The results of a study by New York University researchers explain why cancers can stop responding to kinase inhibitor drugs and may even come back stronger. By harnessing a range of analytical and computational techniques the team demonstrated how different gatekeeper mutations in fibroblast growth factor receptor (FGFR) tyrosine kinases affect the inactive state of the enzyme, destabilizing it by weakening the hydrophobic spine, and allowing the kinase to shift to the active form. The findings, they suggest, could inform which drugs oncologists might use as first-line therapy.
“If a treatment targets kinases that we know will ultimately mutate, it might be better to use a cocktail treatment right away that will still bind to the kinase, even if the gatekeeper is mutated,” said Nate Traaseth, PhD, professor of chemistry at NYU and co-senior author of the team’s published paper in PNAS, which is titled, “Gatekeeper mutations activate FGF receptor tyrosine kinases by destabilizing the autoinhibited state.”
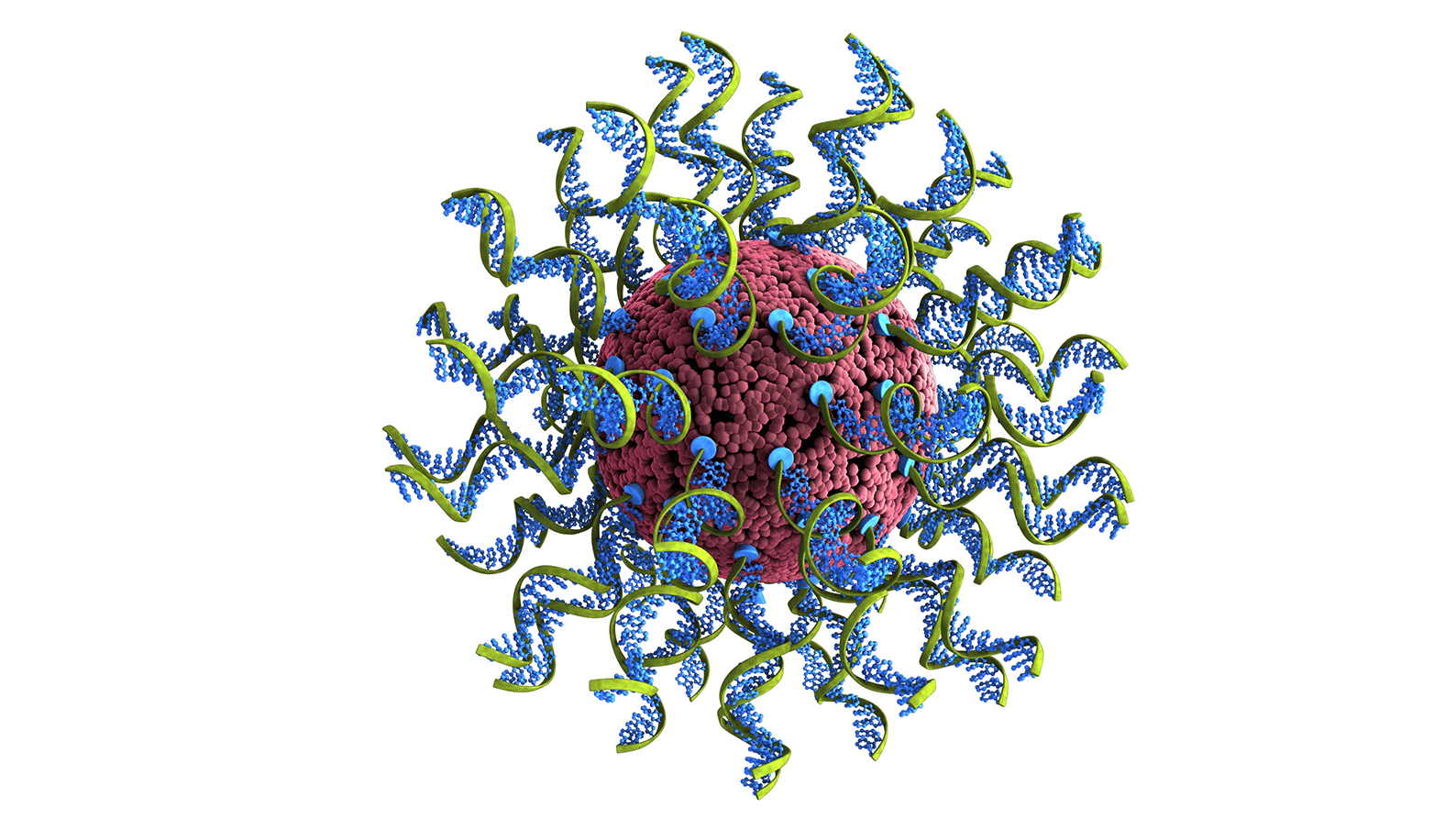
More than 70 FDA-approved cancer drugs are kinase inhibitors, which work by blocking kinases—enzymes that add phosphate groups to molecules in the cell—and preventing the chemical activity necessary for signaling and growth in cancer cells. “Intracellular and intercellular signaling by receptor tyrosine kinases (RTK) play essential roles in the regulation of cell growth, differentiation, metabolism, apoptosis, and senescence,” the authors explained. “Not surprisingly then, aberrant RTK signaling arising from amplifications, mutations, or their misexpression is implicated in a wide array of human developmental, metabolic and immune disorders, and cancer.” While kinase inhibitors can be very effective against cancer, over the long term, some patients experience aggressive cancer recurrence that is more difficult to treat and resistant to the original drug.
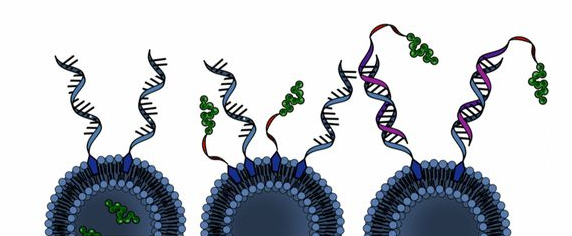
A leading cause of drug resistance—when a cancer no longer responds to a kinase inhibitor—is the emergence of genetic mutations, particularly those in a region in the kinase called the “gatekeeper” residue. The gatekeeper is deeply embedded in the kinase and allows or prevents access to an even-deeper hydrophobic (or water-repelling) pocket. “A major impediment to successful cancer therapy is the emergence of drug-resistant mutations at a residue within the kinase hinge region, which provides fitness advantages for tumor growth and hinders long-term remission,” the investigators continued.
Because kinase inhibitors work by binding to this hydrophobic pocket, mutations to the gatekeeper residue block a drug’s access, reducing its efficacy. But gatekeeper mutations also do something else that, according to the NYU researchers, may be even more important: they make kinases more active. “An underappreciated fact regarding gatekeeper mutations is that they elevate the kinase activity of the affected RTK,” the scientists stated. Alida Besch, a PhD student in NYU’s Department of Chemistry and the study’s first author, added, “When a kinase is switched into the active state, it can lead to processes like cells dividing, a hallmark of cancer. This increased activity is why we hypothesize that cancers come back even stronger, but exactly how gatekeeper mutations increase kinase activity is not well understood.” As the team further commented, “Understanding the molecular basis for this gain-of-function effect is important because the enhanced kinase activity of gatekeeper mutants correlates with greater signaling and worse patient outcomes.”
For their newly reported study the researchers focused on fibroblast growth factor receptors (FGFRs), a family of kinases that frequently mutates in different cancers, including lung and blood cancers. Treating FGFR-related cancers can involve using receptor tyrosine kinase inhibitors that bind to the hydrophobic pocket to block the receptor, which may effectively treat the cancer but also generate drug-resistant gatekeeper mutations.
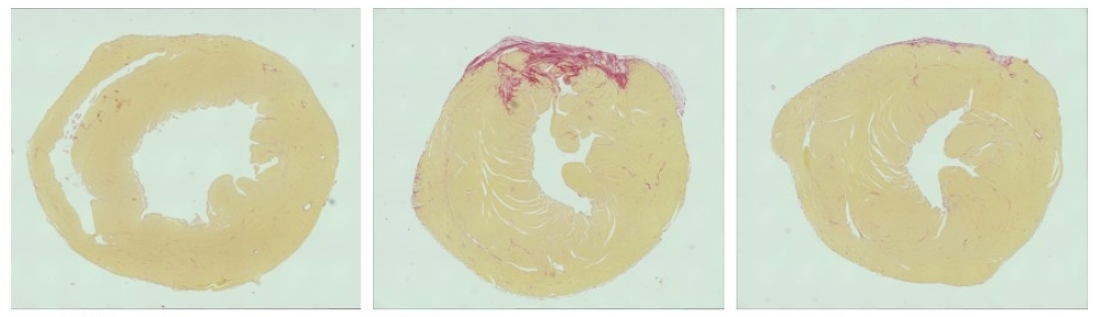
Using a multipronged approach, including kinase activity assays and nuclear magnetic resonance or NMR spectroscopy, together with computer simulations, the researchers studied FGFR kinases harboring two distinct gatekeeper mutations to determine how the kinase is made more active by the gatekeeper mutations.
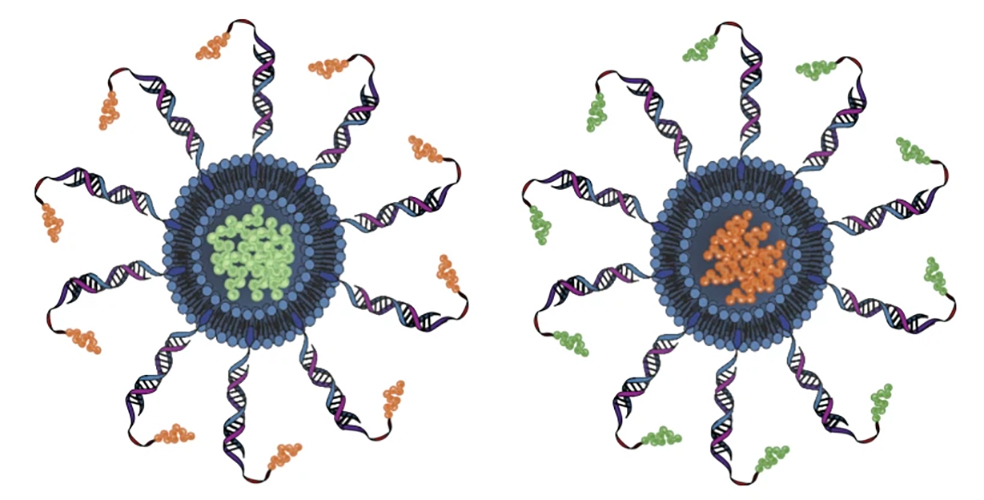
Kinases need to convert from an inactive to active state in order to function, and prior research suggested that gatekeeper mutations affect the kinase’s active state by strengthening and stabilizing the hydrophobic spine, a network of four residues connecting different areas in the kinase. But the experiments and simulations revealed a different story. The researchers discovered that the gatekeeper mutations of the FGFR kinase instead affect the inactive state of the kinase, destabilizing it by weakening the hydrophobic spine, and therefore allowing the kinase to shift to the active form. “We found that these mutations destabilize the autoinhibited conformation of the kinase by weakening the hydrophobic spine and modulating the conformation of the conserved DFG motif, thereby leading to the conclusion that gatekeeper mutations increase in the population of the active state,” they stated.
“This distinction—that gatekeeper mutations affect the kinase’s inactive state and destabilize it—is important, because we generally want receptor tyrosine kinases to be held in the inactive state. Switching into the active state would usually be dictated by external signals like hormones, not the kinase itself,” explained Yingkai Zhang, PhD, professor of chemistry at NYU and the Simons Center for Computational Physical Chemistry and the study’s co-senior author. “But if gatekeeper mutations are destabilizing the kinase and shifting it into its active form, this could explain why some cancers come back stronger.”
The findings could have implications for cancers with mutations in other tyrosine kinases, and potentially inform how clinicians choose which first-line cancer treatment to use—and whether a cocktail of drugs instead may be more effective at preventing recurrence. “ … the mechanism discovered for FGFR kinase may be applicable to gatekeeper mutations in other tyrosine kinases to subvert autoinhibitory mechanisms, leading to enhanced phosphorylation activity and increased clinical severity for patients possessing such mutations,” the researchers concluded.
“They are also considering how these findings could be used in the development of novel cancer therapeutics. One avenue they’re exploring is finding locations in the kinase other than the hydrophobic pocket for drugs to bind to, given not only the prospect of gatekeeper mutations but also that these pockets look so similar in the roughly 500 different types of human kinases, which limits the chances that a drug can precisely target certain kinases. “There’s not a single kinase drug on the market that only hits one type of kinase, although that is the goal,” Traaseth said. “Having drugs bind to different spots of the kinase that are more diverse than the hydrophobic pocket is one way to address this challenge.”