While onsite at the 2013 Annual Meeting of the American Psychiatric Association, Medscape spoke with Drs. Edward M. Kantor and Nolan R. Williams about the emerging new field of interventionalist psychiatry and their initiative to develop a training program.[1]
Background
Medscape: What is interventional psychiatry?
Dr. Williams: Interventional psychiatry is an emerging subspecialty that uses brain stimulation techniques to modulate the dysfunctional circuitry underlying medically resistant psychiatric diseases. Physicians who deliver procedures in the spectrum between standard care and surgery are sometimes referred to as “interventionalists” in other areas of medicine (eg, cardiology, radiology, and neurology). Currently, the field of psychiatry does not recognize interventionalists or offer formal training and certification. Our group is proposing the concept of “interventional psychiatrist” in place of procedure-specific terms such as “somatic therapist” or “ECT (electroconvulsive therapy) practitioner,” which fail to encompass the scope of brain stimulation strategies. It is not meant to replace current psychiatric therapies (medication and psychotherapy) but rather to enhance the practice of psychiatry with an additional set of tools. This can be viewed much in the same way that interventional cardiologists do not replace general cardiologists.
Dr. Kantor: I also see this bringing great opportunity for collaboration across neurology, neurosurgery, and psychiatry, which rarely occurs in other settings. This alone may advance our liaison activities and communication and, more than anything else, will facilitate better care between the disciplines and really help focus us on the whole person — mind, body, and brain — as opposed to one at a time, in isolation.
Medscape: How do you recommend that interventional psychiatry be incorporated into clinical training?
Dr. Kantor: It’s an emerging area of our field, where older techniques like ECT are being adapted for better efficacy with fewer side effects, and new techniques are coming of age. It’s not currently accredited on the training side, but my guess is that as it formalizes over the next 2-3 years, that process will naturally evolve. As a residency director, I support an educational plan that outlines minimum competencies, experience, and oversight. We already have begun exploring the paradigm with the American Association of Directors of Psychiatric Residency Training (AADPRT) and relevant specialty societies. I think the education has to begin with programs like ours at Medical University of South Carolina (MUSC), where the resources are more established, there are enough cases and mentors, and we can train practitioners and research scientists within psychiatry, in a way best suited to work within the existing graduate medical education framework.
A component of basic understanding and clinical exposure in residency would likely be the minimum expectation. On top of that, an optional, more formal track, using senior elective time, would be fairly easy to plan for within the existing training structure. Currently, not all programs have the expertise, but I believe that there is a desire among those that do to collaborate with needed tools like shared guidelines, online and remote learning, and course-based experiences. That said, I imagine that there will never be a one-size-fits-all plan that works in every institution.
Dr. Williams: Psychiatry is rapidly changing. New methods for noninvasively and invasively stimulating the brain have powerful therapeutic potential, but they require background knowledge (eg, circuits, physics of electricity) that is foreign to most psychiatrists. Interventional psychiatry is an emerging subspecialty that needs to be formally recognized and developed at various levels of psychiatric training. Academic centers will have to adapt to ensure adequate training to those who will be providing these neuromodulatory interventions, in order to avoid mistakes of an earlier era and to make sure that psychiatrists are the ones to perform the procedures, rather than other specialists who are clinically unfamiliar with the psychiatric disease management. Establishing formal training programs will ensure that psychiatry is ready to meet the challenges of treatment-resistant psychiatric illness with a properly trained cohort of interventional psychiatrists. We have an interventional psychiatry fellowship program at MUSC, and there are a few others starting around the country.
Approaches to Neuromodulation
Medscape: Can you walk our readers through the primary types of neuromodulation techniques used in psychiatry currently, and also in which conditions they are used, both on- and off-label?
Dr. Williams: Yes.
Transcranial magnetic stimulation (TMS): There are currently 2 different TMS coils that have been approved by the US Food and Drug Administration (FDA) for the acute treatment of depressed patients who have failed to respond to at least 1 antidepressant medication. Interventional psychiatrists need to understand the fundamental principles behind TMS and demonstrate competency in the delivery and programming of TMS paradigms. A recent multisite, naturalistic, observational study of acute treatment outcomes in clinical practice[2] demonstrated greater than 50% efficacy in sicker populations using TMS.
ECT: ECT is an effective acute treatment for a wide array of neuropsychiatric diseases (eg, depression, mania, psychosis) and remains the single most effective therapy for treatment-resistant depression (TRD). Although ECT has been used for nearly a century, advances in the way that it is delivered have greatly reduced side effects. Shorter pulse widths and unilateral electrode configurations have been shown to diminish cognitive side effects. Interventional psychiatrists should receive comprehensive ECT training that addresses indications and contraindications, length and timing of treatment, pulse programming, and maintenance therapy.
Focal electrically administered seizure therapy (FEAST): A new type of ECT has been developed, called FEAST. This unidirectional electrical stimulation with a novel electrode placement and geometry has been proposed as a means to initiate seizures in the prefrontal cortex prior to secondary generalization, but it is still in the research phase.[3]
Vagus nerve stimulation (VNS): VNS was FDA approved in 1997 to treat epilepsy, and in 2005 it became the first invasive neuromodulation device approved by the FDA as a treatment for a psychiatric disorder (chronic TRD). Unfortunately, VNS was FDA approved prior to any Class 1 evidence of efficacy; thus, insurance companies have been reluctant to reimburse for the implant. Nevertheless, the effects of VNS appear to be remarkably durable. Interventional psychiatrists should be the lead contacts on VNS consults and programming for TRD.
Deep brain stimulation (DBS): DBS is typically used to manage movement disorders but is now being investigated as a therapy for a variety of neuropsychiatric conditions such as obsessive-compulsive disorder (OCD), Tourette syndrome [still in research phase], addiction [still in research phase], and TRD [still in research phase]. In 2009, the FDA granted a somewhat controversial humanitarian device exemption for use of DBS for treatment-resistant OCD. Interventional psychiatrists will play a critical role in developing the field of functional neurosurgery for psychiatric disorders. Pertinent skills include patient consultation, intraoperative assessment, postoperative programming, troubleshooting, and integrating device settings with medications (psychopharmacology). There has also been an explosion in psychiatric side effects of DBS used for neurologic conditions like Parkinson disease. The interventional psychiatrist should be adequately trained to troubleshoot these issues.
Transcranial direct-current stimulation (TDCS): This is a therapy that involves an energy source that delivers a constant weak (typically ≤ 1 mA) electrical current through scalp electrodes. This therapy is not grandfathered in by the FDA as a device currently in practice, although other, similar devices are. A recent study[4] from Brazil demonstrated that when combined with sertraline, there is a synergistic effect in treating depression. There are limited data currently, but it seems to have great promise and low cost.
Putting Neuromodulation Into Practice
Medscape: Can you expand on how these techniques might be incorporated into care in conjunction with psycho- and pharmacotherapy?
TMS: In the pivotal trials, the patients were not on any medications. In the real world, TMS is typically combined with medications and therapy. There are now studies looking at combining therapy with TMS for a synergistic effect.
ECT: There are medications that, when used alongside ECT (venlafaxine/nortriptyline) or after ECT (lithium), increase the chances of improvement and better cognitive outcomes.
DBS: Typically this intervention can eventually replace medications; many of the studies reduced/removed medications once the device was working. In many instances, DBS (particularly in depression) will allow for patients to better participate in therapies that they would not have been able to participate in before.
TDCS: The most efficacy that has been shown to date is in combination with sertraline. This will potentially be a role for TDCS in enhancing therapeutic efficacy.
Medscape: Tell us about the interventional psychiatry training program at MUSC and how you envision the program evolving and affecting care.
Dr. Williams: Drs. Mark George and Baron Short have developed a 1-year interventional psychiatry fellowship with the first fellow, Dr. Jon Snipes, finishing June 30, 2013. A second fellow, Dr. Suzanne Kerns, will begin in July 2013.
We feel that interventional psychiatry should be present at 3 levels: (1) a core curriculum of introductory knowledge and experience during psychiatry residency training for all psychiatrists; (2) a neuromodulation elective track during residency at some locations; and eventually (3) a formal interventional psychiatry fellowship that leads to an approved subspecialty certification process under the American Board of Medical Specialties (ABMS).
Base resident education: Psychiatry residents should have an introductory-level understanding of the brain circuits underlying behavior and how they can be modulated using invasive and noninvasive brain stimulation. This fundamental knowledge should improve the quality of patient management by ensuring that patients are aware of the full complement of available therapeutic interventions. Ideally, all psychiatric residents would have a core curriculum that includes brain stimulation consultation and observation of ECT and TMS.
Interventional psychiatry track: Psychiatry residents who have a specific interest in brain stimulation should have the option of pursuing a dedicated training track within their residency program. Under this proposal, interested residents would be required to manage ECT and TMS treatment cases, from initial consultation to acute therapy and maintenance treatments. Psychiatrists who are currently performing these duties could be grandfathered into this arrangement.
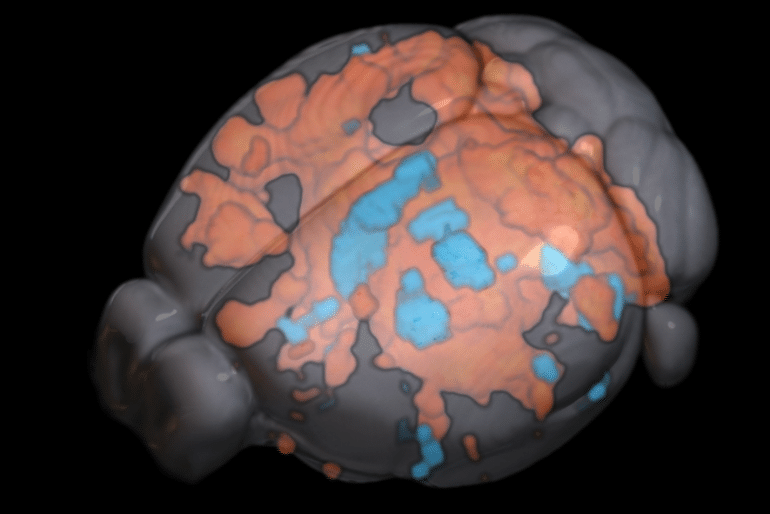
Interventional psychiatry fellowship: Psychiatrists who wish to pursue the most rigorous training program should have the option of pursuing a 1-year fellowship that includes focused training in all of the aforementioned techniques. This training would occur at institutions with robust neuromodulation programs in collaboration with neurology, neurosurgery, and neuroradiology. Fellowship trainees should receive hands-on exposure in established (ECT, TMS, DBS, VNS) and emerging (eg, TDCS) neuromodulatory technologies. Additionally, fellowship trainees should have experience with the tools used to measure the effects of neuromodulation, such as functional MRI and EEG.
Previous Page