Consider it now “an option” for locally advanced disease, editorialists say

Six weeks of neoadjuvant chemotherapy for patients with operable colon cancer is safe and results in downstaging, increased complete resection rates, and better disease control at 2 years, according to results from the randomized FOxTROT trialopens in a new tab or window.
Patients allocated to neoadjuvant chemotherapy followed by 18 weeks of postoperative chemotherapy had a 16.9% risk of residual or recurrent disease within 2 years, compared with a 21.5% risk in patients who received the standard 24 weeks of postoperative chemotherapy only, reported Laura Magill, PhD, of the University of Birmingham in England, and colleagues.
This difference in favor of neoadjuvant therapy translated to a 28% relative reduction in 2-year recurrence (rate ratio [RR] 0.72, 95% CI 0.54-0.98, P=0.037), meeting the trial’s primary endpoint.
“FOxTROT results indicate that [neoadjuvant chemotherapy] then [adjuvant chemotherapy] may be superior to conventional postoperative chemotherapy,” Magill and co-authors wrote in the Journal of Clinical Oncologyopens in a new tab or window.
Relative reductions in colon cancer-specific and all-cause mortality appeared similar, but did not reach statistical significance:
- Colon cancer-specific mortality: RR 0.74 (95% CI 0.52-1.05)
- All-cause mortality: RR 0.76 (95% CI 0.55-1.06)
Initial results of the trial presented at the 2019 annual meeting of the American Society of Clinical Oncologyopens in a new tab or window, and reported as negative, showed a 2-year recurrence rate favoring neoadjuvant chemotherapy (13.6% vs 17.2%) that failed to reach statistical significance, owing to a lower-than-expected event rate in the control arm.
Still, in 2019, as well as with this updated report, trial investigators suggested that neoadjuvant chemotherapy should be considered a therapeutic option for locally advanced colon cancer.
In FOxTROT, patients with radiologically staged T3-4, N0-2, M0 colon cancer were randomly allocated (2:1) to 6 weeks of oxaliplatin-fluoropyrimidine preoperatively plus 18 weeks of therapy postoperatively (n=699), or 24 weeks postoperatively (n=354). Patients with RAS-wild-type tumors could also be randomly assigned 1:1 to receive panitumumab (Vectibix) or not during neoadjuvant chemotherapy.
Patients in the study had a median age of 63. Baseline CT suggested T4 disease in 25% of patients, and lymph-node involvement in 75%. The median follow-up was 3.1 years.
Of the patients allocated to have preoperative chemotherapy, 96% started and 87% completed therapy. Overall, 98.1% of patients in the neoadjuvant group and 99.2% of the patients in the adjuvant-only group underwent surgery.
Magill and co-authors also found:
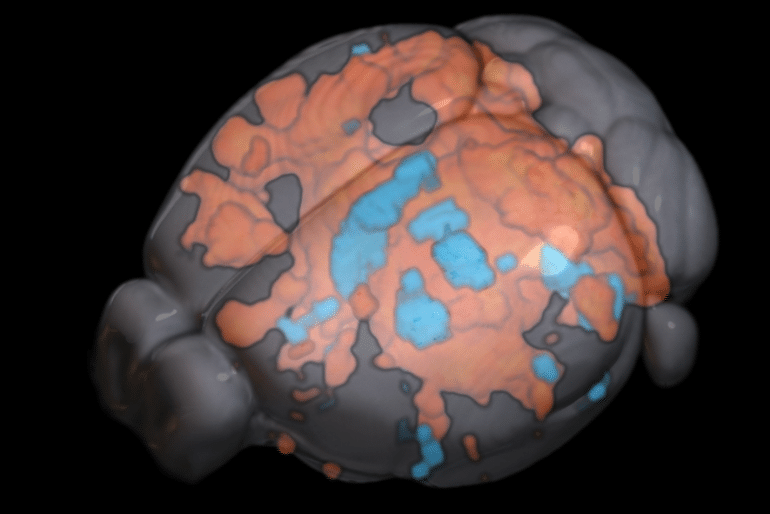
- Resection was more often histopathologically complete with neoadjuvant chemotherapy compared with adjuvant-only chemotherapy: 94% vs 89% (P<0.001)
- Neoadjuvant chemotherapy produced significant T and N downstaging and histologic tumor regression (P<0.001)
- Panitumumab did not enhance the efficacy of neoadjuvant chemotherapy in RAS-wild-type patients
Regarding tolerability, chemotherapy toxicity was comparable whether given before or after surgery, while surgical complications “were, if anything, less in the neoadjuvant chemotherapy group,” the authors reported.
In an editorial accompanying the studyopens in a new tab or window, Julien Taieb, MD, PhD, and Mehdi Karoui, MD, PhD, both of the Georges Pompidou European Hospital, Université Paris Cité, suggested that the question the gastrointestinal oncology community now needs to address is whether neoadjuvant chemotherapy represents a new standard for patients with locally advanced colon cancer.
The answer, Taieb and Karoui wrote, is that FOxTROT comes with several limitations, and that neoadjuvant chemotherapy should be considered “not a standard but an option.”
They emphasized that results from FOxTROT were initially reported as negative and have since become positive. This they attributed to “new statistical analyses incorporating new events mainly because of integration of data generated with CT scans done a bit later than 2 years.”
Moreover, while disease-free survival “has been accepted for 20 years as the most relevant endpoint for adjuvant CC [colon cancer] trials,” FOxTROT used a primary endpoint — the 2-year recurrence-free rate — that is not standard for adjuvant trials, Taieb and Karoui said.
Finally, they pointed out that staging preoperatively with a CT scan is associated with up to one-third of patients being overtreated for what is actually low-risk disease.
However, despite these and other limitations, “FOxTROT remains an important research effort,” the editorialists wrote. “The results convince us that [neoadjuvant chemotherapy] is feasible and safe and certainly not detrimental for patients. This opens a new avenue for preoperative treatments in patients with resectable CC.”