A Stanford Medicine study identifies an easily measured biophysical property that can identify Type 2 diabetics at increased risk for liver cancer who don’t meet current screening guidelines.
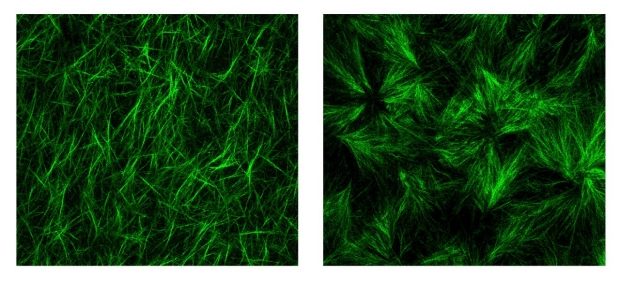
Collagen fibers in a three-dimensional hydrogel (left panel). When advanced glycation end products — a byproduct of poorly controlled diabetes — are added (right), the fibers are shorter and more cross-linked, creating conditions that favor cancer progression.
Weiguo Fan
For centuries, doctors have used their hands as essential diagnostic tools — exploring joints and palpating abdomens to assess a patient’s health. Often a cancer will reveal itself as a lump or unusual stiffness in a normally bouncy tissue or organ.
More recently, the relationship between stiffness and cancer has been documented through biophysical studies and clinical trials, particularly in liver and breast cancer. For example, stiffness is a primary hallmark of liver cirrhosis, which can progress to liver cancer.
Now researchers at Stanford University have shown that another biophysical characteristic known as viscoelasticity — think of how stretching a ball of Silly Putty or a clump of bread dough is met at first with resistance, and then with release — is even more tightly correlated with liver cancer than stiffness, particularly in people with Type 2 diabetes.
The distinction matters because people with Type 2 diabetes are two to three times as likely as people without diabetes to develop liver cancer, which often occurs in the absence of cirrhosis. Liver cancer rates are increasing in part because the prevalence of diabetes is growing worldwide, particularly in marginalized communities where healthy food choices and opportunities for regular exercise are scarce.
“This is the first time that the dogma of matrix stiffness as a primary predictor of liver cancer is being challenged,” said professor of gastroenterology and hepatology Natalie Torok, MD. “Current guidelines recommend routine liver cancer screening only for people with cirrhosis. As a result, many people with Type 2 diabetes are not screened at all. These new findings have major implications not just for liver cancer, but also other cancers for which diabetes is a risk factor, including breast cancers.”
Torok is the senior author of the study, which was published online Jan. 31 in Nature. Postdoctoral scholar Weiguo Fan, PhD, is the lead author.
Torok and her colleagues collaborated with researchers in the laboratory of associate professor of mechanical engineering Ovijit Chaudhuri, PhD, to investigate the role of viscoelasticity in liver cancer in patient samples, animal models and cells grown in the laboratory in a Jell-O-like tissue scaffolding called a hydrogel.
“This study is the first on the role of viscoelasticity in cancer with data that spans from humans and mouse models to in vitro 3D culture studies and computational simulations,” Chaudhuri said. “It definitively establishes the role of viscoelasticity in liver cancer progression.”
The study was supported by Stanford Medicine’s SPARK Program in Translational Research and its Innovative Medicines Accelerator, complementary programs meant to streamline the path of promising academic laboratory discoveries to clinical applications that benefit patients.
Stiffness test
Liver stiffness is measured non-invasively with imaging techniques called transient elastography or MR elastography involving a vibrating pad placed on the abdomen. The vibrations are transmitted from the imaging probe to the organ; the wave of vibration moving through a stiff medium differs from one moving through something more malleable. People with a liver stiffness that exceeds a certain threshold are diagnosed with liver cirrhosis; current guidelines recommend that they be screened every six months for liver cancer with an abdominal ultrasound and blood tests.
Measurements such as stiffness arise from what’s called the extracellular matrix — the space between and around an organ’s cells that is chock-a-block with proteins, sugars and minerals.
“Our organs are not just clumps of cells,” Chaudhuri said. “The cells exist in a scaffolding called the extracellular matrix that gives them physical support but also affects their maturation, specialization and functioning.”
Like a grade-school teacher, the matrix provides a physical framework that supports and organizes the cells, gentling and channeling them to harmoniously create a functional tissue. When the matrix is disrupted, any bad-apple cancerous or pre-cancerous cells more readily lose their way, spreading to places they shouldn’t; dividing uncontrollably; or morphing in to other, more dangerous versions of themselves.
People with diabetes have elevated levels of what are called advanced glycation end products, or AGEs. AGEs arise when blood sugar is poorly controlled and elevated levels of sugar molecules known as glucose begin to glom onto nearby proteins including collagen — a key structural component of the extracellular matrix. (AGEs are also present in protein- or fat-rich foods or in foods prepared at high heat such as frying or broiling.)
The researchers found that liver samples from people with Type 2 diabetes had higher levels of AGEs and were more viscoelastic — but no more stiff — than liver samples from people without Type 2 diabetes. A closer look in laboratory mice showed animals fed a diet high in AGEs had shorter and less interconnected collagen fibers in the liver’s extracellular matrix than those found in animals fed standard chow.
Next, the researchers studied how cells behaved when grown in the laboratory in a three-dimensional gel to mimic liver matrix structure. Tinkering with the cells outside the body allowed them to assess the effect of various changes in their growth and behavior.
“In our engineered hydrogels, we can tune one biophysical property such as viscoelasticity or stiffness at a time to understand how each property impacts the cells,” Chaudhuri said. “We saw that a change in viscoelasticity alone is enough to drive a more invasive behavior in the cells.”
In particular, the researchers noted that a more viscoelastic matrix promotes changes in liver cell shape and allows the formation of invasive protrusions on their membranes that help them escape natural barriers meant to keep cells in their rightful places.
Paradigm shift
Finally, Torok and her colleagues went one step further, dissecting a series of cellular signals that promote liver cancer progression in viscoelastic conditions that includes a cancer-associated protein called YAP.
“This is the first time that changes in collagen structure have been proven to promote viscoelasticity and liver cancer progression independent of stiffness,” Torok said. “It’s a complete change in paradigm that could explain the greater risk of liver cancer in people with Type 2 diabetes and may help select people should undergo regular liver cancer screening.”
Fortunately, like stiffness, viscoelasticity can be assessed non-invasively with MR elastography by changing a few parameters in vibration frequency and measurement. Torok is planning to launch a clinical trial to further study viscoelasticity, Type 2 diabetes and liver cancer progression.
“One of the major questions in medicine today is why people with diabetes and fatty liver disease are so prone to liver cancer, and how we can address this,” Torok said. “Our research suggests that many more people, particularly those with diabetes, should be screened for cancer. If we did that, perhaps we could act earlier and save lives.”
Researchers from Purdue University; Tsinghua University in Beijing; the University of Pittsburgh; the University of California, Davis; Albert Einstein College of Medicine; Keio University in Yokohama; and the University of Pennsylvania contributed to the work.


