Lab-made “mini-brains” are helping scientists makes a breakthrough involving a gene implicated in various neurodegenerative diseases linked to old age. These include frontotemporal dementia (FTD), amyotrophic lateral sclerosis (ALS), and Parkinson’s disease. Scientists in the United Kingdom say this work may pave the way for new detection methods and treatments to address these awful diseases before symptoms ever appear.

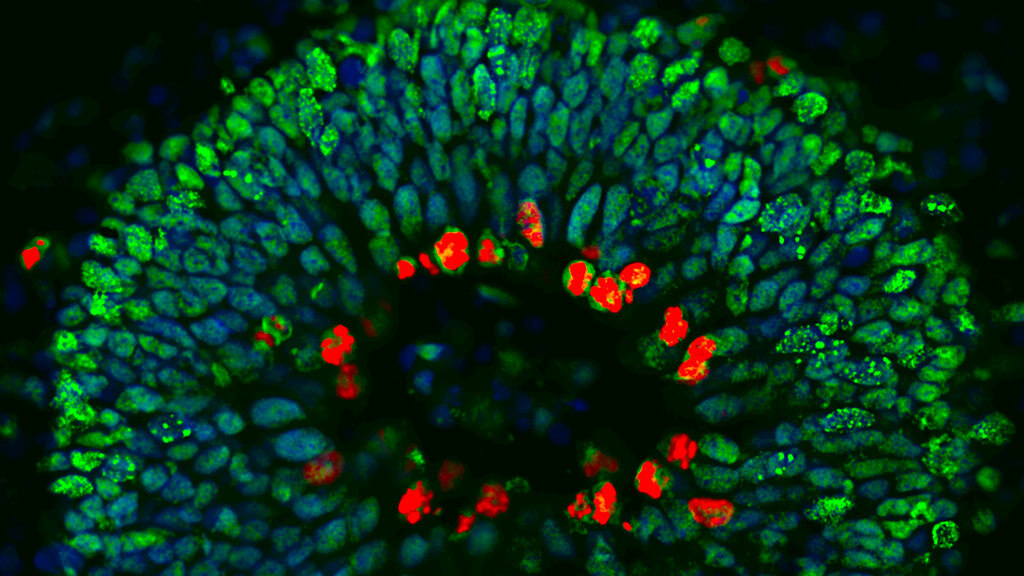
Scientists at the University of Bath explain that in its healthy state, the gene in question (called Angiogenin or ANG) actually plays a very important role in the speed at which undifferentiated stem cells develop into specialized nerve cells. The mutated version of the gene is where things go awry.
In its mutated form, ANG causes stem cells to persist in their original state far longer than they should. In lab experiments, this slowing down of the differentiation process resulted in striking neurodevelopmental defects across nerve cells upon reaching their adult form.
“This suggests nerve-cell degeneration may be primed by defects occurring during early development,” says Dr. Vasanta Subramanian, who led the research from the Department of Life Sciences, in a university release.
During an earlier study, the same Bath research group discovered that ANG, in its healthy form, works to protect nerve cells against damage, degeneration, and any impairment of function. Conversely, the mutated form of the gene makes nerve cells more susceptible to stress (a natural occurrence as cells age and experience wear and tear), eventually leading to premature cell death.
“This new discovery adds to our understanding of Angiogenin and its importance in protecting us from diseases associated with aging,” Dr. Subramanian adds.

To conduct this latest study, the research team chose to focus on a family affected by both frontotemporal dementia and ALS. Genetic testing showed that certain family members had mutations in Angiogenin while others did not.
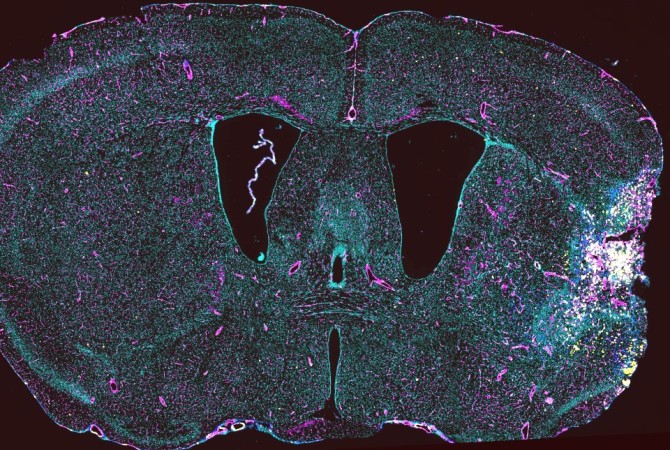
Scientists grew “mini-brains” in a lab for all the family members. A mini-brain is a tiny 3D structure grown using clusters of human stem cells. They serve as realistic models for scientists to study the step-by-step development of disease, and also serve as ideal structures to screen drugs. Study authors noted striking neurodevelopmental defects in the mini-brains of family members carrying the ANG mutation.
“This seems to indicate that subtle development defects play a role in disease susceptibility or onset,” Dr. Subramanian adds. “I envisage a time when we will be identifying people who are susceptible to these diseases, screening them for genetic mutations and offering early-intervention gene therapy to fix the defects.”
In conclusion, Dr. Subramanian stresses the need for more research in order to further clarify the mechanisms by which ANG protects cells and better understand its function in stem cells. This study received funding from the National Centre for the Replacement, Refinement and Reduction of Animals in Research (NC3Rs), BRACE, and the Wellcome Trust VIP award.
“We applaud Dr Subramanian’s innovative research, which could make a big difference in tackling frontotemporal dementia. Better understanding of the Angiogenin gene and its link to FTD could support treatment to slow down or stop the disease in the future. This type of dementia tends to have an early onset between the ages of 45-65 years, and often has a devastating impact during middle age. We are hopeful that this BRACE funded research may play a key role in one day reducing the impact of the condition,” says BRACE CEO Chris Williams.
“Research into the brain and neurological disorders relies in large part on animal models and it is fantastic to see Vasanta’s mini-brain ‘organoids’ delivering new insights into neurodegenerative diseases. It is testament to the utility of these models that they are still being applied to new research questions, almost 15 years after we awarded Vasanta the initial funding to develop human cell-based alternatives to the use of animals in ALS (the most common form of motor neuron disease) research,” comments Dr. Jessica Eddy, NC3Rs Regional Program Manager.