Ongoing research reveals synergistic effects of gut bacteria working to clear cholesterol. Higher levels of bacteria are associated with lower cholesterol.
New research highlights species of healthy gut bacteria that play a key role in helping regulate cholesterol levels.
Published April 2 in Cell, the study identified that specific bacteria in the genus Oscillibacter consume cholesterol, and that people with higher levels of Oscillibacter in their guts had corresponding lower levels of cholesterol. The findings come from among more than 1,400 samples examined as part of the long-term Framingham Heart study aimed at lowering the damage from cardiovascular disease.
Stool samples are often used to determine the microbial composition of the gut microbiome, which is made up of bacteria and other microorganisms like viruses and fungi.
The research team’s goal was to identify how the gut might play a role in lowering the risk of heart disease, the top killer in the United States. One in every five deaths—about 695,000 people—was from cardiovascular disease in 2021, according to the U.S. Centers for Disease Control and Prevention.
Unraveling Microscopic Mysteries
The research involved collecting a library of stool samples over many years and then sorting through more than 16,000 relationships between microbes and their metabolic traits. Scientists noted the strongest association discovered was Oscillibacter levels appearing to be protective of cholesterol levels.
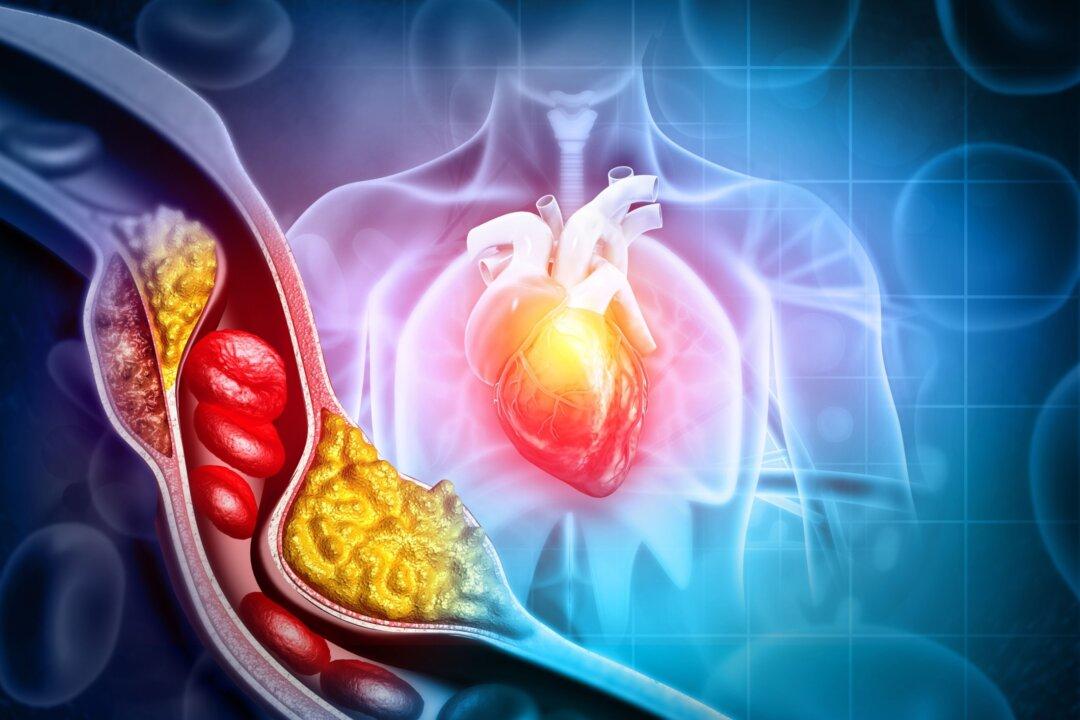
Cholesterol and other substances create plaque—a condition called atherosclerosis—that can build up in the arteries blocking blood flow and potentially lead to heart disease, stroke, heart attack, and blood clots.
Further tests involving growing the bacteria to study metabolic pathways revealed that bacteria converted cholesterol into other products before it was broken down by other bacteria and then excreted. Researchers were assisted by machine learning to determine that Oscillibacter were responsible for creating that biochemical conversion, according to a news release published by the Broad Institute of MIT and Harvard
Researchers also found another bacterial species previously discovered to contribute to lowering cholesterol, Eubacterium coprostanoligenes, may have a synergistic effect with Oscillibacter in metabolizing cholesterol.
“Our research integrates findings from human subjects with experimental validation to ensure we achieve actionable mechanistic insight that will serve as starting points to improve cardiovascular health,” said Dr. Ramnik Xavier, co-director of the infectious disease and microbiome program at Broad, in the news release. He is a professor at Harvard Medical School and chief of gastroenterology at Massachusetts General Hospital.
Expanding Understanding
According to a Harvard Medical School article, scientists have known for a century that gut bacteria break down cholesterol into coprostanol, though they didn’t understand the mechanism or species involved.
An earlier study from the team published in 2020 in Cell Host and Microbe looked at 3,097 stool samples and found that people who had a particular gene in their microbiome—called IsmA—had less cholesterol in their stool, as well as lower blood cholesterol levels. The gene, they determined, made an enzyme to metabolize cholesterol, explaining how some people can eat diets higher in cholesterol but don’t impact their blood cholesterol levels.
“The findings lend more support to the concept that modifying the microbiome could have a therapeutic effect,” study co-author Dr. Stanley Shaw said in the article. A cardiologist at Brigham and Women’s Hospital and associate dean for executive education at Harvard Medical School, Dr. Shaw noted that microbiome-based therapy for heart disease will take years to develop.
Microbiome Therapeutics Coming … Someday
Therapies could mean specific enzyme therapy, probiotics, diet, or other methods. Probiotics can be found in foods like yogurt and fermented vegetables—or in supplements.
The latest study reiterates that the work could ultimately point them to a method for manipulating the microbiome in order to decrease cholesterol levels.
“Our work highlights the possibility that additional sterol metabolism pathways may be modified by gut microbes. There are potentially a lot of new discoveries to be made that will bring us closer to a mechanistic understanding of how microbes interact with the host,” postdoctoral researcher Chenhao Li, a co-first author of the study, added.
Is More Medical Intervention Better?
Though the researchers may be well-intentioned, Dr. Craig Backs told The Epoch Times that strictly honing in on bacteria is overly simplified, has gaps that ignore underlying issues, and leads to a “pill for an ill” approach already dominating medicine.
“There’s clearly more to it than, ‘Fix your cholesterol, and you’ll have less heart disease,’” he said, noting that cholesterol is also one of several risk factors that include smoking, obesity, diet, diabetes, and high blood pressure.
He added, “You can talk about the microbiome all you want, but the way to support the microbiome is to feed the microbiome whole foods.”
Dr. Backs, an internist and founder of the Cure Center for Chronic Disease, coaches his patients to eat more healthily, including staying away from sugar, which also increases cholesterol and wreaks havoc on cardiometabolism.
His intent is to help patients understand why their cholesterol is elevated in the first place and reduce reliance on medication. The Mayo Clinic states that high cholesterol can be the result of inactivity, an unhealthy diet, and even some medications. Genetics can play a role, but it’s overstated.
“If your cholesterol is high, odds are you got it the old-fashioned way through a questionable diet, a lack of exercise and the process of aging,” interventional cardiologist Dr. Leslie Cho said in a Cleveland Clinic article.
Circling Back to the Microbiome
Those lifestyle factors are also linked to dysbiosis—an imbalance of gut microbes that causes the populations of good bacteria to decrease. In fact, lower levels of Oscillibacter bacteria have been associated with obesity.
Oscillibacter metabolizes to create the short-chain fatty acid butyrate. Among its roles in the human body, butyrate helps ameliorate oxidative status. Left unchecked, oxidation in the body can create a kind of inflammatory response that allows for plaque buildup.
With trillions of bacteria living in the human gut—including some not yet identified—associations are a complex medical mystery scientists are still unraveling. But the relationship between functional foods and the cholesterol-lowering mechanisms of the gut microbiota warrant significant study, notes a 2023 study in Foods.
“Gut microbiota dysbiosis is a risk factor in the pathophysiological processes related to cholesterol-associated diseases, constituting a subtle and potential mechanism of disease onset,” the study concludes. “Furthermore, the interaction between natural functional [food] ingredients and the cholesterol-lowering actions of the gut microbiota also represents a significant focus of research.
“This focus is poised to profoundly impact the development of novel therapeutic strategies for drug treatment.”















