Key takeaways:
- The blood test reliably detected patients with stage I and II pancreatic ductal adenocarcinoma with 97% accuracy.
- Combining microRNA markers with CA 19-9 improved diagnostic accuracy.
Perspective from Sanjay S. Reddy, MD, FACS
An investigational exosome-based liquid biopsy showed better than 90% accuracy for detecting early-stage pancreatic cancer among U.S.-based participants in a prospective multicenter study.
When combined with a signature that identified the protein CA 19-9, a known tumor biomarker for pancreatic cancer, the novel liquid biopsy accurately detected 97% of stage I or stage II pancreatic ductal adenocarcinoma in the same study cohort, according to data presented at American Association for Cancer Research Annual Meeting.

Data provided by the NCI highlighted the need for early detection of pancreatic cancer —the 5-year survival rate for individuals diagnosed at stage I or II before the cancer has spread outside of the pancreas is approximately 44% compared with an estimated 3.2% for patients with metastatic disease.
“We purposefully focused ourselves to try to find this cancer as early as possible, preferably stage I or II, and the reason being that if you find somebody with a stage I or II (pancreatic) cancer, there’s a very high chance you can surgically remove the cancer and that’s probably the best way to manage these patients,” Ajay Goel, PhD, AGAF, professor and chair of the department of molecular diagnostics and experimental therapeutics at Beckman Research Institute of City of Hope and associate director of basic sciences at City of Hope Comprehensive Cancer Center, told Healio. “Even in patients with early stage I cancer, if you remove the cancer completely some of the patients can be actually ‘cured,’ which is a frowned upon word when it comes to pancreas cancer, but it is feasible.”
Background, methods
Pancreatic ductal adenocarcinoma (PDAC) is one of the more lethal human malignancies, with 5-year survival rates dropping dramatically if diagnosed in later stages.
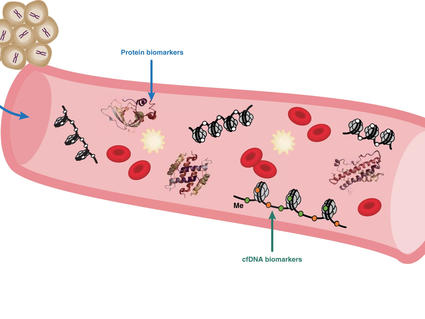
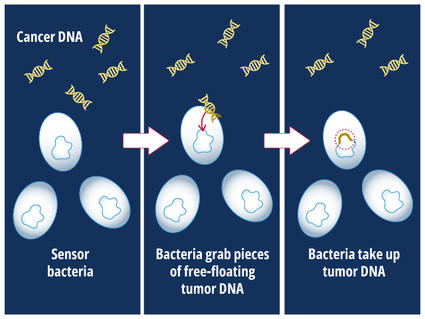
Researchers at City of Hope previously reported on a noninvasive exosome-based liquid biopsy assay that can assist in the early detection of PDAC. At AACR Annual Meeting, researchers presented study results that sought to validate performance of the liquid biopsy assay in a multi-institutional international evaluation.
The study included patients from Japan (150 with PDAC and 102 healthy controls), the United States (139 with PDAC and 193 healthy donors), South Korea (184 with PDAC and 86 healthy donors) and China (50 with PDAC and 80 healthy donors).
Researchers conducted a real-time quantitative polymerase chain reaction-based assay using plasma biospecimen from the four cohorts, while also evaluating the performance of the microRNA (miRNA) signature in combination with plasma CA 19-9 to detect early-stage PDAC.
Results
Researchers established two panels — cell-free miRNAs and exosomal miRNAs — through the Japan cohort, which was used as a training cohort. Patients with PDAC had area under the curve (AUC) values of 0.95 and health donors had 0.97.
After combining the two panels, researchers noted that the resultant signature had 98% accuracy distinguishing between patients with PDAC and healthy donors with 98% accuracy.
Researchers validated the signature’s detection ability in the three additional cohorts (U.S., AUC = 0.93; South Korea, AUC = 0.91; China, AUC = 0.88).
When combined with detection for CA 19-9, researchers reported that the overall diagnostic performance of the liquid biopsy assay improved significantly for the early detection of PDAC (AUC = 0.97; with 95% sensitivity and 96% specificity).
Next steps
Researchers believe the noninvasive exosome-based liquid biopsy assay can provide early detection of PDAC, with upcoming validating studies in development before potentially being available in clinics.
“We published this study a year or so back and we had the numbers in the (lower 90s) but we continued to tweak the assay, which we knew by doing so would optimize it further and we would see an overall gain — but we didn’t expect it to be 97% accurate,” Goel told Healio. “These data give us a lot more confidence and promise.”
Despite not being ready for clinical use, deployment of the detection assay is not far off in the future either, he added.
“I think we are getting closer to cracking the code on early detection of pancreatic cancer,” Goel said. “Overall, these results are quite promising, but we do still have a lot more work ahead of us.”
References:
- AACR. An exosome-based liquid biopsy shows promise for early detection of pancreatic cancer (press release). Available at: https://www.aacr.org/about-the-aacr/newsroom/news-releases/an-exosome-based-liquid-biopsy-shows-promise-for-early-detection-of-pancreatic-cancer/. Posted April 8, 2024. Accessed April 9, 2024.
- Nakamura K, et al. Gastroenterology. 2022;doi:10.1053/j.gastro.2022.06.089.
- Xu C, et al. Abstract 3899. Presented at: The American Society of Breast Surgeons Annual Meeting press briefing; April 3, 2024; virtual.
PERSPECTIVE
This study centers around the concept of early detection of pancreatic cancer. Because this is one of the most aggressive malignancies, this proves to be pivotal in the fight against pancreas cancer. Although there has been no ideal biomarker screening mechanism for early detection, the fundamental ability of a blood test to detect signatures of shed tumor cells — in theory — holds tremendous promise. Utilizing traditional blood tests such as a CA 19-9 — and now these exosome liquid biopsies — at an early stage could lead to a simple way to potentially screen individuals who may be at higher risk. The primary concern with pancreas cancer is that this disease is often systemic, and deep-rooted weeds prove to be the most challenging to address. With these novel techniques for early detection, we hope to address the evolution of this disease at a time point where we can successfully intervene.
Sanjay S. Reddy, MD, FACS
Marvin S. Greenberg, MD, chair in pancreatic cancer surgery
Fox Chase Cancer Center