A groundbreaking discovery in pain management could revolutionize how we treat chronic pain. In a report from a study published in the Proceedings of the National Academy of Sciences, researchers at New York University, in collaboration with colleagues at the University of Pittsburgh, have announced the discovery of a novel medication that could treat centralized pain that targets Cav2.2 calcium channels (also called N-type calcium channels).
First, what is centralized pain? Why don’t other pain medications work well against it? And why does this medication target Cav2.2 calcium channels? An example of a pain-relieving medication working through ion channels is lidocaine. Lidocaine binds to and inactivates voltage-gated sodium channels. Since these are important for peripheral pain reporting nerves, it can block pain for several hours.
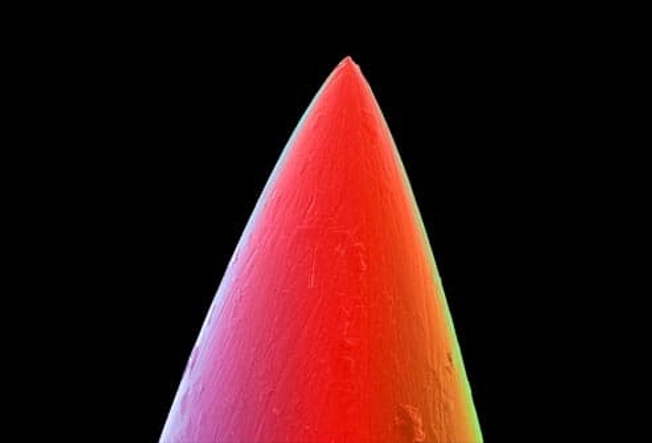
Researchers at the Pain Research Center at NYU College of Dentistry were very interested in calcium channels called Cav2.2 because they play a crucial role in the transmission of pain signals in the central nervous system. If we could slow down or block these channels, we could reduce the ability of these second and third-order neurons to produce pain signals. This would be incredibly important to most chronic pain sufferers since these channels are integral to pain transmission in second and third-order afferent nociceptive neurons.
Drugs like gabapentin and pregabalin, Neurontin, and Lyrica bind these receptors at the alpha-2-delta subunit of the Cav2.2 channel, reducing pain signal transmission. This class of medications is called gabapentinoids, and while these medications are now widely used for nerve pain and epilepsy, as they are the best we have right now, they are not without problems.
Gabapentin is recommended as a first-line treatment for chronic neuropathic pain by various medical authorities, and this is a general recommendation applicable to all neuropathic pain syndromes except for trigeminal neuralgia, where it may be used as a second or third-line agent.
Gabapentin and pregabalin, while therapeutic, also produce feelings of relaxation and euphoria. And human beings tend to want to repeat activities that generate these feelings. It turns out that with the increasing prescription rates of gabapentin, there’s been a corresponding rise in its misuse. People subject to substance abuse issues, which is pretty much everyone under the right circumstances, may be drawn to gabapentin and pregabalin for their calming effects. If mixed with opioids, alcohol, or other depressants, a synergistic response can be elicited, and gabapentin’s effects can be amplified, leading to increased sedation and, in some cases, dangerous respiratory depression. An alcohol-like effect if you will.
Overdose-related deaths due to gabapentinoids themselves are still quite rare, and of course, any medication or substance can kill you if you take enough of it. Much more commonly a problem, however, is the potential for the gabapentinoids to produce euphoric effects in a subset of patients. This can quickly lead to a substance use disorder, even addiction perhaps.
A substance use disorder can be considered a situation where someone chooses to use a substance or activity to alter their mood or experience euphoria despite negative life consequences. Addiction, on the other hand, could be considered a loss of control of the use of a substance or activity. These people cannot stop even if they really want to. This loss of control is mediated by overexpression of the gene deltaFosB, in the nucleus accumbens of the brain, and seems to be directly related to euphoric effects.
The risk of Gabapentin abuse highlights the need for careful prescription and monitoring practices. Health care providers are advised to screen patients for a personal or family history of substance abuse, especially to alcohol or sedatives, and for mood disorders like depression and anxiety, before prescribing gabapentinoids.
Patients should also be educated about the risks of misuse with regular follow-ups and monitoring as always. Understand, however, that just because a medication has drawbacks, does not mean that politicians and government agents need to Monday morning quarterback a doctor’s decision to use these medications.
In fact, there is evidence that gabapentinoids can be used effectively in the treatment of alcohol and sedative addiction through medication-assisted therapy (MAT). MAT is where a doctor can take a substance that has a similar but milder effect than the drug of abuse, and uses that to help someone maintain control of their addiction. This is how medications like Suboxone work. Hopefully, tapering off the milder medication later, though some people need maintenance therapy to avoid relapse.
Gabapentinoids have been an amazing medication for those suffering from nerve-related pain. But what if we could find a better way to produce this effect? Without the potential for euphoria?
There is a natural 17-amino acid molecule called CBD3 that specifically binds and deactivates the Cav2.2 calcium channel. What if we found a medication that worked like this natural molecule? In a report from a study published in the Proceedings of the National Academy of Sciences, it was announced that we may have a significant breakthrough in this pursuit.
Researchers at New York University, in collaboration with colleagues at the University of Pittsburgh, ran a computer simulation that screened a library of 27 million compounds to look for a small molecule that would “match” the CBD3 amino acids. The simulation narrowed the library down to 77 compounds, which the researchers experimentally tested to see if they lessened the amount of calcium influx. This further pared the pool down to nine compounds, which were assessed using electrophysiology, to measure decreases in electrical currents through the calcium channels.
One compound, which the researchers named CBD3063, emerged as the most promising candidate for treating centralized pain through this approach. Biochemical tests revealed that CBD3063 disrupted the interaction between the CaV2.2 calcium channel and CRMP2 protein. CRMP stands for Collapsin Response Mediator Protein, and it is critical to neuroplasticity in these central pain nerves. CRMP2 regulates the trafficking and surface expression of various ion channels and receptors, including Cav2.2 calcium channels, thereby reducing the rate of calcium entering the channel. This reduces the firing rate of central pain neurons and lessens the release of neurotransmitters, reducing the pain signal.
This new compound was later proven effective at reversing four types of chronic pain in animal studies: chemotherapy-induced neuropathy, inflammatory pain, acute injury-related pain, and trigeminal neuralgia. What’s remarkable is that it outperformed gabapentin, without any evidence so far of troublesome side effects. This discovery is not just a scientific achievement; it’s a beacon of hope for millions suffering from severe chronic pain, and it underscores the importance of innovative research in developing new pain therapies.