By Dr. Mercola
CRISPR gene-editing technology brought science fiction to life with its ability to cut and paste DNA fragments, potentially eliminating serious inherited diseases. CRISPR-Cas9, in particular, has gotten scientists excited because,1 by modifying an enzyme called Cas9, the gene-editing capabilities are significantly improved. That’s not to say they’re perfect, however, as evidenced by a recent study that showed CRISPR may have significant unintended consequences to your DNA, including large deletions and complex rearrangements.2
Many of the concerns to date regarding CRISPR, or Clustered Regularly Interspaced Short Palindromic Repeat, technology have centered on off-target mutations. The featured study, published in Nature Biotechnology, looked at on-target mutations at the site of the “cuts,” revealing potentially dangerous changes that could increase the risk of chronic diseases like cancer.
Is CRISPR Scrambling DNA?
Researchers at the U.K.’s Wellcome Sanger Institute systematically studied mutations from CRISPR-Cas9 in mouse and human cells, focusing on the gene-editing target site. Large genetic rearrangements were observed, including DNA deletions and insertions, that were spotted near the target site.
They were far enough away, however, that standard tests looking for CRISPR-related DNA damage would miss them. The DNA deletions could end up activating genes that should stay “off,” such as cancer-causing genes, as well as silencing those that should be “on.” One of the study’s authors, professor Allan Bradley, said in a statement:3
“This is the first systematic assessment of unexpected events resulting from CRISPR/Cas9 editing in therapeutically relevant cells, and we found that changes in the DNA have been seriously underestimated before now. It is important that anyone thinking of using this technology for gene therapy proceeds with caution, and looks very carefully to check for possible harmful effects.”
The deletions detected were at a scale of “thousands of bases,” which is more than previously thought and enough to affect adjacent genes. For instance, deletions equivalent to thousands of DNA letters were revealed. “In one case, genomes in about two-thirds of the CRISPR’d cells showed the expected small-scale inadvertent havoc, but 21 percent had DNA deletions of more than 250 bases and up to 6,000 bases long,” Scientific American reported.4
The cells targeted by CRISPR try to “stitch things back together,” according to Bradley, “But it doesn’t really know what bits of DNA lie adjacent to each other.” As a result, the DNA may be rearranged, previously distant DNA sequences may become attached, or unrelated sections could be incorporated into the chromosome.5
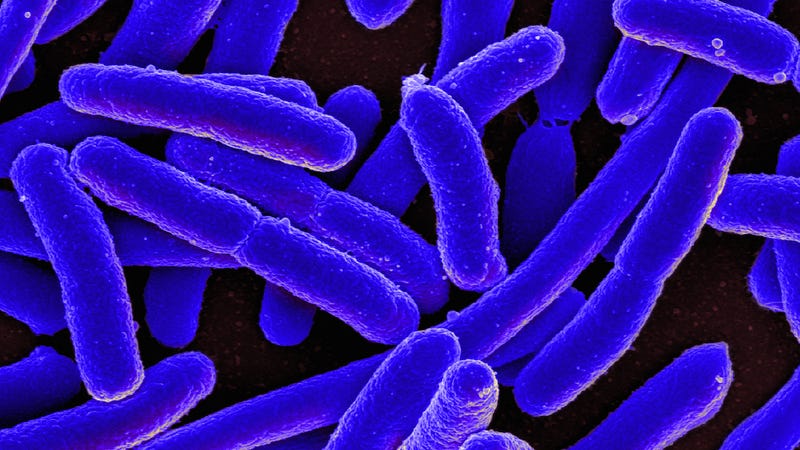
Cas9, a bacteria enzyme that acts as the “scissors” in CRISPR, actually remains in the body for a period of hours to weeks. Even after the initial DNA segment had been cut out and a new section “pasted” into the gap to repair it, Cas9 continued to make cuts into the DNA. “[T]he scissors continued to cut the DNA over and over again. They found significant areas near the cut site where DNA had been removed, rearranged or inverted,” The Conversation reported.6
Does This Mean CRISPR Isn’t Safe?
It’s too soon to say what the long-term effects of gene-editing technology will be, and there are many variables to the safety equation. The findings likely only apply to CRISPR-Cas9, which cuts through the DNA’s double strand. Other CRISPR technologies exist that may alter only a single strand or not involve cutting at all, instead swapping DNA letters.
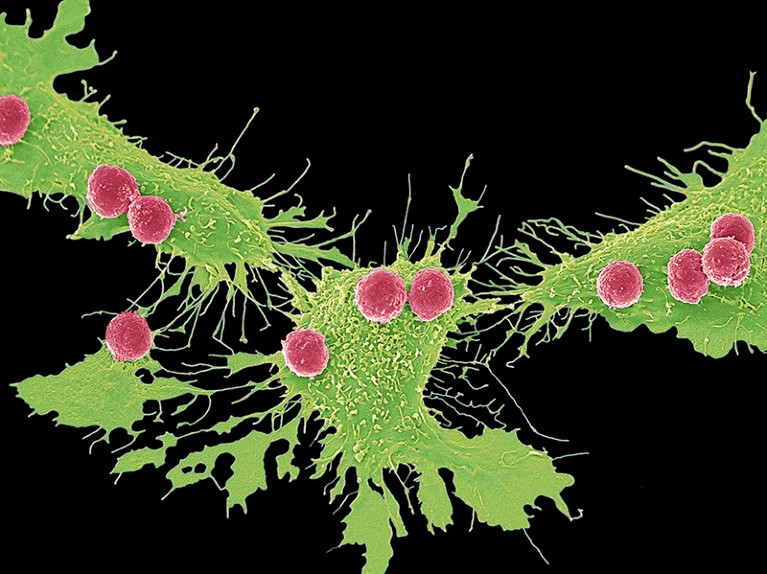
There are also CRISPR systems that target RNA instead of DNA and those that could potentially involve only cells isolated from the body, such as white blood cells, which could then be analyzed for potential mutations before being put back into the body.7
The Nature study did make waves in the industry, though, such that within the first 20 minutes of the results being made public three CRISPR companies lost more than $300 million in value.8
Some companies using CRISPR have said they’re already on the lookout for large and small DNA deletions (including one company using the technology to make pig organs that could be transplanted into humans). One company also claims it hasn’t found large deletions in their work on cells that do not divide often (the Nature study used actively dividing cells).9
The researchers are standing by their findings, however, which the journal took one year to publish. During that time, Bradley says, he was asked to conduct additional experiments and “the results all held up.”10 Past studies have also found unexpected mutations, including one based on a study that used CRISPR-Cas9 to restore sight in blind mice by correcting a genetic mutation.
The researchers sequenced the entire genome of the CRISPR-edited mice to search for mutations. In addition to the intended genetic edit, they found more than 100 additional deletions and insertions along with more than 1,500 single-nucleotide mutations.11 The study was later retracted, however, due to insufficient data and a need for more research to confirm the results.12
CRISPR-Edited Cells Could Cause Cancer
Revealing the many complexities of gene editing, CRISPR-Cas9 also leads to the activation of the p53 gene, which works to either repair the DNA break or kill off the CRISPR-edited cell.13
CRISPR actually has a low efficacy rate for this reason, and CRISPR-edited cells that survive are able to do so because of a dysfunctional p53. The problem is that p53 dysfunction is also linked to cancer (including close to half of ovarian and colorectal cancers and a sizable portion of lung, pancreatic, stomach, breast and liver cancers as well).14
In one recent study, researchers were able to boost average insertion or deletion efficiency to greater than 80 percent, but that was because of a dysfunctional p53 gene,15 which would mean the cells could be predisposed to cancer. The researchers noted, ” … it will be critical to ensure that [CRISPR-edited cells] have a functional p53 before and after engineering.”16
A second study, this one by the Karolinska Institute in Sweden, found similar results and concluded, ” … p53 function should be monitored when developing cell-based therapies utilizing CRISPR–Cas9.”17
Some have suggested that if CRISPR could cure one chronic or terminal disease at the “cost” of an increased cancer risk later,18 it could still be a beneficial technology, but most agree that more work is needed and caution warranted.
A CRISPR clinical trial in people with cancer is already underway in China, and the technology has been used to edit human embryos made from sperm from men carrying inherited disease mutations. The researchers successfully altered the DNA in a way that would eliminate or correct the genes causing the inherited disease.19
If the embryos were implanted into a womb and allowed to grow, the process, which is known as germline engineering, would result in the first genetically modified children — and any engineered changes would be passed on to their own children. A February 2017 report issued by the U.S. National Academies of Sciences (NAS) basically set the stage for allowing research on germline modification (such as embryos, eggs and sperm) and CRISPR, but only for the purpose of eliminating serious diseases.
In the U.S., a first of its kind human trial involving CRISPR is currently recruiting participants with certain types of cancer. The trial is going to attempt to use CRISPR to modify immune cells to make them attack tumor cells more effectively. As far as risks from potential mutations, it’s anyone’s guess, but lead researcher Dr. Edward Stadtmauer of the University of Pennsylvania told Scientific American, “We are doing extensive testing of the final cellular product as well as the cells within the patient.”20
Are ‘Designer Babies’ Next?
It’s easy to argue for the merits of CRISPR when you put it in the context of curing deafness, inherited diseases or cancer, and at least 17 clinical trials using gene-editing technologies to tackle everything from gastrointestinal cancer to tumors of the central nervous system to sickle cell disease have been registered in the U.S.21 Another use of the technology entirely is the creation of “designer babies” with a certain eye color or increased intelligence.
About 40 countries have already banned the genetic engineering of human embryos and 15 of 22 European countries prohibit germ line modification.22 In the U.S., the NAS report specifically said research into CRISPR and germline modification could not be for “enhancing traits or abilities beyond ordinary health.” Still, using gene editing to create designer babies is a question of when, not if, with some experts saying it could occur in a matter of decades.23
There are both safety and ethical considerations to think about. With some proponents saying it would be unethical not to use the technology. For instance, Julian Savulescu, an ethicist at the University of Oxford, told Science News he believes parents would be morally obligated to use gene-editing technology to keep their children healthy.
“If CRISPR could … improve impulse control and give a child a greater range of opportunities, then I’d have to say we have the same moral obligation to use CRISPR as we do to provide education, to provide an adequate diet …”24 Others have suggested CRISPR could represent a new form of eugenics, especially since it can only be done via in vitro fertilization (IVF), putting it out of reach of many people financially and potentially expanding inequality gaps.
On the other hand, some argue that countries with national health care could provide free coverage for gene editing, possibly helping to reduce inequalities.25 It’s questions like these that make determining the safety of CRISPR and other gene-editing technology more important now than ever before.
What Does a CRISPR-Enabled Future Hold?
We’ve already entered the era of genetic engineering and CRISPR represents just one piece of the puzzle. It’s an exciting time that could lead to major advances in diseases such as sickle-cell anemia, certain forms of blindness, muscular dystrophy, HIV and cancer, but also one that brings the potential for serious harm. In addition to work in human and animal cells, gene-edited crops, in which DNA is tweaked or snipped out at a precise location, have already been created — and eaten.
To date, the technology has been used to produce soybeans with altered fatty acid profiles, potatoes that take longer to turn brown and potatoes that remain fresher longer and do not produce carcinogens when fried. The latter could be sold as early as 2019.
The gene-editing science, in both plants and animals, is progressing far faster than long-term effects can be fully realized or understood. There are many opportunities for advancement to be had, but they must come with the understanding that unintended mutations with potentially irreversible effects could be part of the package.