Summary: During periods of social isolation, astrocytes in the brain become hyperactive. This suppresses circuit formation and memory formation. Reversing astrocyte hyperactivity can help mitigate memory deficits associated with social isolation.
Source: Baylor College of Medicine
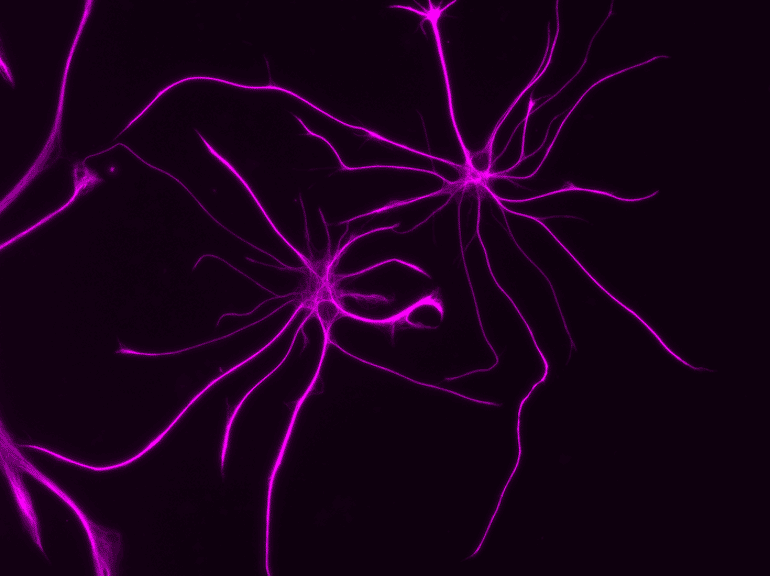
Here is an important reason to stay in touch with friends and family: social isolation causes memory and learning deficits and other behavioral changes. Many brain studies have focused on the effects social deprivation has on neurons, but little is known about the consequences for the most abundant brain cell, the astrocyte.
Researchers at Baylor College of Medicine working with animal models report in the journal Neuron that during social isolation, astrocytes become hyperactive, which in turn suppresses brain circuit function and memory formation. Importantly, inhibiting astrocyte hyperactivity reversed the cognitive deficits associated with social deprivation.
“One thing we have learned during the COVID pandemic is that social isolation can influence cognitive functions, as previous studies suggested,” said co-first author, Yi-Ting Cheng, graduate student in Dr. Benjamin Deneen’s lab at Baylor. “This motivated co-first author Dr. Junsung Woo and me to further investigate the effects of social isolation in the brain, specifically in astrocytes.”
Astrocytes play diverse roles in the brain such as supporting the functions of neurons, participating in synapse formation and function, releasing neurotransmitters and making the blood-brain barrier.
“Under normal group housing conditions, astrocytes facilitate and promote circuit function and memory,” said Deneen, professor and Dr. Russell J. and Marian K. Blattner Chair of neurosurgery and director of the Center for Cancer Neuroscience at Baylor. He also is the corresponding author of the work.
“However, we found that during social deprivation, astrocytes in the brain region known as the hippocampus actually suppress circuit function and memory formation. The broad conclusion is that astrocyte function is tuned to social experiences.”

Looking for a deeper understanding of the mechanism by which astrocytes of socially-isolated mice cause learning and memory deficits, the researchers studied calcium ions (Ca2+), which previous studies had shown play a central role in astrocyte-mediated learning and memory behaviors.
“We evaluated the effect of social deprivation on astrocyte Ca2+ activity and discovered that social isolation greatly increased it, specifically the activity involving Ca2+ channel TRPA1. This in turn was followed by the release of the inhibitory neurotransmitter GABA that put a break on neural circuits involved in memory and learning,” Cheng said.
“Importantly, both pharmacological and genetic inhibition of TRPA1 reversed the physiological and cognitive deficits associated with social deprivation.”
“Although social isolation also affects other brain cells, we are very excited about the discovery that specifically manipulating astrocytes is enough to restore learning and memory deficits triggered by social isolation in animal models,” Deneen said.
“Our findings show a new role for astrocytes in brain physiology,” Cheng said. “What astrocytes do is affected by changes in the environment and will reflect in the animal’s behavior. In this case, we learned that social interaction is good for astrocytes and therefore, for the brain.”