Key takeaways:
- An e-consult program for oncologists and allergy specialists had a mean turnaround time of 19.7 hours.
- Nine out of 10 oncologists surveyed were very satisfied with this turnaround time.
Oncologists were satisfied with an electronic system for consulting with allergists about hypersensitivity reactions during chemotherapy, according to a study published in The Journal of Allergy and Clinical Immunology: In Practice.
However, specialists need to become more familiar with the system, Aleena Banerji, MD, allergist and immunologist, and Kimberly G. Blumenthal, MD, MSC, quality and safety officer, both in the division of rheumatology, allergy and immunology, department of medicine, Massachusetts General Hospital, and colleagues wrote.

“Chemotherapy hypersensitivity reactions have an incidence rate ranging from 10% to 15% for carboplatin but increases to more than 20% to 30% after seven cycles of treatment,” Banerji and Blumenthal told Healio in a joint statement.
“Incidence rates of hypersensitivity reactions to paclitaxel and docetaxel are approximately 10% and occur most often during the first or second treatment,” they continued.
Hypersensitivity reactions can range from a mild skin rash or hives to severe, life-threatening anaphylaxis, the authors said.
“Symptoms can appear within minutes of starting the chemotherapy infusion, which can be very scary to patients,” Banerji and Blumenthal said.
Milder reactions can be treated with antihistamines, but when the reaction is severe, trained staff need to be knowledgeable about managing anaphylaxis, they continued.
“Additionally, when a hypersensitivity reaction occurs to first-line treatment, a different second-line agent may be used, which can be associated with worse clinical outcomes for the patient,” Banerji and Blumenthal said.
The system’s success
Clinicians can use electronic consultations (e-consults) when they have questions for other clinicians about care for specific patients in outpatient treatment. These asynchronous communications rely on information available in the electronic health record.
Massachusetts General Hospital supports more than 20,000 e-consults each year across multiple specialties, the authors said, with an expected turnaround for each e-consult of 72 hours.
“The allergy/immunology group has been involved in the care of hundreds of patients with chemotherapy hypersensitivity reactions, but communication about care was frequently by text, phone or email,” Banerji and Blumenthal said.
“These communications were not subsequently documented in the patient’s chart and led to a lack of understanding of the care plan by the whole team, delays in patient care and suboptimal coordination of care,” they said.
The hospital instituted the e-consult program specific to hypersensitivity reactions (HSRs) during chemotherapy in October 2020 to reduce time to allergist recommendations and to improve formal documentation in the EHR.
Between October 2020 and August 2021, hospital personnel completed 165 e-consults specifically about chemotherapy HSRs. The mean turnaround time for these e-consults was 19.7 hours (standard deviation, 24.7 hours).
Each one of these e-consults included clear recommendations using the standard smart phrase in the EHR documentation, the researchers said, and 87 (53%) patients did not need a formal allergy consultation after the e-consult was completed.
The researchers distributed surveys to 47 oncologists before and after the e-consult program was launched. Fourteen (30%) responded to the pre-launch survey, 14 (30%) responded to the post-launch survey and 10 (21%) responded to both.
Seven of the 10 (70%) oncologists who answered both surveys said they primarily used email or texts to contact allergists for guidance when a patient had an HSR due to chemotherapy. The other three used the Epic system to request consultations.
Also, nine of the 10 oncologists who responded to both surveys were very satisfied with their methods for obtaining guidance from allergists in the pre-launch survey, and the 10th was somewhat satisfied.
All 10 of these oncologists also said that contacting an allergist was easy and that they spent less than 15 minutes coordinating allergy care for chemotherapy HSRs. Eight (80%) said they were very satisfied with allergy team response times.
According to the post-launch survey, four of the 10 (40%) continued to use email to contact allergists, and three of them only used email, but all 10 also said that they were very satisfied with their consultation methodology.
Further, 70% of the referring oncologists said that the e-consult’s reply speed was better after the program was launched in the post-launch survey, compared with 40% in the pre-launch survey, although the program did not have any impact on the time that oncologists spent coordinating care with the allergy team.
Nine (90%) of 10 oncologists additionally said that they were very satisfied with the time it took to receive a response from the allergy team once the program was launched, and six (60%) said the program was slightly or significantly better than the previous model for collaboration.
The oncologists unanimously said that the information in the e-consult was helpful for patient care as well.
In the free responses to a survey question about how the e-consults could be improved, two oncologists said they preferred to maintain other options for communication, and one expressed confusion about when a chemotherapy HSR e-consult should be ordered instead of a formal in-person consultation.
Looking ahead
E-consults save costs and improve efficiency in care by preventing the need for formal allergy consult visits, the researchers said, with an average turnaround of less than a day compared with more than 3 months in waiting time for outpatient clinic visits.
The less frequent use of texts and emails for consulting with allergy staff also is an improvement, the researchers continued, because the EHR does not document these communications. Also, texts and emails may lead to safety issues by not complying with health privacy laws and because of their absence in the EHR.
The researchers additionally said they expected more of the oncologists to use the e-consult program because of how it improves patient care. They also expressed surprise that the oncologists spent the same amount of time coordinating care, which they attributed to an existing culture of efficient patient care for HSRs.
“We were surprised about the lack of global understanding around an e-consult program, as our institution has vast experience with using e-consults,” Banerji and Blumenthal said. “Additionally, the lack of universal acceptance around using e-consults with clear benefit to patient care suggests we need to provide better education around e-consults.”
Based on these findings, the researchers called e-consults specific to chemotherapy a useful tool for consultations to improve patient care and EHR documentation, but overall success will depend on specialists who are familiar with the program.
Banerji and Blumenthal said the authors are now developing ways to educate their medical colleagues about the use of e-consults with an understanding of how they lead to improvements in patient care.
“Additionally, our goal is to evaluate the benefits and challenges of using e-consults in a larger number of chemotherapy hypersensitivity reactions,” they said
Perspective
For certain types of chemotherapy such as platinum drugs and taxanes, immediate hypersensitivity reactions are fairly common. The longer a patient is receiving these drugs, the higher the chance is of experiencing one. For patients who are on these drugs for more than 12 cycles, the chance is almost 50% that they will have a reaction at some point.
There also is a chemotherapy for head and neck cancer (cetuximab) that is a little more likely to cause an immediate reaction in the parts of the country (the Southeastern U.S., mostly) where alpha-gal allergy is present.
Other types of chemotherapy do have hypersensitivity reactions, but they are not as common. They are more like other drugs in their reaction rates. Depending on the drug, you get different profiles of reactions that are possible to experience. This paper appears to mostly focus on the immediate types of reactions based on their description.
Oncologists in our system at Vanderbilt will usually reach out to their allergist colleagues via a consult request in our EHR after a reaction. But typically, they will also reach out personally via phone, EHR messages or HIPAA compliant messaging. The initiation of provider-to-provider communication is important when you are managing an event that might limit a patient’s ability to receive first-line therapy for cancer.
E-consultations can improve care in these cases. Currently, we do not have a formal system promoting e-consultations, but it definitely is something that we do for our oncologists when they or their patients need us to. It is like using the EHR to have a back-and-forth conversation.
I personally think that the most efficient way to go about it, for us, has been to have the oncologist reach out with a referral, let us know what they observed during the reaction, and then we facilitate the patient getting seen by me or a colleague within a week, so we don’t slow down their chemotherapy treatments.
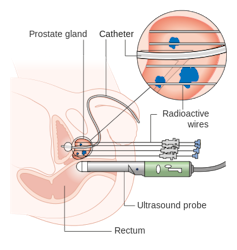
We (the allergists) will then have a telehealth or in-person consultation with the patient to discuss the reaction and the management options. Then we go back to their treating oncologist with recommendations, at which point we all try again using a modified plan under careful observation (sometimes in the hospital setting) and see how it goes. Sometimes we will use chemotherapy skin testing to identify a culprit allergen, but oftentimes it is not necessary since the history is enough to let us know what to do.
So, the system described in this study is similar to my experience. I think we are all trying to tackle this problem of making sure that our vulnerable cancer patients don’t fall through the cracks and miss out on their key chemotherapy treatments even if they have reactions to them. We want to make things safe and keep the quality of what we are doing up to the highest level.
It is important for the public to be aware that there are protocols that can make it possible even for a patient who has had an immediate reaction or allergy (anaphylaxis type) to chemotherapy to tolerate it safely. We use specialized, slow infusion protocols called desensitization protocols to deliver the drugs without setting off their reactions.
It is more work for everyone to treat a patient who has become allergic to their chemotherapy, but it is work that is worth doing to make sure they don’t miss out on the best drugs for their cancer. I have patients that I suspect are still alive today because they did not have to miss out on the drug that was actually working against their tumors.
Finally, I think these authors did a great job in trying to figure out how to facilitate good communication at their institution. When you are dealing with an allergic reaction, 80% to 90% of good medical care going forward comes down to communication amongst the treating team and the patient, in my experience.
Cosby A. Stone Jr., MD, MPH
Assistant Professor in Allergy/Immunology, VUMC Drug Allergy Research, Vanderbilt University Medical Center