Pulsed electromagnetic field (PEMF) therapy shows promise in reducing pain and improving quality of life for osteoarthritis patients.
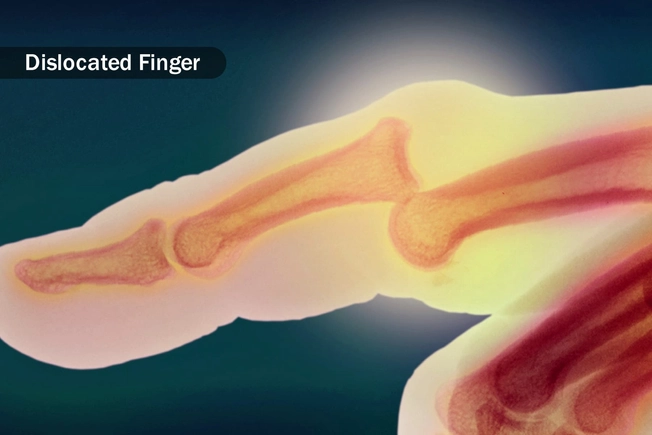
As the U.S. population grows older, an increase in agonizing joint conditions lurks on the horizon. Chief among them is osteoarthritis, a debilitating disease caused by the natural breakdown of cartilage.
But new research suggests that a solution may lie in the power of magnetic fields—a drug-free therapy that could offer relief without the risks of common painkillers.
Pulsed Electromagnetic Fields Shown to Significantly Reduce Pain
A recent systematic review published in the Journal of Clinical Medicine sheds light on the potential of pulsed electromagnetic field (PEMF) therapy, introduced into clinical practice in the 1970s with a device approved by the Food and Drug Administration to help speed up the healing of broken fractures to alleviate symptoms of osteoarthritis.
For the new review, researchers analyzed 17 randomized controlled trials involving 1,197 patients with osteoarthritis who underwent PEMF therapy. They assessed the data to evaluate the effectiveness of PEMF across different anatomical areas, focusing on levels of pain reduction and improvements in patients’ quality of life.
The findings suggest that PEMF therapy significantly improved pain reduction, as assessed through the Visual Analog Scale (VAS) and Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) scores. VAS scores decreased by 60 percent, and WOMAC scores improved by 42 percent.
The review also noted participants’ reduced medication usage and enhanced physical function.
Despite these positive outcomes, the review highlighted the variability in treatment duration and the types of PEMF devices used, with the study authors calling for further investigation and standardization in these areas.
How Magnetic Therapy Works
PEMF therapy has gained popularity for its ability to alleviate pain and support healing across various conditions, Dr. Peter C. Lascarides, assistant professor of physical medicine and rehabilitation at the Zucker School of Medicine at Hofstra/Northwell Health, told The Epoch Times.

“It’s especially useful for people with chronic pain conditions like fibromyalgia, known for causing widespread pain and fatigue and osteoarthritis, which involves significant joint pain and inflammation,” he said.
Beyond speeding up the healing of broken bones, there is evidence that PEMF therapy helps to improve physical function and decrease stiffness, according to Dr. Lascarides.
PEMF is currently also used to stimulate the body in ways that aid in pain relief and tissue regeneration. This electromagnetic-based therapy is already commonly used for bone fractures that fail to heal within three to six months.
Patients are prescribed a small, battery-powered pulse generator connected to a coil placed next to the injury for eight to 10 hours per day. Alternatively, an electrical stimulator may be implanted near the break. Either way, the PEMF device generates a magnetic field that induces currents to flow in the nearby tissues.
“By using electromagnetic fields, PEMF therapy stimulates the body’s own healing mechanisms,” Dr. Lascarides said, “which encourages ’self-repair’ that can lead to marked improvements in comfort and mobility.”
PEMF Considered Safe With Minimal Side Effects
Overall, PEMF therapy is considered a safe treatment with minimal significant side effects.
Most people experience no issues during therapy, although a few may feel slight, brief discomfort at the point of application, Dr. Lascarides said. However, he noted that people with electronic implants, such as pacemakers, should avoid PEMF therapy to prevent potential interference with their devices.
Because of limited research on the effect of PEMF therapy on pregnant women, they should forego this treatment as a safety precaution, he said.
The existing research in this area raises some concerns. A small 2019 study published in Environmental Health found that prenatal exposure to an extremely low magnetic field had measurable adverse effects on female infants, although not on males. Effects included smaller head, upper arm, and abdomen circumferences, suggesting reduced fetal growth.
Pain Relief Without the Risks Linked to NSAIDs
Current research on PEMF therapy is “encouraging,” suggesting that it may be an effective, noninvasive method for managing pain and aiding healing without relying on drugs or surgery.
This is significant, as nonsteroidal anti-inflammatory drugs (NSAIDs) come with a broad range of side effects, including increased risk of gastrointestinal bleeding, heart attack, and stroke.
Chronic NSAID use has also been associated with an elevated risk of peptic ulcers and acute kidney failure.
Dr. Lascarides said PEMF therapy is promising as a possible treatment option to alleviate patients’ discomfort and improve their quality of life without the usual risks and side effects of traditional pharmaceutical-based pain treatments. However, there is still much to learn about it, he said.
“Ongoing and additional studies are crucial to further understand how PEMF therapy can be best applied, who stands to benefit most from it, and how it can be integrated into more comprehensive care strategies to optimize its advantages for those seeking relief,” Dr. Lascarides said.