this improves your sense of well-being overtime, she explains.
Challenges to Psychedelic Medicine
In regard to psychedelic therapy in general, and microdosing more specifically, it’s important to note two things.
Legalities Are Incredibly Complex and Evolving
Most psychedelics remain illegal for use, either in full doses or microdoses.
Esketamine (Spravato), a form of ketamine delivered via a nasal spray, was approved by the U.S. Food & Drug Administration (FDA) in 2019 for treatment-resistant depression when used under supervision in a medical setting, and it is the only substance considered a psychedeliclike medicine that’s federally legal.
Psilocybin has been approved by certain states, such as Oregon, for supervised use, and though licensed facilities administering the drug have not yet opened, some plan to do so in the coming months, according to an April 2023 article from Oregon Public Broadcasting.
LSD is considered a Schedule 1 drug, which is defined by the U.S. Drug Enforcement Administration as having “no currently accepted medical use and a high potential for abuse.” Still, legislative efforts to decriminalize psychedelics (on local and state levels) are growing, according to research.
That could all change, as the FDA released draft guidance in June 2023 for clinical researchers conducting studies around the use of psychedelic drugs as a potential treatment for psychiatric or substance use disorders. One obvious pain point is the need for more standardized clinical studies on these substances, and the FDA’s guidance advises on study design through drug development of psychedelic medicines. (This is currently in draft form, and the public has a chance to comment before the final version is released.)
Research Isn’t Clear (or Established)
What’s more — and this is key to keep in mind — research on psychedelic medicine is still in early stages, and the results are mixed. Studies are currently performed in academic medical settings via clinical trials, with the premise that participants take hallucinogenic doses of these substances, and research has a long way to go to draw more clear and widely applicable conclusions.
There’s even less data on microdosing, and many of the purported health benefits are only assumed from larger-dose trials. Even the benefits listed below may end up not being actual benefits of microdosing, as research evolves and becomes more clear in the coming months and years. Fundamentally, more research is needed, and it’s crucial to take the excitement surrounding psychedelic therapy with a grain of salt until we know more.
With all of that in mind, here’s what some experts and research presume about the possible health benefits of microdosing — though again, this could change.
1. May Lead to a Short-Term Mood Boost
LSD acts on the same serotonin neurotransmitter system as SSRIs, which are common antidepressant medications. That’s why there are theoretical reasons why the scientific community suspects that LSD taken as a hallucinogenic dose or microdose may be beneficial in mood disorders, De Wit explains.
De Wit and other researchers looked at this in a study in which people who did not have depression were given either a placebo, 13 mcg of LSD, or 26 mcg of LSD every three to four days, then monitored on their mood, cognitive performance, and responses to emotional tasks. (Both LSD doses were considered microdoses, for the study’s purpose.) The 26 mcg dose produced “feeling a drug” and stimulant effects when the drug was taken, but it did not change mood or cognition over the four-week course of the study.
That was admittedly a little disappointing to the researchers. “We were hoping to see a decrease in depression or anxiety scores, or more feelings of well-being. But the benefits were mixed and minimal,” says De Wit. “Each direct dose produces some feelings of well-being and energy, but over time that declines a bit, and you feel those effects less and less with each dose.” In the end, De Wit and her research colleagues could not find real improvements in feelings of well-being or behavior different from a placebo.
The placebo effect in medicine is well known and real, but there are downsides to banking on a placebo effect for benefits. That can lead to exploitation, says De Wit. “You want to make sure that claims made about a drug are genuine,” she says.
Another study randomized healthy male adults to take LSD or a placebo. The LSD group took 14 doses of 10 mcg of LSD every three days over six weeks. Ten percent of the LSD group dropped out due to treatment-related anxiety. Over the course of the study, daily questionnaires showed that people felt more creative, connected, energetic, and happy, as well as less irritable, and they experienced greater well-being on the days they were given the drug. However, these benefits were short-lived.
2. May Enhance Mental Performance and Creativity
One of the anecdotal benefits of microdosing is that it enhances creativity.
In research on microdosing psychedelic truffles (mushrooms), people who took a small dose of these psychedelics tested better on creative problem-solving tasks and cognitive flexibility compared with those who didn’t take these drugs. This study did not have a control group, and it was not measured against a placebo. Researchers point out that psychedelics may activate certain brain receptors linked to learning and adaptivity, which may increase the personality trait of openness and decrease rigidity in thinking.
In addition, a survey that recruited microdosers from online forums to complete questionnaires found that current and former microdosers rated higher on creativity, open-mindedness, and wisdom (the ability to learn from your mistakes while considering multiple perspectives), and lower on dysfunctional attitudes and negative emotionality, compared with nonmicrodosers. Most commonly, people used LSD and psilocybin. The researchers point out that people who have more dysfunctional attitudes tend to be more vulnerable to stress and depression. The sample used included mostly white, heterosexual, middle-class men, so a more diverse sample group is needed, as well as a more randomized and controlled population. Additionally, more controlled clinical trials would be needed to support claims of enhanced mental and creative performance
3. Low Doses May Still Allow You to Function Normally
Microdosing is more along the lines of taking a typical pharmaceutical drug, says Nese Devenot, PhD, a postdoctoral associate at the Institute for Research in Sensing at the University of Cincinnati. “While treatment with large doses requires 6 to 10 hours of your day and results in [potentially] profound alterations in one’s perception, a microdose can be iterated into your life because it’s a subhallucinogenic dose,” they say.
Some users say that microdoses produce no subjective effects, though many report that they do feel some stimulation. But in general, most people feel that they can go about their day as normal when microdosing, Dr. Devenot says, of their anecdotal understanding. Private advocacy groups, such as Moms on Mushrooms, aim to destigmatize microdosing plant-based medicines to take the edge off of the stress of parenting.
That said, one of the most common issues surrounding microdosing is accidentally taking too high of a dose. “If you’re trying to go to work, and objects and shapes are warping around you, that can be distracting and distressing if you were not prepared for an intense experience,” says Devenot. Plus, there are inherent risks if you’re driving, operating machinery, parenting, and doing other activities that require alert attentiveness.
Overall, the research cited here has found that microdosing (as it pertains to LSD) is generally safe for most people. However, there are many ways microdosing can go wrong. Unless you’re part of a clinical trial, you will most likely have to obtain the drugs illegally, which is not recommended by most doctors, scientific researchers, psychedelic experts, and certainly, Everyday Health. There are questions about the purity of the drug (if there are other substances within it) and variability of the dose, and that lack of control can be dangerous when you don’t know what you’re truly taking or how much, says De Wit. In addition, because there isn’t long-term research on microdosing, it’s not yet known if taking small amounts of one of these drugs changes the brain in unknown ways.
Bottom Line: We Need More Scientific Research
There are so many unknowns about microdosing. “People are considering these types of substances for all kinds of psychological disorders. It’s [uncharted] territory right now, since we don’t know what it does or who benefits,” says De Wit.
For Devenot’s part, they note that microdosing trials “have not stood up to the test of evidence-based science. I’m open to the science showing there are some benefits, but I’m not convinced from what I’ve seen that it’s more than placebo.” People who are desperate for answers, who want help with depression or PTSD or after a cancer diagnosis, commonly turn to the hope and promise of psychedelic medicine, but the science for microdosing is not there yet, she says.
That doesn’t mean microdosing should be entirely off the table as a possible route for healing in the future, however. “Though there is not enough evidence, an absence of evidence does not mean that it’s not working,” says De Wit. “It might mean that, as researchers, we haven’t found the right outcome to measure or that different people [and diagnoses] experience different benefits. But we haven’t seen them yet.” Still, this is an avenue that’s worth studying, within the greater context of psychedelic therapy, especially if people are experimenting on their own without telling their doctor. “This is a new era of psychedelic research that we should investigate in whatever way we can,” says De Wit.