Summary: Vitamin D enhances a type of gut bacteria in mice, improving their immunity to cancer. The study shows that mice with higher levels of vitamin D resist tumor growth better and respond more effectively to immunotherapy.
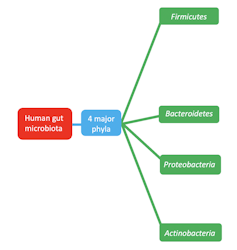
This effect seems linked to the increase of Bacteroides fragilis in the gut, which somehow enhances the mice’s immune response to cancer. Further research is needed to see if this applies to humans, as earlier studies suggest a potential link between vitamin D levels and cancer risk.
Key Facts:
- Vitamin D Role: Mice fed with vitamin D exhibited increased levels of Bacteroides fragilis, which helped them resist cancer better.
- Human Implications: Preliminary data analysis from 1.5 million people in Denmark hints at a correlation between low vitamin D levels and higher cancer risk.
- Future Research: Understanding how vitamin D can be utilized to boost the beneficial gut microbiome could open new pathways for cancer treatment and prevention.
Source: Francis Crick Institute
Researchers at the Francis Crick Institute, the National Cancer Institute (NCI) of the U.S. National Institutes of Health (NIH) and Aalborg University in Denmark, have found that vitamin D encourages the growth of a type of gut bacteria in mice which improves immunity to cancer.
Reported today in Science, the researchers found that mice given a diet rich in vitamin D had better immune resistance to experimentally transplanted cancers and improved responses to immunotherapy treatment.
This effect was also seen when gene editing was used to remove a protein that binds to vitamin D in the blood and keeps it away from tissues.
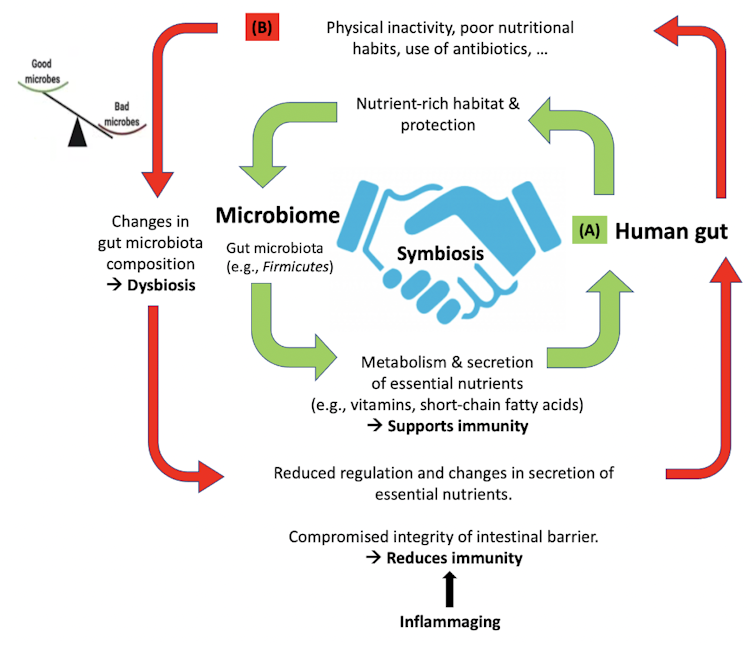
Surprisingly, the team found that vitamin D acts on epithelial cells in the intestine, which in turn increase the amount of a bacteria called Bacteroides fragilis. This microbe gave mice better immunity to cancer as the transplanted tumours didn’t grow as much, but the researchers are not yet sure how.
To test if the bacteria alone could give better cancer immunity, mice on a normal diet were given Bacteroides fragilis. These mice were also better able to resist tumour growth but not when the mice were placed on a vitamin D-deficient diet.
Previous studies have proposed a link between vitamin D deficiency and cancer risk in humans, although the evidence hasn’t been conclusive.
To investigate this, the researchers analysed a dataset from 1.5 million people in Denmark, which highlighted a link between lower vitamin D levels and a higher risk of cancer.
A separate analysis of a cancer patient population also suggested that people with higher vitamin D levels were more likely to respond well to immune-based cancer treatments.
Although Bacteroides fragilis is also found in the microbiome in humans, more research is needed to understand whether vitamin D helps provide some immune resistance to cancer through the same mechanism.
Caetano Reis e Sousa, head of the Immunobiology Laboratory at the Crick, and senior author, said: “What we’ve shown here came as a surprise – vitamin D can regulate the gut microbiome to favour a type of bacteria which gives mice better immunity to cancer.
“This could one day be important for cancer treatment in humans, but we don’t know how and why vitamin D has this effect via the microbiome. More work is needed before we can conclusively say that correcting a vitamin D deficiency has benefits for cancer prevention or treatment.”
Evangelos Giampazolias, former postdoctoral researcher at the Crick, and now Group Leader of the Cancer Immunosurveillance Group at the Cancer Research UK Manchester Institute, said: “Pinpointing the factors that distinguish a ‘good’ from a ‘bad’ microbiome is a major challenge. We found that vitamin D helps gut bacteria to elicit cancer immunity improving the response to immunotherapy in mice.
“A key question we are currently trying to answer is how exactly vitamin D supports a ‘good’ microbiome. If we can answer this, we might uncover new ways in which the microbiome influences the immune system, potentially offering exciting possibilities in preventing or treating cancer.”
Romina Goldszmid, Stadtman Investigator in NCI’s Center For Cancer Research, said: “These findings contribute to the growing body of knowledge on the role of microbiota in cancer immunity and the potential of dietary interventions to fine-tune this relationship for improved patient outcomes.
“However, further research is warranted to fully understand the underlying mechanisms and how they can be harnessed to develop personalized treatment strategies.”
This research was funded by Cancer Research UK, the UK Medical Research Council, the Wellcome Trust, an ERC Advanced Investigator grant, a Wellcome Investigator Award, a prize from the Louis-Jeantet Foundation, the Intramural Research Program of the NCI, part of the National Institutes of Health, CCR-NCI and the Danish National Research Foundation.
Research Information Manager at Cancer Research UK, Dr Nisharnthi Duggan said: “We know that vitamin D deficiency can cause health problems, however, there isn’t enough evidence to link vitamin D levels to cancer risk.
This early-stage research in mice, coupled with an analysis of Danish population data, seeks to address the evidence gap. While the findings suggest a possible link between vitamin D and immune responses to cancer, further research is needed to confirm this.
“A bit of sunlight can help our bodies make vitamin D but you don’t need to sunbathe to boost this process. Most people in the UK can make enough vitamin D by spending short periods of time in the summer sun.
“We can also get vitamin D from our diet and supplements. We know that staying safe in the sun can reduce the risk of cancer, so make sure to seek shade, cover up and apply sunscreen when the sun is strong.”

Abstract
Vitamin D regulates microbiome-dependent cancer immunity
A role for vitamin D in immune modulation and in cancer has been suggested. In this work, we report that mice with increased availability of vitamin D display greater immune-dependent resistance to transplantable cancers and augmented responses to checkpoint blockade immunotherapies.
Similarly, in humans, vitamin D–induced genes correlate with improved responses to immune checkpoint inhibitor treatment as well as with immunity to cancer and increased overall survival.
In mice, resistance is attributable to the activity of vitamin D on intestinal epithelial cells, which alters microbiome composition in favor of Bacteroides fragilis, which positively regulates cancer immunity.
Our findings indicate a previously unappreciated connection between vitamin D, microbial commensal communities, and immune responses to cancer.
Collectively, they highlight vitamin D levels as a potential determinant of cancer immunity and immunotherapy success.