Day: 12/19/2022
FDA OKs Bladder Cancer Gene Therapy
Less than one month after the FDA approved a gene therapy for hemophilia B, the agency today gave its OK to Ferring Pharmaceuticals for Adstiladrin (nadofaragene firadenovec-vncg). The product is a non-replicating adenoviral vector‑based gene therapy indicated for the treatment of adult patients with high-risk Bacillus Calmette-Guérin (BCG)-unresponsive non-muscle-invasive bladder cancer (NMIBC) with carcinoma in situ (CIS) with or without papillary tumors.

“This approval provides healthcare professionals with an innovative treatment option for patients with high-risk non-muscle invasive bladder cancer that is unresponsive to BCG therapy,” said Peter Marks, MD, PhD, director of the FDA’s Center for Biologics Evaluation and Research. “Today’s action addresses an area of critical need. The FDA remains committed to facilitating the development and approval of safe and effective cancer treatments.”
Bladder cancer is one of the more common forms of cancer. These abnormal cells can invade and destroy normal body tissue. Over time, the abnormal cells can also metastasize through the body. Most newly diagnosed bladder cancers (75–80%) are classified as NMIBC—a type of cancer that has grown through the lining of the bladder but hasn’t yet invaded the muscle layer. This type of cancer is associated with high rates of recurrence (30–80%) and the risk of progression to invasive and metastatic cancer.
Treatment and care of patients with high-risk NMIBC, including those with carcinoma in situ, or CIS (abnormal cancer cells found in the place where they first formed and that have not spread to nearby tissue), often involves removing the tumor and the use of BCG to reduce the risk that the cancer will recur. Few effective treatment options exist for patients who develop BCG-unresponsive disease.
Increased risk of disease worsening or death
The failure to achieve a complete response, or the disappearance of all signs of cancer as seen on cystoscopy, biopsied tissue, and urine, is associated with an increased risk of death or a disease-worsening event. Without treatment, the cancer can invade, damage tissues and organs, and spread through the body.
According to the Centers for Disease Control and Prevention, about 57,000 men and 18,000 women are diagnosed with bladder cancer annually, and roughly 12,000 men and 4,700 women die from the disease each year in the United States.
The safety and effectiveness of Adstiladrin was evaluated in a multicenter clinical study that included 157 patients with high-risk BCG-unresponsive NMIBC, 98 of whom had BCG-unresponsive CIS with or without papillary tumors and could be evaluated for response. Patients received Adstiladrin once every three months for up to 12 months, or until unacceptable toxicity to therapy or recurrent high-grade NMIBC.
Overall, 51% of enrolled patients using Adstiladrin therapy achieved a complete response (the disappearance of all signs of cancer as seen on cystoscopy, biopsied tissue, and urine). The median duration of response was 9.7 months. Forty-six percent of responding patients remained in complete response for at least one year.
Adstiladrin is administered once every three months into the bladder via a urinary catheter. The most common adverse reactions associated with Adstiladrin included bladder discharge, fatigue, bladder spasm, urinary urgency, hematuria, chills, fever, and painful urination.
Individuals who are immunosuppressed, or immune-deficient should not come into contact with Adstiladrin.
Lung Cancer, ‘Silent Killer’, Still Curable If Detected Early

Adenocarcinoma often begins along the outer parts of the lungs and is the most common type of cancer in people who have never smoked. (Shutterstock)
Lung cancer is often called “the silent killer,” because it can go unnoticed until reaching advanced stages when death is inevitable.
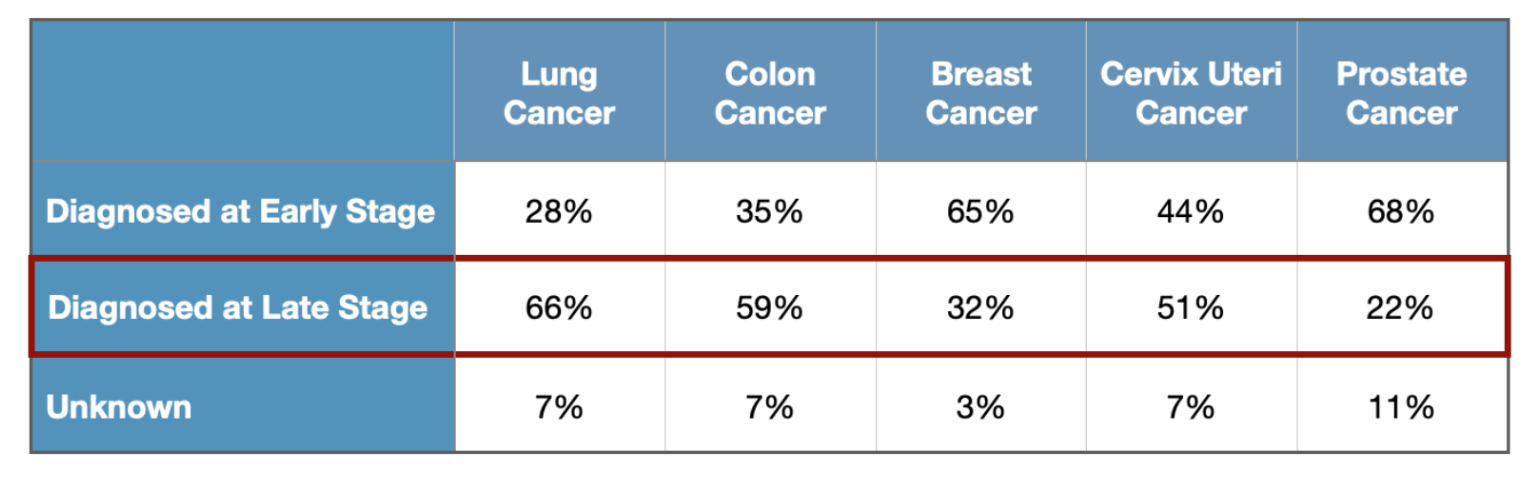
According to National Cancer Institute, 65.8 percent of lung cancer cases were diagnosed at a late stage, surpassing other common cancers like colon cancer, breast cancer, and prostate cancer.
“Other cancers give you signs and symptoms,” Raja M. Flores, MD, thoracic surgeon, and Chief of the Division of Thoracic Surgery at Mount Sinai Hospital., told The Epoch Times.
Lung cancer is different.
According to the American Lung Association (ALA), lung cancer is now the leading killer for both men and women in the U.S., and in 1987, it surpassed breast cancer to become the leading cause of cancer deaths in women.
Some Lung Cancer Patients Have Signs While Most Do Not
Many of the symptoms of lung cancer depend on location.
“When you have a tumor that’s closer to your trachea, you may cough up a little blood in early stage,” Flores said. “You may have a wheeze.”
However, the majority of lung cancers don’t occur centrally, near the trachea. Instead, they occur on the outer parts of the lung.
When it’s curable, you don’t know it’s there. Until it has spread.
That’s the biggest thing. “I think everybody tries to ask what signs should I look for—you’re not going to have signs,” said Flores.
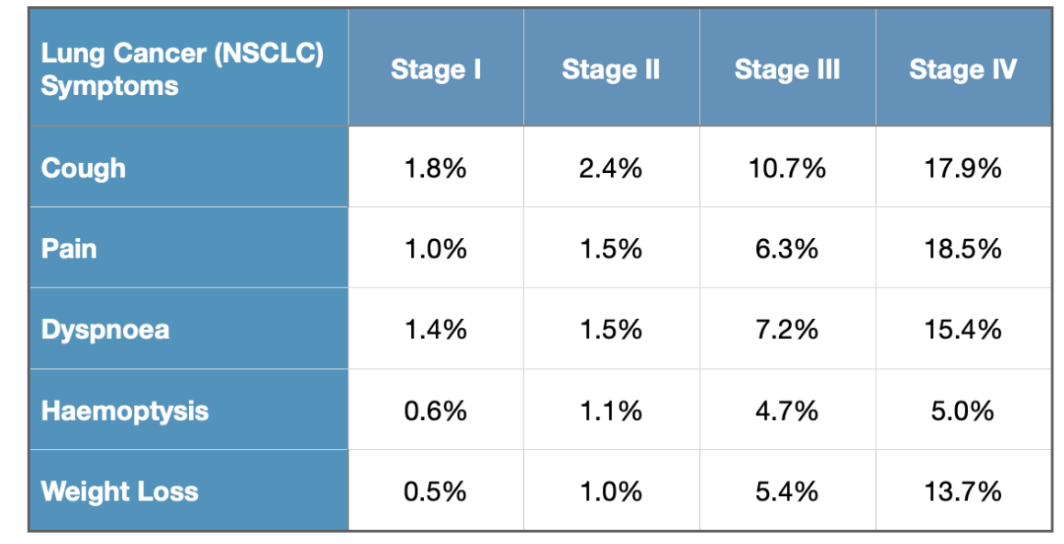
A 2020 Spainish study published in the European Society for Medical Oncology Open analyzed the symptoms of non-small cell lung cancer (NSCLC)—the most common type of lung cancer. The study involved nearly 10,000 patients. The result showed that at stage I, the most common symptom was coughing, however, only 1.8 percent of the patients showed this symptom. As the cancer progressed to stage IV, 17.9 percent of patients showed cough symptoms.
The other main type of lung cancer is small cell lung cancer. There are treatments for both types that carry relatively high survival rates if the disease is caught early.
Small cell is usually treated with chemotherapy unless it’s in its very early stage, called a small nodule stage one, when it can be removed surgically.
“But they usually do chemotherapy in addition to that and they’ll get a brain scan to make sure there’s nothing that’s spread to the brain,” Flores said.
Non-small cell lung cancer can be split into two categories—adenocarcinoma and squamous cell carcinoma. They make up about 80 to 85 percent of lung cancers.
“These tend to grow and spread more slowly,” said Aimee Strong, DNP, Nurse Practitioner, University of Virginia Thoracic Surgery, Lung Cancer Screening Program
Adenocarcinoma often begins along the outer parts of the lungs and is the most common type of cancer in people who have never smoked. However, squamous cell cancer can begin near the middle of the lungs.
Small cell lung cancer is almost always related to smoking. “It is fast growing and spreads quickly,” said Strong.
Smoking Is Not the Only Risk Factor
The degree of risk depends from person to person, and it’s not only smoking but also secondhand smoke that increases the odds of developing lung cancer.
“Let’s say you grew up in a household where mom and dad were smoking like chimneys, especially back in the seventies, you’re at risk,” Flores said.
Flores has had patients who were DJs back when clubs were full of cigarette smoke, who eventually developed lung cancer.
This isn’t the only problem.
“People from 9/11 who were exposed to the asbestos in the pulverized dust down there [are also at risk],” he said.
Besides, research published in European Respiratory Review, finds that there is a significant genetic component to lung cancer risk.
In China, lung cancer has been increasing over the past decades.
“There are some people who believe there’s a genetic component to it, [and] that you see [it] in the Chinese population,” said Flores. At the same time, “when you go there you realize that pollution is out of control.”
He noted it’s hard to say whether genetic or environmental factors play a bigger role, but tends to think this is due to the environmental conditions in China.
“I do believe that if you develop cancer, you got it from some external insult that caused the mutation in your system, that’s given you this cancer,” said Flores. “I don’t think it’s just bad luck.”
Early Detection Is ‘Very Curable’, Screening Is Essential
There are significantly more treatment options for lung cancer than were available even five years ago, and more sophisticated forms of radiation therapy to treat the disease.
When caught early, especially with the low-dose CAT scan, lung cancers are “very curable,” said Flores.
This even includes fast growing small cell lung cancers.
The problem is not that we don’t have a cure.
“We have a cure, 80 percent of the people with stage I will be cured,” Flores said. “The problem is that we don’t catch it early enough.”
He said the best solution is screening, and people who should be screened for lung cancer include:
- Current and former smokers
- People exposed to asbestos or radon gas
- Those with a family history of lung cancer
People who are at risk can see a lung physician, whether it’s a surgeon, a pulmonologist, a radiologist, or an internal medicine doctor.
Flores observed that many at risk due to previous smoking, now have families.
“They have this guilt that they smoked and how can you fix that guilt?” Flores asked. “Get a screening CAT scan.”
New CDC Report Attributes 3,500 Deaths in America to Long COVID

A person is tested for COVID-19 in New York City on May 3, 2022.
Long-term effects from COVID-19 infection, referred to as “long COVID,” are responsible for over 3,500 deaths in the first two and half years of the pandemic, according to a new government report.
The report (pdf), released Wednesday by the Centers for Disease Control and Prevention (CDC), is based on death certificate data for deaths that occurred in the United States from January 2020 through June 2022. The data were collected and processed by the National Center for Health Statistics, the CDC’s statistical data arm.
Overall, researchers found 3,544 death records that cited long COVID as a “cause or contributing factor of death.” This accounts for 0.3 percent of all 1,021,487 COVID deaths recorded during this period.
To identify long COVID-related deaths, researchers looked at death certificates that have both the cause-of-death code for COVID-19 and literal text with key terms such as “long COVID,” “post COVID,” “chronic COVID,” “long haul COVID,” “post-acute sequelae of COVID,” “PASC,” and others. The reason, according to the report, is that the cause-of-death code for post-COVID conditions has not yet been implemented in the United States at the time of this analysis.
The Findings
According to the report, people aged 75–84 accounted for the highest percentage of long-COVID-related deaths by age (28.8 percent), followed by those aged 85 and over (28.1 percent) and 65–74 (21.5 percent). By contrast, the highest percentage of COVID-19 deaths occurred among people aged 65–74 (23.8 percent) and 75–84 (23.5 percent), followed by those aged 50–64 (22.6 percent).
The report also shows that men (51.5 percent) accounted for a slightly higher percentage of long COVID-related deaths than women (48.5 percent). The age-adjusted death rate for long COVID was 7.3 per million people for males and 5.5 for females.
When it comes to racial demographics, the data shows that the majority of long COVID-related deaths occurred among non-Hispanic white people (78.5 percent), followed by black people (10.1 percent) and Hispanic people (7.8 percent). All other racial groups accounted for less than 2 percent of such deaths.
CDC Claims Undercounting
Given the way death certificates are filled out, the 3,544 figure could be an undercount, the researchers said.
“The study may underestimate long COVID deaths because clinical guidance for the identification and reporting of PASC has evolved over time and death certificate literal text may contain additional key terms that were not included in this study,” the report read.
“The investigation only included death certificates that listed COVID-19 as a cause of death, and as a result may underestimate deaths where prior COVID-19 infection was not confirmed or suspected but may have contributed to the death.”
Questionable Methodology
While researchers claim that long COVID is responsible for at least 3,500 deaths, critics question whether what the report used as statistical evidence actually points to that conclusion.
Dr. Vinay Prasad, a hematologist-oncologist and professor at the University of California, San Fransisco, took issue with the methodology and overall integrity of the analysis. He argued that just because certain key words are found on death certificates, it doesn’t necessarily mean that long COVID is as deadly as the report would make it seem.
“Imagine a person hospitalized with COVID, on the vent for 20 days, and then someone wrote [COVID-19] as the cause of death, and then casually said ‘post covid.’ This would be listed as a long covid death,” Prasad wrote in a blog post. “Are you serious?”
“[The CDC] didn’t interview providers,” he continued. “They didn’t review the medical record. They didn’t look in multiple datasets. They didn’t look across countries. They basically didn’t do anything a respectable scientist would before making such a bold, public claim.”
“This is widely used to craft a narrative that long covid can kill, but they have no such evidence,” the professor said.
According to the CDC, post-COVID conditions can include “a wide range of ongoing health problems” that can last weeks, months, or longer. Scientists still don’t know whether these health problems are caused by the virus itself, some other illness, or a combination of both.
In the meantime, the CDC said it’s trying to better identify the most frequent long COVID symptoms and the most common risk factors, better understand how many people are affected by long COVID, and how often people who have been infected with COVID-19 develop long COVID afterward.
Exercise, Mindfulness Don’t Boost Healthy Older Adults’ Cognition

“We aren’t saying, ‘Don’t exercise’ or, ‘Don’t practice mindfulness,’ ” Eric J. Lenze explains. “But we had thought we might find a cognitive benefit in these older adults. We didn’t.” (Ground Picture/Shutterstock)
Exercise and mindfulness failed to boost older adults’ cognitive function in a recent study.
Researchers studied the cognitive effects of exercise, mindfulness training, or both for up to 18 months in older adults who reported age-related changes in memory but had not been diagnosed with any form of dementia. The findings appear in JAMA.
“We know beyond any doubt that exercise is good for older adults, that it can lower risk for cardiac problems, strengthen bones, improve mood, and have other beneficial effects—and there has been some thought that it also might improve cognitive function,” says first author Eric J. Lenze, professor and head of the psychiatry department at Washington University School of Medicine in St. Louis.
“Likewise, mindfulness training is beneficial because it reduces stress, and stress can be bad for your brain. Therefore, we hypothesized that if older adults exercised regularly, practiced mindfulness, or did both there might be cognitive benefits—but that’s not what we found.”
Lenze and his colleagues still want to see whether there may be some cognitive effects over a longer time period, so they plan to continue studying this group of older adults to learn whether exercise and mindfulness might help prevent future cognitive declines. In this study, however, the practices did not boost cognitive function.
“So many older adults are concerned about memory,” says senior author Julie Wetherell, a professor of psychiatry at the University of California, San Diego. “It’s important for studies like ours to develop and test behavioral interventions to try to provide them with neuroprotection and stress reduction as well as general health benefits.”
The researchers studied 585 adults ages 65 through 84. None had been diagnosed with dementia, but all had concerns about minor memory problems and other age-related cognitive declines.
“Minor memory problems often are considered a normal part of aging, but it’s also normal for people to become concerned when they notice these issues,” says Lenze, who also directs Washington University’s Healthy Mind Lab. “Our lab’s principal aim is to help older people remain healthy by focusing on maintaining their mental and cognitive health as they age, and we were eager to see whether exercise and mindfulness might offer a cognitive boost in the same way that they boost other aspects of health.”
All study participants were considered cognitively normal for their ages. The researchers tested them when they enrolled in the study, measuring memory and other aspects of thinking. They also conducted brain-imaging scans.
The participants were randomly assigned to one of four groups: a group in which subjects worked with trained exercise instructors; a group supervised by trained experts in the practice of mindfulness; a group that participated in regular exercise and mindfulness training; and a group that did neither, but met for occasional sessions focused on general health education topics. The researchers conducted memory tests and follow-up brain scans after six months and again after 18 months.
At six months and again at 18 months, all of the groups looked similar. All four groups performed slightly better in testing, but the researchers believe that was due to practice effects as study subjects retook tests similar to what they had taken previously. Likewise, the brain scans revealed no differences between the groups that would suggest a brain benefit of the training.
Lenze says the study’s findings don’t mean exercise or mindfulness training won’t help improve cognitive function in any older adults, only that those practices don’t appear to boost cognitive performance in healthy people without impairments.
“We aren’t saying, ‘Don’t exercise’ or, ‘Don’t practice mindfulness,’” Lenze explains. “But we had thought we might find a cognitive benefit in these older adults. We didn’t. On the other hand, we didn’t study whether exercise or mindfulness might benefit older adults who are impaired due to dementia or to disorders such as depression. I don’t think we can extrapolate from the data that these practices don’t help improve cognitive function in anyone.”
Lenze says the researchers recently received funding from the National Institutes of Health (NIH) to continue following the group of adults who participated in this study.
“They are still engaging in exercise and mindfulness,” he says. “We didn’t see improvements, but cognitive performance didn’t decline either. In the study’s next phase, we’ll continue following the same people for five more years to learn whether exercise and mindfulness training might help slow or prevent future cognitive declines.”
The study had support from the National Institute on Aging, the National Center for Complementary and Integrative Health, the NIH Office of Behavioral and Social Science Research, and the McKnight Brain Research Foundation. Additional funding came from the Taylor Family Institute for Innovative Psychiatric Research.
Exposure to Spike Protein Impacts Women’sMaternal Healthand Maternal Health
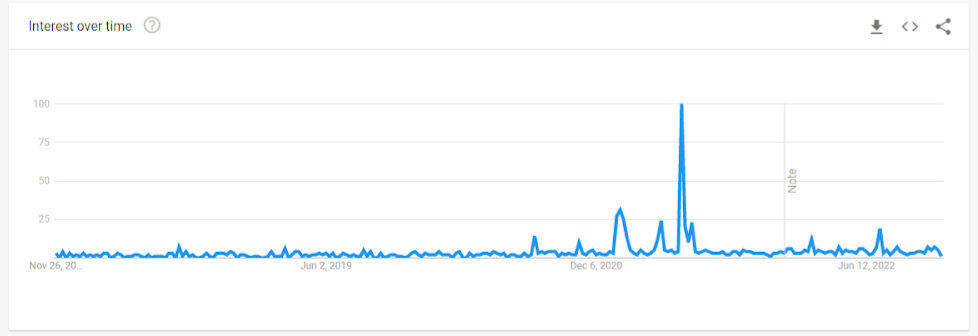
Unexpected rise of ‘decidual cast’ searches after COVID vaccine launch
(Shutterstock)
In late January, 2021, just a month after the Pfizer and Moderna COVID-19 vaccines were granted Emergency Use Authorization (EUA) by the Food and Drug Administration (FDA) in December 2020, a dramatic change in Google trend searches for “decidual cast” was evident.
Another surge in interest occurred in mid-June 2021, a month after the Pfizer vaccine was granted an expanded EUA for adolescents ages 12–15 years.
A decidual cast is defined as: “a large, intact piece of tissue that is passed through the vagina in one solid piece. It happens when the thick mucus lining of the uterus, called the decidua, sheds in the near exact shape of a uterine cavity, creating a triangular cast.”
Women began reporting unusual menstrual conditions on social media, including decidual cast shedding (DCS). This prompted several internet-based surveys, one of which was conducted by MyCycleStory.com.
While the literature contains only case reports of DCS, making the true prevalence difficult to measure, the condition is thought to be quite rare. Fewer than 40 cases have been published over the course of 100 years, usually related to ectopic pregnancy, miscarriage, or prolonged progesterone use.
However, 292 women reported experiencing DCS during a 7.5 month MyCycleStory study period in 2021.
Even though the absolute number of cases is not that high, this unusually increased incidence over the background rate requires further study to ascertain the cause, and any other potential contributors related to the pandemic.
Studies Observe an Impact on Women’s Menstrual Cycle
In the United States Vaccine Adverse Event Reporting System (VAERS), over 11,000 people self-reported a menstrual-related issue to the system following COVID-19 vaccination by April 2022. Events included heavy bleeding, irregular or delayed menstruation, oligomenorrhea, and amenorrhea.
Likewise, the United Kingdom’s Medicines and Healthcare Products Regulatory Agency (MHRA) yellow card surveillance scheme received 51,695 reports of menstrual disorders, including heavier or delayed periods, and unexpected bleeding, after the COVID-19 vaccine.
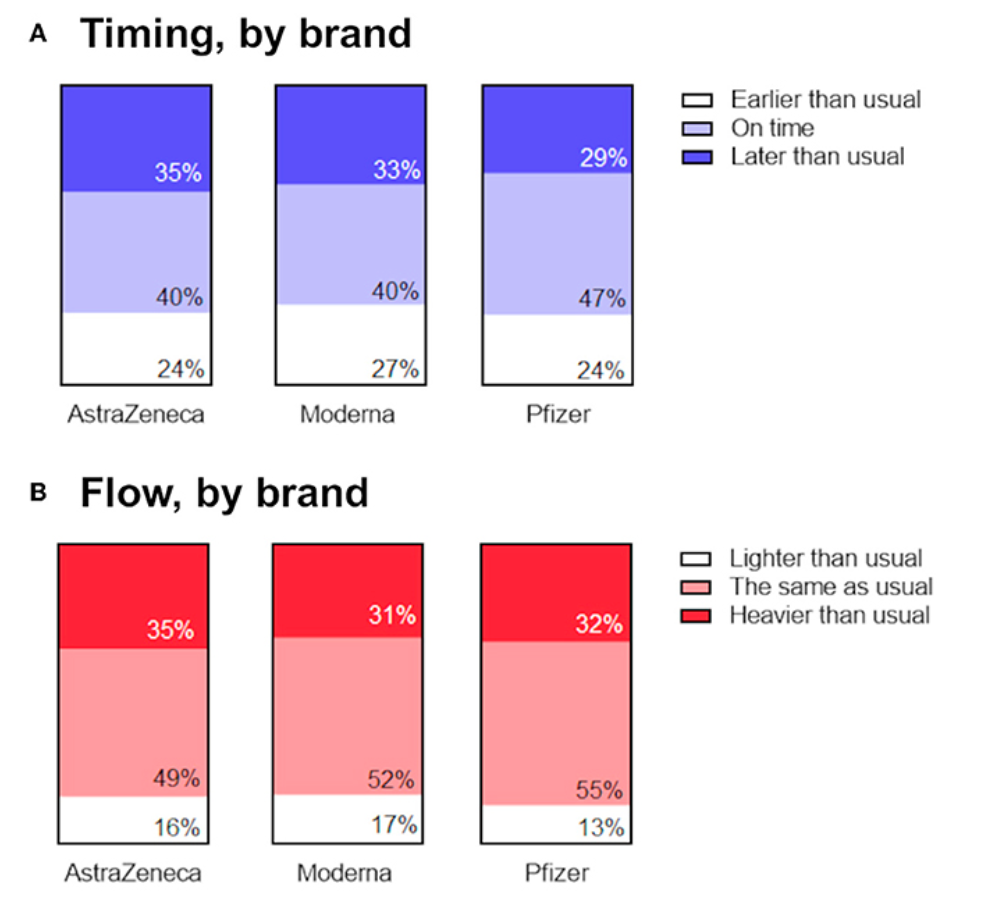
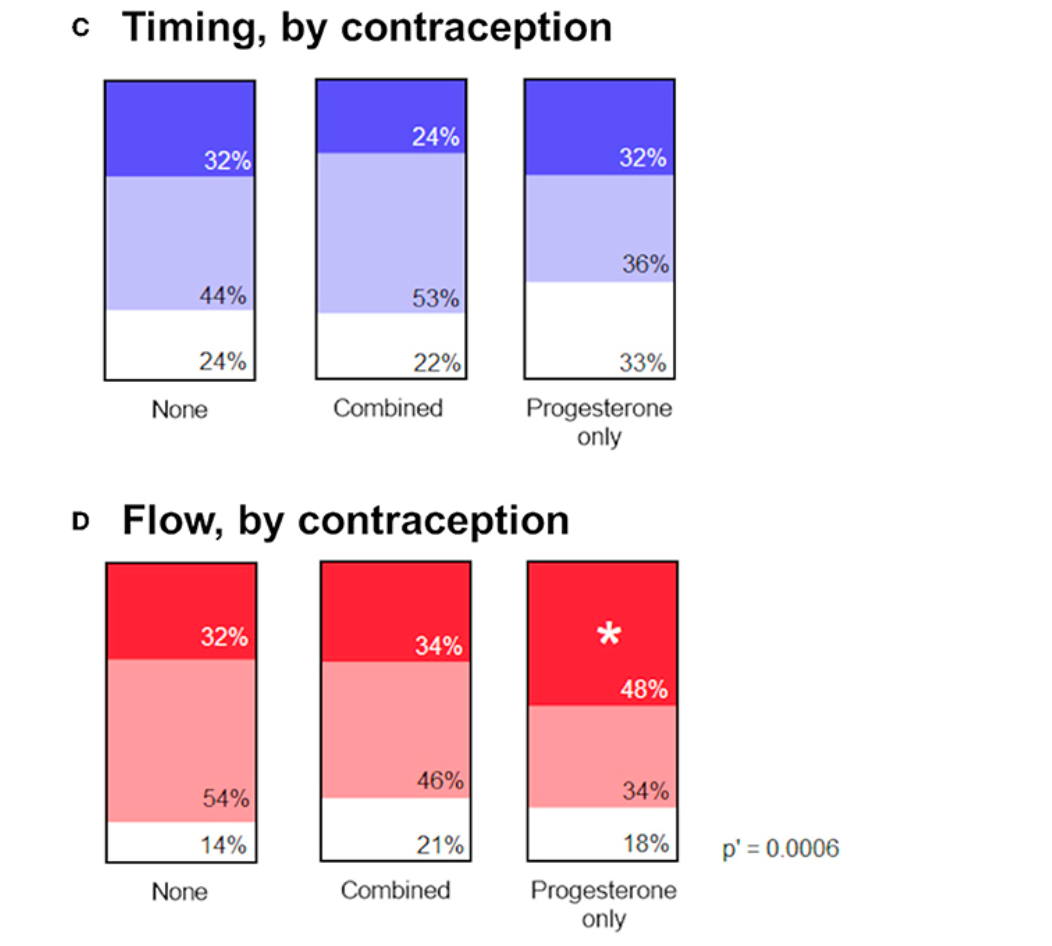
Findings from these databases suggested the possibility of negative impacts in menstrual cycles following COVID-19 vaccination. The relationship between COVID-19 vaccination and menstrual cycle has been evaluated in several peer-reviewed studies.
In a large prospective cohort study conducted by Harvard, the Apple Women’s Health study, cycle length was manually tracked by 9,682 vaccinated and unvaccinated women who contributed 128,094 menstrual cycles, most of whom were vaccinated (88 percent) with Pfizer (55 percent) or Moderna (37 percent). Both cycle length and menses length were tracked prospectively to capture baseline, vaccination, and follow-up measures.
This study found that mean cycle length did increase following vaccination, particularly for women who received their vaccine during the first two weeks of the cycle, during the follicular phase.
Following the first dose in the follicular phase, the cycle length increased by 0.97 days, and following the second dose by 1.43 days. The cycle remained longer for one to two months after vaccination then returned to baseline.
Women who were vaccinated during the luteal phase tended to have a shorter cycle (-0.97 days).
Another prospective United States cohort study of nearly 4,000 women ages 18 to 45 years evaluated those with normal cycle lengths for three consecutive cycles before the first vaccine dose and three post-vaccine cycles (cycles 4, 5, and 6). Those who were unvaccinated were evaluated over six cycles during a similar time period.
The investigators computed within-individual changes in cycle length and menses length for cycles 1–3 and 4–6 then used mixed-effects models to compare differences in cycle and menses length between the vaccinated and unvaccinated cohorts.
The investigators found a mean 0.91 day increase in mean cycle length for women receiving the mRNA vaccine during their second vaccine cycle.
More vaccine recipients had a cycle length change of at least 8 days than unvaccinated (6.5 percent vs 4.6 percent, p=0.017). The longer vaccine cycles seemed to be concentrated among the 358 individuals who received both doses within a single cycle.
In this subgroup of vaccinated women, the unadjusted mean cycle length increase was 2.38 days and a substantially larger proportion (10.6 percent) had an increased cycle length of at least 8 days compared with the unvaccinated cohort (4.3 percent, P<.001).
The authors found no difference in menses length between cohorts.
A smaller Israel study among 219 women regularly tracking cycles also found changes in menstruation reported by almost 40 percent of vaccinated women. Parity (number of pregnancies) and medication use seemed to be risk factors for menstrual irregularities.
Half of those suffering from irregular bleeding were multiparous versus 31.5 percent multiparity among women with no irregular bleeding. Presence of comorbidities was also higher among women reporting irregular bleeding.
Interestingly, women reporting regular medication use were less likely to report irregular bleeding.
Another study included both a prospective cohort of 79 women and a retrospective cohort of 1273 women.
The study did also find a cycle length increase (delay to the next period) in women cycling spontaneously, suggesting that COVID-19 vaccination can lengthen the menstrual cycle.
However, no such change was observed among those using contraception, suggesting that this effect of COVID-19 vaccination may be mediated by ovarian hormones.
While several studies (references 9–14) have suggested that COVID-19 infection can cause changes in cycle length, the Nurses’ Health Study did not detect such an association following COVID-19 infection.
In this study, COVID-19 vaccination was associated with cycle length in the short term (within 6 months of vaccination), particularly among women with short, long, or irregular cycles prior to vaccination. Changes in cycle length were detected for both mRNA and adenovirus-vectored vaccines.
A plausible connection between COVID-19 vaccination–both mRNA and adenovirus-vectored vaccines–and increased cycle length appears reasonable. The effect seems most pronounced among women who have already had a child and who receive both doses within a single cycle, which is consistent with the survey study from Israel.
VAERS Data Suggests Increased Risks of Menstruation and Pregnancy Irregularities
A preprint study of adverse events (AE) reported to the Vaccine Adverse Events Reporting System (VAERS) compared the ratio of AEs due to COVID-19 vaccines to influenza vaccines. Thorp and colleagues gathered data on pregnancy and menstruation irregularities reported to VAERS between Jan. 1, 1998 to June 30, 2022.
The reporting ratio for AEs related to COVID-19 vaccines compared to influenza vaccines were at least double (and statistically significant at p<0.05) for the following:
- menstrual abnormality (MA), miscarriage(M), fetal malformation (FM), fetal cardiac disorders (FCD), fetal growth abnormalities (FGA), fetal abnormal surveillance (FAS), fetal death/stillbirth (FS) and low amniotic fluid (LAF), which are listed In the below graph. A value greater than 1 implied that AE are reported more frequently with COVID-19 vaccine compared to influenza vaccines.
- fetal chromosomal abnormalities, fetal cystic hygroma, fetal arrhythmia, fetal cardiac arrest, fetal vascular mal-perfusion, fetal placental thrombosis, which are not included in the Figure but also significantly increased.
It should be noted that for any VAERS study, this is a passive reporting system which relies on physician reporting and may not reflect the true rate for the AE. Detection of AEs may vary significantly depending on public awareness of the AE, thus sensitivity may be as low as 1% percent of all AEs or 67 percent. Self-reports by patients are not necessarily confirmed by a physician diagnosis. The VAERS database is appropriate for hypothesis-generation, but population-based studies are needed to understand true incidence and causation.

Source of preprint: James A. Thorp, Claire Rogers, Michael P. Deskevich, Stewart Tankersley, Albert Benavides, Megan D. Redshaw and Peter A. McCullough. COVID-19 Vaccines: The Impact on Pregnancy Outcomes and Menstrual Function. Link of preprint.
Canadian Study Observed Increased Risks of Severe Adverse Events During Pregnancy
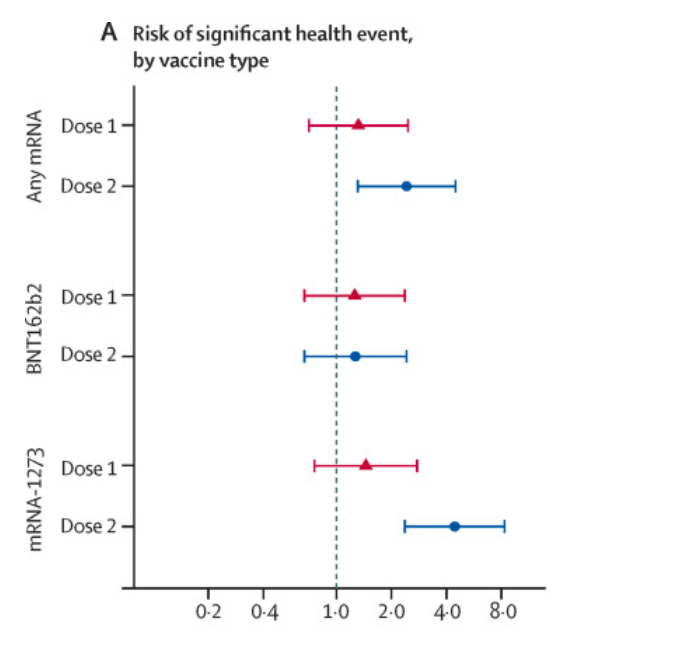
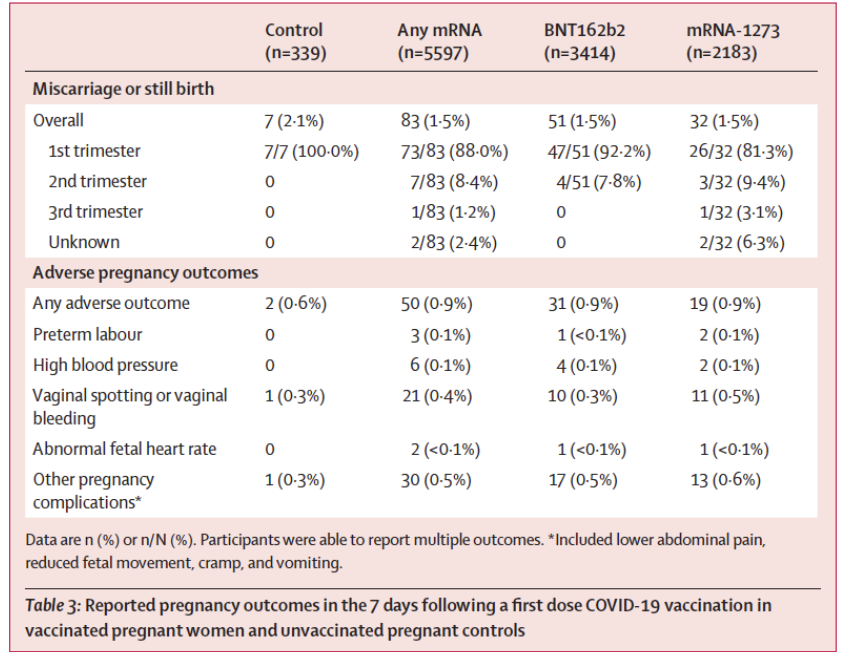
A Canadian prospective observational cohort study of COVID-19 vaccines, published in Lancet Infectious Disease pregnancy, evaluated the frequency of significant health events among 5625 pregnant / vaccinated, compared with 339 pregnant / unvaccinated and 185 735 nonpregnant / vaccinated controls, resulting a total of 191,360 women ages 15–49 years included.
The data were collected by survey with follow-up phone calls to those reporting any medically attended event.
The pregnant vaccinated females had a 4.4-fold (95 percent CI 2.4-8.3) increased risk of a severe health event after dose two of Moderna compared to pregnant unvaccinated females; this association was not seen for those vaccinated with Pfizer.
The dose of Moderna vaccine (100mcg) is more than 3 fold that of Pfizer (30mcg) in adults, which may well explain the different results among vaccine brands.
Miscarriage or stillbirth was the most frequently reported adverse pregnancy outcome. Both miscarriage and stillbirth describe pregnancy loss, but they differ according to when the loss occurs. In the United States, a miscarriage is usually defined as loss of a baby before the 20th week of pregnancy, and a stillbirth is loss of a baby at or after 20 weeks of pregnancy.
It was reported at similar rates between control (2.1 percent of 339) and vaccinated groups within seven days after dose one of any mRNA vaccine (1.5 percent of 5,597).
Other rare adverse pregnancy outcomes such as vaginal bleeding, abnormal fetal heart rate, and reduced fetal movement were increased slightly within seven days following any mRNA vaccination compared to control.
There were an additional individuals who reported experiencing miscarriage or stillbirth between the first COVID-19 vaccine dose and completion of the second (dose two) survey (up to 10 days after dose two), however the precise timing of these events relative to vaccination was not known.
Impact on Fertility
The impact of vaccination and infection on ovarian function and fertility is a heavy topic. The key findings from a number of peer-reviewed publications and preprints has been summarized here.
Reduced Total Fertility Rate (TFR)
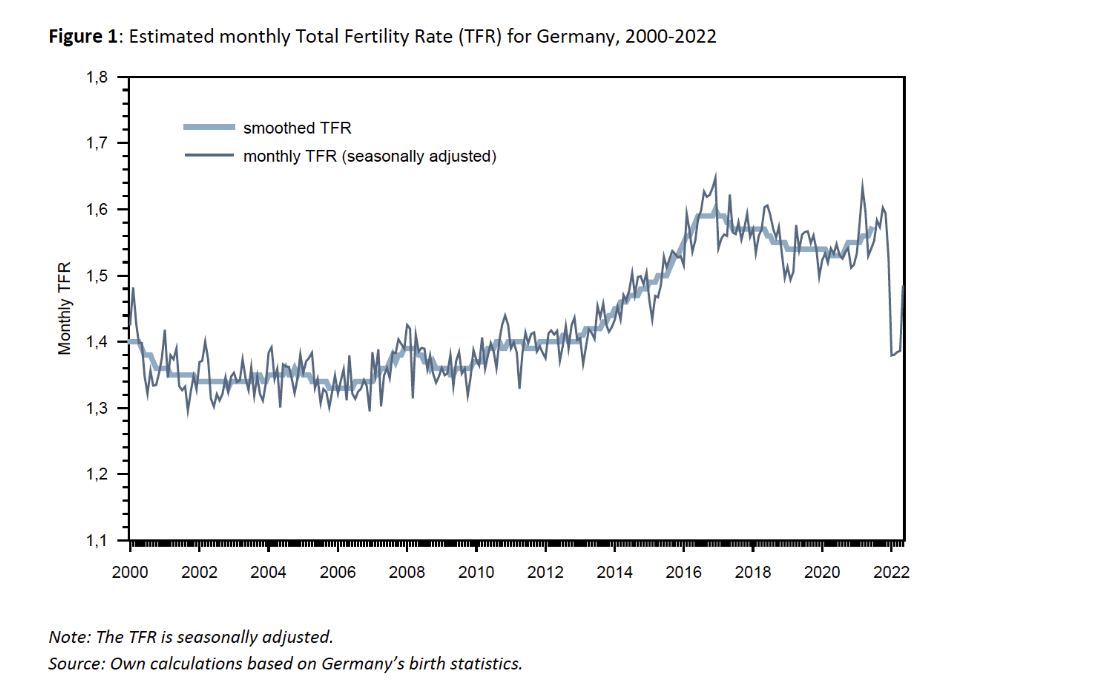
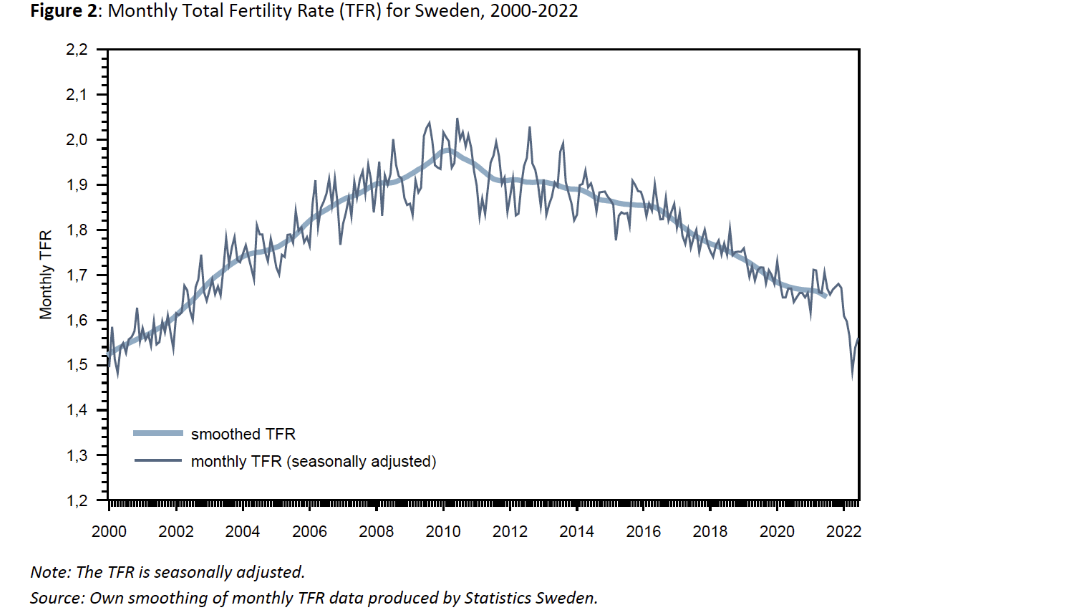
There is a population-wide change in fertility after vaccination campaigns. In a new preprint, the total fertility rate (TFR) in Sweden and Germany was trended over time, from early in the pandemic through 2022.
Many countries noticed a fertility decline early in the pandemic, but Germany and Sweden were largely unaffected. These countries, however, recently experienced a reduction in the TFR.
The seasonally-adjusted TFR in Germany declined 14 percent from 1.5-1.6 in 2021 to 1.3-1.4 in early 2022. A similar trend was seen in Sweden, with a 10 percent decline from 1.7 to 1.5-1.6.
The authors note that the sharp declines in TFR align with the onset of vaccination campaigns precisely nine months prior. The authors speculate that concerns about vaccine safety during conception and pregnancy might have caused women to hold off on starting their family until after vaccination.
Further population-based longitudinal research is necessary to detect any slight but significant effects of vaccination on fertility.
Pregnancy Rates
A systematic review and meta-analysis has evaluated the impact of COVID-19 vaccines on fertility
In the systematic review, 29 studies conducted in Israel, United States, Russia, China, Italy, North America, and Turkey were included.
The pregnancy rates were observed to decline in the vaccinated group by 15 percent for biochemical pregnancy rate and by 4.3 percent for clinical pregnancy rate, in a comparison to the unvaccinated group.
It is reported that both declines did not reach a statistical difference among vaccinated and not vaccinated groups. However, a clinical meaningful decline is not necessarily to be statistically significant. And whether to achieve a statistical difference or not may be confounded by the power of studies.
Furthermore, meta-analyses were performed for pre- and post-vaccination sperm progressive motility (44 percent versus 43 percent, p = 0.07).
Anti-Müllerian Hormone (AMH)
Anti-Müllerian hormone (AMH) has been used as a marker to assess ovarian function in women and it impacts fertility. It gives an estimate of ovarian reserve–how many eggs are remaining in the ovaries. Older women normally have lower levels than younger women.
In a prospective study conducted in Israel among 129 women who received two mRNA vaccines, the change in AMH was assessed via baseline and 90-day measurements, pre- and post-vaccination.
In this study, no change was detected in AMH levels pre- vs post-vaccination (5.3 vs 5.3 µg/l, respectively).
The authors concluded that while this study was limited to a three-month followup after the first vaccination, there did not appear to be any effect of mRNA vaccination on ovarian function.
Another similar but smaller Israeli prospective study among 31 women undergoing in vitro fertilization (IVF) treatment found that AMH remained stable pre- and post-mRNA vaccination.
There are limitations of the AMH studies. First, there is no control group and only self control was used.
Second, serum AMF levels are known to be affected by multiple factors including obesity, vitamin D levels, oral contraceptive therapies, genes (BRCA mutations contributing to breast and ovarian cancers), chemotherapy, common ovulatory disorders (polycystic ovary syndrome, PCOS), and history of ovarian surgery. Any potential changes in common confounding factors for serum AMF levels (body weight, contraceptives, vitamin D levels) in these subjects should be analyzed and reported.
In a retrospective study including 200 women undergoing IVF, no difference in fertility outcomes was detected, including oocyte retrieval, fertilization and pregnancy rates, and embryo quality.
Although this study found similar pregnancy rates between vaccinated and unvaccinated (32.8 percent and 33.1 percent, respectively), it would have required a much larger sample size to detect a small but meaningful difference.
A sample of at least 985 participants would be needed to detect a smaller 5 percent difference in pregnancy rates. In other words, this study was underpowered to detect a meaningful difference of reduction in pregnancy rates.
In another retrospective cohort study of 222 vaccinated and 983 unvaccinated women who underwent ovarian hyperstimulation, no effect of vaccination was found for the primary outcome, fertilization rate, nor any of the secondary outcomes, including eggs retrieved, mature oocytes retrieved, mature oocyte ratio, blastulation rate, or euploid rate.
For 214 vaccinated and 733 unvaccinated women undergoing frozen-thawed euploid transfer, the adjusted analysis found no significant association for vaccination and the primary outcome, clinical pregnancy (adjusted odds ratio [aOR] 0.79, 95 percent CI 0.54-1.16), nor any of the secondary outcomes: pregnancy (aOR 0.88, 95 percent CI 0.58-1.33), ongoing pregnancy (aOR 0.90, 95 percent CI 0.61-1.31), biochemical pregnancy loss (aOR 1.21, 95 percent CI 0.69-2.14), or clinical pregnancy loss (aOR 1.02, 95 percent CI 0.51-2.06).
However, these confidence intervals are large and the sample size insufficient to rule out a small but clinically meaningful difference in outcomes.
A small cohort study of 32 individuals (9 recovered SARS-CoV-2 positive, 9 vaccinated, 14 uninfected/unvaccinated) found no differences in follicular function and oocyte quality.
Together, these studies suggest that any effect of either infection or vaccination on fertility will be difficult to detect unless studies are designed with sufficient statistical power geared to expected changes in primary and secondary endpoints.
A decrease of 0.3 percent in the vaccinated group is 30 fewer pregnancies per 10,000 women, thus any study designed to detect a difference this slight would need to enroll 770,000 women.
Some might suggest powering phase III clinical trials to detect fertility impact is impractical, but certainly intentional post-marketing surveillance when vaccine uptake is in the millions is possible.
Mechanism of Action of AEs in Reproductive Health
A number of molecular mechanism of actions have been discussed which may contribute to the AEs observed in women.
First, immune activation following exposure to spike protein after vaccination might trigger an abnormal innate immune response, activate inflammatory cytokines and inflammatory genes.
Second, the spike protein induced local and systemic inflammation might impact the signaling between the brain and ovaries (the hypothalamus-pituitary-adrenal or HPA axis), resulting in hormone imbalances, prolongation of follicular recruitment during the early part of the cycle, and lengthening the cycle.
On the other hand, vaccination during the luteal phase may suppress growth of the endometrial lining and affect endometrial stability, thus shortening the cycle.
Third, ovarian inflammation may also be caused by lipid nanoparticles (LNP) effects on hormones, an autoimmune reaction with anti-syncytin antibodies at the endometrium, or inflammatory processes triggered by the spike protein either from the vaccine or infection.
Fourth, abnormal bleeding can be caused by abnormal local clotting in the endometrium during the period.
A large body of evidence has shown that the spike protein can trigger the clotting cascade via inducing endothelial disruption, inflammation of endothelial cells, massively released activated vWF, overactivating platelet, fibrous network from neutrophil extracellular traps (NETs), as well as increasing angiotensin II level, activating Toll-like receptor 4, all adding up to initiate blood clotting cascades.
Meanwhile, spike protein disrupts the clot dissolving mechanisms through inducing resistance to fibrinolysis, competitive binding to heparan sulfate, as well as forming an amyloid-like substance.
Based on the evidences of spike protein’s domino-like activities related to abnormal blood clotting, the potential role of spike protein originating from SARS-CoV-2 or COVID-19 vaccine in the abnormal bleeding of vaccinated women is likely to contribute to the surge of increased DCS and menstrual disorders during COVID pandemic, amongst other dysregulated immune and hormone mediated pathologies.
Impact on Lactation: Antibodies Detected in Milk and Symptoms Reported
A prospective cohort study included 50 lactating women who received mRNA vaccines with both blood and milk samples prior to their first vaccination dose, immediately prior to dose two, and four to ten weeks after their second dose.
Anti-SARS-CoV-2 receptor binding domain (RBD) antibodies were measured in each sample, and blood samples were collected from a subset of infants whose mothers were vaccinated while lactating.
After vaccination, levels of anti-SARS-CoV-2 IgG and IgM significantly increased in maternal plasma and there was significant transfer of IgA and IgG antibodies to milk.
Self-reported symptoms (fever, chills, headache, joint pain, muscle aches or body aches, and fatigue or tiredness) were reported by significantly more participants after the 2nd dose than after the 1st dose.
Two mothers reported slightly less milk production in the first 24-72 hours after vaccine doses.
Twelve percent of infants were reported with at least one symptom after the 1st maternal vaccine dose, which are primarily gastrointestinal symptoms and sleep changes.
The study lacked an unvaccinated control and these changes in infant behaviors are common; future studies should evaluate these reports.
The study also collected symptoms following vaccination and noted that more vaccine-related side effects may be experienced by those receiving Moderna compared to Pfizer, which should be again attributed to the higher dose of Moderna.
Natural Immunity Impact on Lactation
Finally, a study of mothers recently recovered from SARS-CoV-2 infection evaluated both antibodies and T cells in breastmilk. Because only about one in four women elect to be vaccinated during pregnancy, the ability of the mother to confer passive immunity to her infant through breast milk is an important question to assess.
In this small study of 30 lactating women, both antibody and T cell parameters were evaluated in milk samples collected at 12 timepoints over the course of a month.
A second set of samples were donated four months after a positive SARS-CoV-2 test to test durability of the immune markers.
The study confirms that women recently infected with SARS-CoV-2 have antibodies in their milk which can neutralize the spike complex. The milk is also enriched with mucosal memory T cells.
This study may be the first to demonstrate that breast milk from mothers who have recovered from SARS-CoV-2 infection contains long-lasting IgA and IgG antibody responses and that breastmilk can provide passive protection to the infant via mucosal-homing, effector-memory T cells which can seed the infant gastrointestinal tract.
Summary of Key Observations
Based on the available data collected from clinical studies, vaccine safety databases or surveys, a summary of key observations include:
- Concerns about the negative impacts of COVID-19 vaccination on the menstrual cycle have been validated by peer-reviewed research.
- The cycle length appears to increase following both mRNA and adenovirus-vectored vaccination, particularly for those women who received both doses within a single cycle (21-28 day interval), and those who were vaccinated during the follicular phase.
- VAERS data suggests increased risks of menstruation and pregnancy irregularities. A Canadian study also observed increased risks of severe adverse events during pregnancy associated with the Moderna vaccine.
- Sharp decline of total fertility rates were reported in Germany and Sweden in 2022. A 15 percent decline in the biochemical pregnancy rate and a 4.3 percent decline in the clinical pregnancy rate were reported, though AMU studies did not detect any meaningful change.
- Spike protein induced inflammation, immune disorders, and hormone mediated mechanisms of action as well as abnormal clotting cascades and overactivation have been correlated to these clinical adverse events.
- COVID vaccine induced antibodies have been detected in milk, as well as symptoms among mothers and infants post vaccination are reported.
- The effect has been observed across spike protein-based COVID-19 vaccines regardless of vaccine type. The higher dose mRNA vaccine (Moderna) is associated with a higher likelihood of these events than the lower dose mRNA vaccine (Pfizer).
These findings strongly suggest that more rapid and intentional post-marketing surveillance is necessary to detect impacts of vaccination on menstrual, pregnancy, and lactation events.
The CDC continues to recommend vaccination and boosters for all individuals over 5 years of age despite a lack of evidence regarding an incremental reduction in serious COVID-19 illness among those younger than 40 years of age.
To address vaccine hesitancy, public health officials and regulatory agencies must demonstrate that individual concerns are addressed and that clinical trials are designed to detect rare adverse events in otherwise healthy, young individuals prior to issuing broad recommendations.
A phased trial rollout which prioritizes enrollment of higher risk individuals and follows them for clinically important endpoints, such as hospitalization and death, would allow rapid deployment of lifesaving vaccines while minimizing harm to those at low risk of serious illness.
New Test Detects 14 Cancer Types at Stage I, When Most Curable

Using the GAGs test, patients with undetected cancer showed a 39 to 50 percent lower risk of death, and the test predicted cancer location with 89 percent accuracy. (Roman Zaiets/Shutterstock)
Cancer is difficult to cure in later stages, so early detection is essential to curing the disease. New research finds an early detection method for many cancers that could significantly improve cancer survival rates.
Cancer Growth May Rely On Metabolic Changes
Increasing evidence has shown that cancer cells’ rapid growth relies on a shift in their metabolism.
Glycosaminoglycans (GAGs) are a type of sugar that plays an important part in metabolism. A 2016 study by Gatto indicated that these sugars were excellent biomarkers to non-invasively detect kidney cancer.
Francesco Gatto, Ph.D., study author from Chalmers University of Technology told The Epoch Times, GAGs feature structural changes in the blood and urine that appeared to be “a universal signature” across cancer types.
This signature was detectable in very small, stage I cancers.
Gatto and his team tested this marker across 14 cancer types, said Gatto. They developed a machine learning method that used algorithms to detect changes in GAGs that indicated cancer.
New Test Has Up to 62 Percent Sensitivity to Stage I Cancer
The study included 1,260 healthy and cancer-diagnosed participants experiencing one of 14 cancer types. 34 percent of the patients had stage I—low-grade cancer.
When doing the test, only small amounts of blood or urine were required, making this method practical and inexpensive.
Gatto and his team first found the technique accurately detected the 14 cancer types they tested for, with up to 62 percent sensitivity to stage I disease.
They then discovered that twice as many stage I cancers in asymptomatic, healthy people could be detected, compared to DNA-based Multi-Cancer Early Detection (MCED) tests currently under development, which work by detecting genetic fragments from tumors that are found in the blood.
Using the GAGs test, patients with undetected cancer showed a 39 to 50 percent lower risk of death, and the test predicted cancer location with 89 percent accuracy.
Gatto said they still don’t fully understand why this happens.
“However, the data quite clearly shows that the more extreme the GAG changes, the worse is the prognosis for cancer patients,” he noted. This may suggest cancers that affect GAGs are biologically very aggressive.
Current Tests Don’t Detect Enough Early Cancers
Current screening tests are cancer-type-specific, meaning patients are tested separately for each cancer type.
Current screening techniques rely on either direct visualization of cancer, followed by a biopsy or a blood or stool test, indicating that cancer is likely. The requirement for imaging is expensive and requires travel to a hospital or imaging center as well as specific expertise.
The interpretation of imaging results also depends on the skill of the individual who is either doing the colonoscopy, reading the mammogram, or a computerized tomography (CT) scan.
However, these methods only detect some kinds of cancer and aren’t very effective at finding cancer at the earliest stage.
Therefore, “tumors that are allowed to grow and spread often develop multiple mutations, which make them less likely to respond to therapy,” said William L. Dahut, MD, chief scientific officer for the American Cancer Society (ACS).
Dahut emphasized that blood-based tests like that developed by Gatto could potentially detect cancer earlier than an imaging test, providing a “roadmap” to who needs imaging and allowing for a wide variety of cancers to be screened with a single test.
“The use of metabolism as a screening technique is novel that has definite potential, and the early results are promising,” he said.
He pointed out that additional studies should be done to show tests like this have a clinical impact beyond just detecting malignant cells.
Study Was ‘Proof of Concept’
Gatto said his research was a “proof of concept” study that only analyzed about one thousand patients, and we should wait for confirmation in much larger ones involving 10,000 or more.
“We did already confirm some findings within this study, which is encouraging but limited by the number of patients tested,” he said.
Gatto added that there appear to be some conditions, such as acute inflammation, that can also change GAGs. So, they need to monitor and confirm which subjects would be “most suitable for a test based on GAGs.”
A clinical trial is already underway and results are slated for 2025. Gatto is hopeful that this method could be used in pilot hospital settings sometime after that.
Cancer Incidence Rising
Advances in cancer screening technology are needed more than ever.
A recent review of cancer registry records from 44 countries finds that the incidence of early-onset cancers has increased for many types, some specifically affecting our digestive system. This increase is seen throughout middle and high-income countries.
The review authors believe some of the upswings in younger adults are partly happening because there are now highly sensitive tests for some cancers. These include breast, prostate, and thyroid.
However, testing doesn’t completely account for the increase.
They found that starting in the 1990s, worldwide trends including increased obesity, Type 2 diabetes, and a western-style diet high in saturated fats, red meat, processed meat, sugar, and ultra-processed foods might have a significant role.
“Cancer-related lifestyle factors in adulthood often originate from childhood and/or adolescence,” the review authors wrote.
They emphasized the importance of encouraging being active, eating a healthy diet, and avoiding alcohol and tobacco as important methods of primary cancer prevention.
Short evening sleep, longer midday napping may increase hypertension risk
Middle-aged and older adults who sleep less than 6 hours per day and take longer midday naps are more likely to develop hypertension and CVD, with slight variations for men vs. women, researchers reported.
“Siesta is a prevalent lifestyle in many countries, including China, and according to the data from [the] Chinese Center for Disease Control and Prevention, 39.3% of Chinese adults aged 15 to 69 years take siesta regularly and the rate of siesta was the highest among people aged 60 to 69 years,” Ling Lin, MM, of the department of emergency nursing at Fujian Medical University Union Hospital in Fuzhou, China, and colleagues wrote in the study background. “Too long [a] siesta may decrease the sleep duration at night and affect the total sleep duration of people, indicating that the percentage of siesta in the total sleep duration may be associated with the risk of hypertension or CVD. Whether the ratio of siesta duration in the total sleep duration was associated with the occurrence of hypertension or CVD was still unclear.”

Source: Adobe Stock
Longitudinal sleep data
Lin and colleagues analyzed data from 7,604 middle‐aged and older adults with sleep data and without hypertension or CVD at baseline, using the China Health and Retirement Longitudinal Study (CHARLS) database, a nationally representative longitudinal survey conducted in mainland China between June 2011 and March 2012. Median follow-up was 6.5 years; participants were followed for up to 3 years with questionnaires, with follow-up discontinued when an outcome event (hypertension or CVD) was observed. Researchers assessed associations of siesta and siesta ratio with incidence of hypertension and CVD.
The findings were published in Clinical Cardiology.
At the end of follow-up, 2,075 participants had hypertension and 986 participants had CVD.
Researchers found that, compared with a sleep duration of 6 to 8 hours, total sleep duration of less than 6 hours was associated with increased risk for hypertension, with an OR of 1.168 (95% CI, 1.023-1.335). A siesta ratio of at least 0.4 was similarly associated with hypertension risk, with an OR of 1.712 (95% CI, 1.129-2.594).
Sex-based differences in sleep time, CV risk
Among men aged 60 years and older, a siesta ratio of at least 0.4 was associated with higher risk for hypertension, whereas a total sleep duration of less than 6 hours was correlated with elevated risk for hypertension in men younger than 60 years.
Participants with a siesta duration of less than 30 minutes were more likely to develop CVD (OR = 2.053; 95% CI, 1.323-3.185). Among women aged 60 years and older, a sleep duration of less than 6 hours at night was associated with increased risk of CVD, whereas a siesta duration of less than 30 minutes and sleep duration of less than 6 hours at night was associated with CVD risk among women younger than 60 years.
“A longer daytime nap may lead to the elevation of evening cortisol levels and then increase the blood pressure levels,” the researchers wrote. “A high ratio of siesta suggested a long duration of siesta and a shorter duration of the sleep at night. The mechanisms of these might be because a longer duration of siesta may result in insomnia or low quality of sleep at night. Increasing studies indicated that a better night sleep is essential for the health of people.”
The researchers noted that the findings might provide a reference for midday napping and total sleep duration in people aged 45 years and older and said longer sleep at night vs. midday napping may be recommended.
The findings follow similar research published in July in Hypertension. As Healio previously reported, adults who reported taking frequent daily naps had greater risk for essential hypertension and stroke compared with those who never or rarely nap, likely due to poor sleep at night.
Low-dose tamoxifen confers sustained reduction in recurrence risk in noninvasive breast cancer
Use of low-dose tamoxifen conferred a sustained reduction in risk for recurrence among women with noninvasive breast cancer, according to updated results from the randomized, phase 3 TAM-01 trial.
The findings — presented at San Antonio Breast Cancer Symposium — also showed a low risk for death at 10-year follow-up.

“Four years ago, we presented 5-year data on low-dose tamoxifen, which showed a significant reduction in risk for recurrence,” Andrea DeCensi, MD, director of the medical oncology unit at National Hospital E.O. Ospedali Galliera — S.C. Oncologia Medica in Italy, said during a presentation.
After SABCS in 2018, ASCO and the U.S. Preventive Services Task Force guidelines included low-dose tamoxifen for preventive therapy in high-risk lesions. In addition, National Comprehensive Cancer Network recommended low-dose tamoxifen after ductal carcinoma in situ for symptomatic patients or those who were unwilling or unable to take full-dose tamoxifen, DeCensi said.
“Most importantly, [low-dose tamoxifen] became the most popular treatment [for] patients with high-risk lesions across several prominent U.S. centers, with lower discontinuation rates vs. 20 mg daily tamoxifen, raloxifene or aromatase inhibitors,” DeCensi said.
Background and methods
As Healio previously reported, the TAM-01 trial included 500 women (mean age, 54 years) undergoing treatment for DCIS, lobular carcinoma in situ (LCIS) or atypical ductal hyperplasia (ADH) across 14 centers in Italy.
Researchers assigned patients to either 5 mg daily tamoxifen (n = 253) or placebo (n = 247). Treatment continued for 3 years, with a minimum 2 years of additional follow-up. Incidence of invasive breast cancer or DCIS served as the primary endpoint.
Results of 5-year follow-up data presented at SABCS in 2018 showed a 52% decrease in cumulative risk for breast intraepithelial neoplasia recurrence with low-dose tamoxifen.
Researchers observed 14 primary events in the low-dose tamoxifen group vs. 28 events in the placebo group (HR = 0.48; 95% CI, 0.26-0.92). They also reported a significant decline in contralateral breast cancer cases in the low-dose tamoxifen group (12 vs. 3; HR = 0.24; 95% CI, 0.07-0.87). Results showed no significant differences in daily hot flashes, vaginal dryness/pain at intercourse, or musculoskeletal pain/arthralgia.
At SABCS, DeCensi presented updated data on breast cancer recurrence based on median follow-up of 9.7 years (range, 8.3-10.9).
Results
Researchers observed a 42% reduced risk for recurrence with low-dose tamoxifen.
Subgroup analyses showed reductions in ipsilateral breast events (16 vs. 23; HR = 0.68; 95% CI, 0.36-1.28) and contralateral breast events (6 vs. 16; HR = 0.36; 95% CI, 0.14-0.92) in the low-dose tamoxifen group.
“The effect on contralateral breast events reopens the door for prevention in high-risk unaffected women,” DeCensi said.
Researchers additionally reported a benefit with low-dose tamoxifen among post-menopausal women (HR = 0.43; 95% CI, 0.2-0.91), those with a BMI greater than 30 kg/m2 (HR = 0.26; 95% CI, 0.07-0.97), those who underwent mastectomy (HR = 0.2; 95% CI, 0.4-0.97) and those with DCIS (HR = 0.49; 95% CI, 0.27-0.89).
“In the DCIS cohort, we observed a remarkable 50% reduction in recurrence risk with 3-year low-dose tamoxifen, which — to us — provides a new standard of care for this cohort,” DeCensi said.
The safety of low-dose tamoxifen appeared consistent with previously reported findings, researchers noted.
Study limitations included the limited power for interactions and subgroup analysis, as well as the lack of vis-à-vis comparison with 20 mg daily tamoxifen. However, a noninferiority trial would be poorly accepted among patients with high-risk lesions due to toxicity of the 20-mg dose, DeCensi said.
“The lack of the 5 mg dose on the market is a reflection of zero commercial interest for this drug,” he added. “However, the 10-mg dose administered on alternate days is a reasonable alternative due to its long half-life.”
Implications
The findings are one more example of a missed optimal dose for a targeted agent, DeCensi said.
“Our aim is to attain a safe and equitable treatment that could cost $2 to $3 per month vs. the cost of other modern treatments, which is merciless and embarrassing,” he said. “My pledge to young investigators is to not miss the unique beauty of clinical academic research.”
Globally, only one in five meet WHO’s physical activity guidelines
Fewer than 20% of adults and adolescents around the world meet WHO’s physical activity guidelines, according to researchers.
The guidelines from 2020 recommend that children and adolescents complete 60 minutes of moderate-to-vigorous aerobic physical activity every day, and muscle-strengthening activities (MSA) 3 days per week. For adults and older adults, the guidelines call for 150 to 300 minutes of moderate physical activity or 75 to 150 minutes of vigorous intensity per week and MSA 2 days per week.

In a systematic review and meta-analysis, Antonio Garcia-Hermoso, PhD, head of the children and youth physical activity unit at Navarrabiomed, which is affiliated with the Public University of Navarra, and colleagues sought to estimate the proportion of the global population that was meeting WHO’s recommendations.
“Our study provides an accurate estimate of the prevalence of physical activity at the population level, which is an important modifiable chronic disease risk factor,” Garcia-Hermoso and colleagues wrote in the British Journal of Sports Medicine. “Adults engaging in aerobic and MSA at recommended levels showed important reductions in the risk of all-cause and cause-specific mortality in addition to a lower risk for multimorbidity (eg, cardiovascular risk and type 2 diabetes).”
The researchers searched five databases and identified 21 studies that included approximately 3.4 million people from 31 countries.
Overall, they found that the prevalence of adherence to the guidelines was 17.15% (95%, CI 15.44%-18.94%) among adults. The prevalence of adherence was slightly higher among teens, at 19.45% (95% CI, 16.34%-22.75%)
They additionally noted that adherence was lower among adults with low or medium education levels, those who were older, women, people who had underweight or obesity and those who self-rated their health as poor or moderate (P < 0.001), “although the prevalence remained very low in all cases.”
The researchers also analyzed prevalence by geographic location. Compared with those from Northern European countries like Iceland, Sweden, Denmark and the Netherlands, the United States and Southern and Central European countries like Malta, Cyprus, Croatia, Romania and Poland had lower prevalence of meeting guidelines.
Garcia-Hermoso and colleagues wrote that they were “unable to identify the key causes of the geographical differences” but offered a few possible explanations, like the different tools used to measure physical activity or “adoption of different exercise promotion policies between countries.”
“The Netherlands, one of the countries with higher prevalence, adopted the physical activity guidelines in 2017, and aimed for 75% of the Dutch population to adhere to them,” the researchers wrote. “The government launched several national policies or action plans for the promotion of physical activity for health through the collaboration between central government, the sports sector, municipalities, businesses, care providers and civil society organizations.”
Additionally, “wealth inequalities across countries, which likely impact an individual’s access to fitness facilities or the availability of free time to engage in aerobic and MSA, could also explain some of these differences.”
Garcia-Hermoso and colleagues concluded that “only one out of five adolescents and adults met the recommended combined aerobic and MSA guidelines,” and “large-scale public health interventions promoting both types of exercise are needed to reduce the associated burden of noncommunicable diseases.”
“These low prevalence levels are concerning from a public health perspective and emphasize the need to provide large-scale physical activity interventions that must be supported by long-term political commitment and paired with coordinated and sustained dissemination and communication strategies across sectors,” they wrote.