Month: June 2022
In Pics: This AI-piloted flying hotel never lands, offers memorable experience
Scent of a Friend: Similarities in Body Odor May Contribute to Social Bonding.
Intermittent Fasting May Help Heal Nerve Damage.
Nearly 30% of those with rheumatic disease saw employment change early in COVID-19 pandemic
Approximately 27% of patients with a rheumatic disease experienced a change in employment status during the early months of the COVID-19 pandemic, according to survey results published in The Lancet Rheumatology.
“People with rheumatic disease are at increased risk of infection due to immune dysregulation and the use of immunosuppressive medications,” Jonathan S. Hausmann, MD, of Beth Israel Deaconess Medical Center, in Boston, and colleagues wrote. “However, at the beginning of the COVID-19 pandemic, little was known to inform discussions about the risks of COVID-19 in people with these rheumatic diseases. As a result, people with rheumatic diseases faced substantial challenges in deciding how to modify their behavior to reduce their risk of infection with the SARS-CoV-2 virus.”

“These challenges also greatly affected employment and education, and consequently, access to health insurance and the ability to obtain health care,” they added. “Understanding the effect of the pandemic on people with rheumatic disease might help rheumatologists better address their patients’ needs and inform policies to protect this potentially vulnerable population.”
To examine how the COVID-19 pandemic has affected patients with rheumatic disease across the world, Hausmann and colleagues, in partnership with the American College of Rheumatology and its COVID-19 Global Rheumatology Alliance, created a survey. Developed through the help of key stakeholder groups, the COVID-19 Global Rheumatology Alliance Survey was administered to adults with inflammatory or autoimmune rheumatic diseases around the world through social media, websites and patient support organizations.

Jonathan S. Hausmann
Questions covered demographics, rheumatic diagnosis, COVID-19 diagnosis, adoption of protective behaviors against coronavirus infection, medication access and changes, health care access and communication with rheumatologists, and changes in employment or schooling status. A total of 12,117 participants responded to the survey between April 3, 2020, and May 8, 2020. Among these respondents, 10,407 included the appropriate age data. The researchers included data from participants with and without COVID-19, but excluded those who reported only noninflammatory rheumatic diseases.
In all, the researchers included complete responses from 9,300 respondents in their analysis, of whom 90.1% were women, 9.6% were men and 0.3% were nonbinary. In addition, 67.5% of the included participants reported they were white, while 16.8% identified as Latin American, 2.1% were Black, 2% were Asian and 0.5% were Native American, Aboriginal or First Nation. The most common rheumatic diagnoses were rheumatoid arthritis, with 39.1%; systematic lupus erythematosus, at 31%; and Sjögren’s syndrome, at 13.9%.
According to the researchers, 82% of the included respondents had continued their antirheumatic medications as prescribed, while 99.7% reported they had been following the suggested protective behaviors to prevent or limit COVID-19 spread. A total of 2,524 respondents, or 27.1%, reported a change in employment status. In all, the number of respondents who reported working full time decreased 13.6%, from 4,066 to 3,514.
“Understanding the early behaviors of people with inflammatory and autoimmune conditions is necessary to assess the effects of the pandemic on this population, and not only those who became infected with SARS-CoV-2,” Hausmann and colleagues wrote. “A far-reaching consequence of the pandemic at the time of data collection was the abrupt change to employment, and many people with rheumatic disease were faced with delayed or reduced income. Unique within the field of rheumatology, our study illustrates the direction and magnitude of employment change from Jan 1, 2020, to May 8, 2020.”
“Further work should address the consequences of employment status changes for health care access, medication affordability, mental health and rheumatic disease activity,” they added. “With an improved understanding of COVID-19 and the existence of patient recommendations from professional organizations, future studies should address changes in behaviors, perceptions and concerns in this population, including COVID-19 vaccination, COVID-19 sequelae and the long-term effect of the pandemic on patient outcomes.”
PERSPECTIVE
As the COVID-19 pandemic continues, research emerges on the effects of the physical and emotional health and financial impact of individuals worldwide. The pandemic has shaped the way people interact with one another and this includes the way people prioritize and receive health care services.
This study highlights the behaviors worldwide of patients with rheumatic diseases and how that has changed during the pandemic. The researchers illustrate the importance of the health professional in identifying barriers to care, such as the loss of insurance coverage due to job loss/changes, as well as having conversations about patient perceptions and attitudes toward their medication regimen. Asking questions pertaining to how the pandemic has affected their lives personally as well as professionally can encourage conversations that may identify areas for intervention to improve overall health.
The study also indicated that many patients adopted what is described as “protective behaviors,” such as social distancing and masking. These positive behaviors can be encouraged, and health care providers can provide patients with the necessary resources that give them the most current up-to-date information in a time where things are rapidly changing. We can also provide reassurance or changes if needed to treatment regimens in order to optimize adherence and preventing disease flares.
Patients who are immunosuppressed may also need help from their health care team in the way of documentation for schools and places of employment to ensure that they have accommodations in place to help keep them safe from infection. As the patients and families that we care for continue to adapt to how their lives have been changed during this pandemic, health care professionals are in a prime position to engage in shared decision-making with our patients as a way to support them and optimize their health.
Carolyn Zic, MSN, FNP-BC
Nurse practitioner, Pediatric rheumatology
University of Chicago
Comer Children’s Hospital
Board member, Rheumatology Nurses Society
Advisory board member, Mallinckrodt Pharmaceuticals
Radiofrequency ablation effective for most children with benign thyroid nodules
Most children who undergo image-guided radiofrequency ablation for treatment of benign nonfunctional thyroid nodules have at least a 50% reduction in nodule volume 4 years after treatment, according to study data published in Thyroid.
“Radiofrequency ablation was effective in reducing the volume of benign nonfunctional thyroid nodules in children, providing significant symptomatic relief with a good safety profile during short- and long-term follow-up,” Xinguang Qiu, MD, of the department of thyroid surgery at The First Affiliated Hospital of Zhengzhou University in China, and colleagues wrote. “Radiofrequency ablation should be considered as a beneficial, minimally invasive treatment modality for selected pediatric patients.”

Researchers reviewed data from 62 patients aged 18 years or younger with benign thyroid nodules treated with radiofrequency ablation at The First Affiliated Hospital of Zhengzhou University from July 2014 to August 2017 (75.8% girls; mean age, 14.4 years). Participants underwent an ultrasonography prior to the procedure to evaluate thyroid nodule composition and symptoms and had follow-up 3, 6 and 12 months after treatment. After 1 year, follow-up visits were performed annually. Ultrasonography and laboratory tests were repeated at each follow-up visit. Volume reduction ratio was calculated to assess the extent of nodule volume reduction.
Of the study cohort, 54 children had one thyroid nodule requiring treatment, and eight had two thyroid nodules. At 3 months, the mean volume reduction ratio was 65.1%, and increased to 74.7% at 6 months and to 77.5% at 1 year. The mean volume reduction ratio was 60.3% at 2 years, 68.5% at 3 years and 55.1% at 4 years. Thirty-six nodules had strong echogenicity or hyperechogenicity at 3 months, and six retained these characteristics at 6 months.
Sixteen of the 70 nodules began to regrow after initial treatment. Of the regrowing nodules, 56.3% had a volume reduction ratio below 50%, indicating a loss in treatment efficacy. Of those that lost treatment efficacy, 66.7% became larger than before treatment. Three nodules underwent a second radiofrequency ablation and surgery was performed on two other nodules.
Children requiring treatment of bilateral nodules had a lower volume reduction rate (13.6% vs. 74.1%; P < .001), lower technical efficacy (56.3% vs. 90.7%; P = .001) and higher regrowth rate (68.8% vs. 9.3%; P < .001) compared with unilateral nodules.
“We found that bilateral nodules requiring treatment had lower volume reduction rates, lower therapeutic efficacy and higher rates of regrowth, and the presence of bilateral nodules was an independent factor related to efficacy and regrowth,” the researchers wrote. “The specific reason for these associations is unclear. In addition, such results have not been reported in adult studies. Thus, radiofrequency ablation may not be appropriate for the treatment of bilateral thyroid nodules in children.”
Nodules with a higher cystic component had a higher volume reduction ratio than those with a lower cystic component (72.4% vs. 46.7%; P = .001). Nodules with higher vascularity had a lower regrowth rate than those with low vascularity (12.1% vs. 32.4%; P = .043). In all, 4.8% of patients had complications from the procedure.
The researchers wrote that radiofrequency ablation provides benefits for many patients, but those who undergo the procedure require long-term follow-up and the lack of a pathological exam means providers can not rule out malignancy.
“This treatment requires specialized treatment centers, specialized equipment, and highly skilled and experienced physicians, so access to radiofrequency ablation may also be a barrier to its use,” the researchers wrote. “Therefore, we believe that radiofrequency ablation is more likely to be a complementary treatment modality to surgical treatment.”
Artificial intelligence may be used to identify benign thyroid nodules
An ultrasound-based artificial intelligence classifier of thyroid nodules identified benign nodules with sensitivity similar to fine-needle aspiration, according to data presented at ENDO 2022.
“Artificial analysis of thyroid ultrasound images can identify nodules that are very unlikely to be malignant,” Nikita Pozdeyev, MD, PhD, assistant professor at University of Colorado Anschutz Medical Campus, told Healio. “These are mostly spongiform nodules that have a less than 3% probability of malignancy.”

Pozdeyev and colleagues trained a supervised deep learning classifier of thyroid nodules on 32,545 images of 621 thyroid nodules acquired from University of Washington. The classifier was then tested on an independent set of 145 nodules collected from the University of Colorado. The Big Transfer BiT-M ResNet-50×1 convolutional neural net architecture was modified to contain, 3, 4, 6 and 3 PreActBottleneck units per block 1 through 4. Weights pretrained on the ImageNet-21k dataset were loaded, and weights for blocks 3 and 4 fine-tuned for the binary classification task of distinguishing between benign and malignant thyroid nodules.
“We used an approach used to train clinically relevant classifiers called transfer learning,” Pozdeyev said in a press conference. “We took a model trained on natural images like cars, dogs and humans, and then that model is trained on an image set with tens of millions of images. Then we modified that model to work on a specific task — in our case, to take ultrasound images of thyroid nodules and make a call: cancerous or benign.”
When scaled by nodule size and using six random cine clip images per nodule, the classifier achieved an area under receiver operating characteristic curve of 0.872 on five-fold cross-validation. In the training data set of thyroid nodules, the classifier achieved a sensitivity of 94%, a specificity of 52% and a negative predictive value of 96% when determining benign vs. malignant nodules.
In the independent test set of thyroid nodules, the classifier achieved a sensitivity of 97% and a specificity of 61%. The negative predictive value was 98.5% and the positive predictive value was 40%.
“Computer-assisted diagnosis systems will be increasingly used by physicians of all specialties, including endocrinology,” Pozdeyev told Healio. “Our proof-of-concept study showed that an artificial intelligence-based thyroid nodule classifier can objectively select thyroid nodules that are unlikely to be malignant, do not require fine-needle aspiration biopsy, and can be managed with active surveillance. The validation of such a computer-assisted diagnosis system in a prospective clinical trial will be necessary before introduction into clinical practice.”
Frequently asked questions about COVID-19 vaccines for infants, toddlers
COVID-19 vaccines are now available for children as young as age 6 months in the United States.
The FDA has authorized and the CDC has recommended Moderna’s two-dose series at 25 g per dose for children aged 6 months through 5 years and Pfizer-BioNTech’s three-dose series at 3 g per dose for children aged 6 months to 4 years.
Below, Healio Pediatrics Editorial Board Member Leonard R. Krilov, MD, FAAP, FIDSA, FPIDS, chief of pediatric infectious diseases at NYU Langone Hospital – Long Island, answers some frequently asked questions about the vaccines.

Leonard R. Krilov
Healio: Is one vaccine preferred over the other?
Krilov: I think it’s a little too soon to answer that. I think there are pros and cons to each of the two.
Moderna has the advantage that it is only two doses and will be completed in a month. On the counter side, there did seem to be more adverse reactions in terms of fever and local pain, as well as fatigue and headache or irritability and sleep disturbances with this vaccine. Will that impact compliance with the second dose or how the vaccine will be perceived? Additionally, even though it is approved as a two-dose series with follow-up, there may well be an indication for a booster for this vaccine.
On the other side of the coin, the Pfizer vaccine at one-tenth of the adult dose seems to be associated with lower rates of local reactions and fever compared with placebo. However, the Pfizer vaccine requires three doses, and would take potentially up to almost 3 months to complete the series. The preliminary data suggested minimal, if any, protection after just the first two doses.
As in any clinical trial, you cannot put two experimental products head to head. The studies were conducted at different times with differing SARS-CoV-2 infection rates in the community and the data may not be totally comparable for the two vaccines. I think it is too soon to say where the favorability is going to be. Both vaccines are recommended equally. I’ll switch hats and put my parent hat on (although my children are grown) and suggest I would probably lean toward achieving protection sooner, but the most important thing is to get the children vaccinated.
Healio: As you mentioned, Pfizer’s vaccine is three doses. What are some ways a pediatrician can make sure a parent brings their child back for two follow-up vaccine appointments?
Krilov: Ensuring compliance with the vaccine series is important and needs to be emphasized to achieve the best level of protection. In a way, compliance is inversely proportional to number of doses or number of visits, so it is a concern that needs to be addressed.
I think we need to work with parents on demonstrating the significance of the infection, as well as the safety and benefits of the vaccine. The communication with the family should address the misconception that COVID-19 is a benign disease for young children and infants. Although we have not seen the mortality in young children from COVID-19 observed in the elderly and those with significant medical conditions, there have been more than 30,000 children aged younger than 5 years hospitalized with COVID-19 and more than 440 deaths in children aged younger than 4 years from this infection. More than one-half of these cases occurred in children with no pre-existing medical conditions.
The phrase I have used in these discussions is that although the infection is milder in children, it is not necessarily mild. It can still be a significant disease in terms of the acute illness and long COVID. Symptoms persisting for months have been described in children as well as in adults. Beyond this, discussing the safety and effectiveness of the vaccine in preventing severe disease should be included.
As we are trying to return to some degree of normalcy with no masks in school and increased in-person events, which is especially important for younger children’s speech development and socialization, I think vaccination is a critical part of our toolbox to help us get there safely. Telephone or text message reminders for second or third doses can be helpful in achieving compliance.
Healio: How can pediatricians counsel parents who may be hesitant about getting their young children vaccinated?
Krilov: I think there are two components to that discussion. One is certainly to emphasize that it is a safe and beneficial vaccine for their child. The other is that we need to spend some time addressing the misconception that this is a benign disease for the younger child, as described in the previous answer. In other words, we need to educate about what we’re vaccinating against. We have to be able to convincingly demonstrate that what we’re vaccinating against is worth preventing.
I think, in a way, for the other routine childhood vaccines, we are the victim of our own success. When people don’t see a lot of the vaccine-preventable diseases, they lose track of how significant they are, or were, and so therefore, can focus on potential concerns about reactions or the vaccines not being necessary. Maybe some of that’s true for COVID-19 as well, in the sense that the focus has been on older individuals and those with underlying medical issues. But I think it’s still significant for young children.
We want children to be able to do more and more and interact — that this is an important part of our toolbox help get there, maintain that. So, I think that is the track we need to take in order to be able to work with parents on showing the significance of the infection, as well as the safety and benefits of the vaccine.
Healio: Should parents start scheduling appointments now, or can the COVID-19 vaccine wait until they being their children in for a well visit or some other appointment?
Krilov: Because the vaccination is going to be administered over two or three visits, it might be hard to just totally dovetail into regular scheduled visits. And given, you know, the high levels of community spread in most areas of the country right now, I see no benefit to waiting. I understand it’s an extra visit, but I think the benefits are clear and the benefits should be achieved as soon as possible. It also should be noted that the COVID-19 vaccine can be given at the same time as other scheduled vaccines to avoid delays in getting vaccinated.
Healio : Do you think young children will eventually need a booster?
Krilov: Yes, I do think it is likely a booster for these children will be needed at some point, but it will require follow-up to determine if or when. Is this going to become like influenza, requiring periodic boosters for everyone? Are we going to settle into a more seasonal endemic pattern that will make timing of or need for boosters more predictable? Will there be additional waves this fall or winter, leading to recommendations for booster doses? Two and a half years ago we were talking about no hospital beds and having portable morgues in hospital parking lots, and now it’s a much more manageable disease. But again, there are still large numbers of cases.
I think the likelihood is this virus will continue to circulate, and with that, probably we will need periodic boosters. Is it going to be the same booster or, like influenza, is it going to be modified to match circulating variants? For example, omicron variant vaccines are in development now, so will the booster be with a different variant even to boost the immunity better? Will it turn out in a way down the road like influenza if we have multiple circulating variants to be a multivariant vaccine? It is still a bit premature to know the answer, but based on how immunity seems to wane for older children and adults, I do expect we will be looking at boosters for young children.
A New Statistical Method for Improved Brain Mapping
Summary: Researchers propose a new, more robust statistical method for mapping the brain.
Source: Paris Brain Institute
Brain mapping consists in finding the brain regions associated with different traits, such as diseases, cognitive functions, or behaviours, and is a major field of research in neuroscience. This approach is based on statistical models and is subject to numerous biases.
To try to counter them, researchers from the ARAMIS team, a joint team between the Paris Brain institute and Inria, and their collaborators at the University of Queensland (Australia) and Westlake University (China), propose a new statistical model for brain mapping.
The results are published in the Journal of Medical Imaging.
Mapping the brain
Mapping the brain is a challenge that mobilizes many neuroscience researchers around the world. The goal of this approach is to identify the brain regions associated with different traits, such as diseases, cognitive scores, or behaviors.
This type of study is also known as “Brain-wide association study” and rely on an exhaustive screening of brain regions to identify those associated with the trait of interest.
“The difficulty is that we are looking for a needle in a haystack, except that we don’t know how many needles there are, or in our case, how many brain regions there are to find,” explains Baptiste Couvy-Duchesne (Inria), first author of the study.
Meeting the challenges of signal redundancy
A first challenge lies in the number of brain measurements available per individual, which can quickly reach one million or more.
In addition, brain regions are correlated with each other. Some regions are highly connected and associated with many others, like nodes in a network.
Others, however, are more isolated, either because they are independent of other brain regions or because they contribute to very specific cognitive trait or brain function.
“If a brain region associated with our trait of interest is part of a highly connected network, the analysis will tend to detect the whole network, because the signal propagates within regions that are correlated with each other,” continues the researcher,
“This signal, which may seem very strong at first sight, is in fact redundant. How then can we find the region or regions that really contribute to the trait of interest within the network?”
To solve this problem, the researchers are proposing new statistical methods that are suited to the high dimensional image as well as for modelling the complex correlation structure within the brain.
Simulations to develop new statistical methods
In order to test the developed statistical methods, the researchers need very controlled data.
“We cannot compare methods directly on real traits or diseases, since we do not know what we are supposed to find,” explains Baptiste Couvy-Duchesne, “one method could find 10 regions associated with a trait, another 20, although we cannot tell which one is giving the correct answer.”
The key to this solving problem is to use simulations. Researchers use real brain images, but study fake diseases or fake scores, which they have constructed to be associated with dozens or hundreds of predefined brain regions.
This way, they are able to check whether the statistical methods detect the expected regions, but also whether they detect others (‘false positives’).
A more robust method and open questions
Once their method had been calibrated through these simulations (which revealed that the proposed approach was more accurate than the existing ones) the researchers used real traits as validation.

“Our new method finds fewer regions on average because it manages to remove some of the redundant associations. The next step is to apply it to study Alzheimer’s disease,” concludes the researcher.
A central result of the study it to demonstrate how pervasive are the redundant associations, using the current statistical methods. Thus, many associations identified to date may not be robust of directly pertinent for the trait studied.
In addition, several factors that are difficult to control can affect the quality of MRIs, such as head movements or the type of machines used, which can exacerbate the problem and lead to false associations.
Beyond the development of more refined analysis methods, the issue of data quality and homogeneity remains crucial.
About this brain mapping research news
Abstract
A parsimonious model for mass-univariate vertex-wise analysis
Purpose: Covariance between gray-matter measurements can reflect structural or functional brain networks though it has also been shown to be influenced by confounding factors (e.g., age, head size, and scanner), which could lead to lower mapping precision (increased size of associated clusters) and create distal false positives associations in mass-univariate vertexwise analyses.
Approach: We evaluated this concern by performing state-of-the-art mass-univariate analyses (general linear model, GLM) on traits simulated from real vertex-wise gray matter data (including cortical and subcortical thickness and surface area). We contrasted the results with those from linear mixed models (LMMs), which have been shown to overcome similar issues in omics association studies.
Results: We showed that when performed on a large sample (N = 8662, UK Biobank), GLMs yielded greatly inflated false positive rate (cluster false discovery rate >0.6). We showed that LMMs resulted in more parsimonious results: smaller clusters and reduced false positive rate but at a cost of increased computation. Next, we performed mass-univariate association analyses on five real UKB traits (age, sex, BMI, fluid intelligence, and smoking status) and LMM yielded fewer and more localized associations. We identified 19 significant clusters displaying small associations with age, sex, and BMI, which suggest a complex architecture of at least dozens of associated areas with those phenotypes.
Conclusions: The published literature could contain a large proportion of redundant (possibly confounded) associations that are largely prevented using LMMs. The parsimony of LMMs results from controlling for the joint effect of all vertices, which prevents local and distal redundant associations from reaching significance.
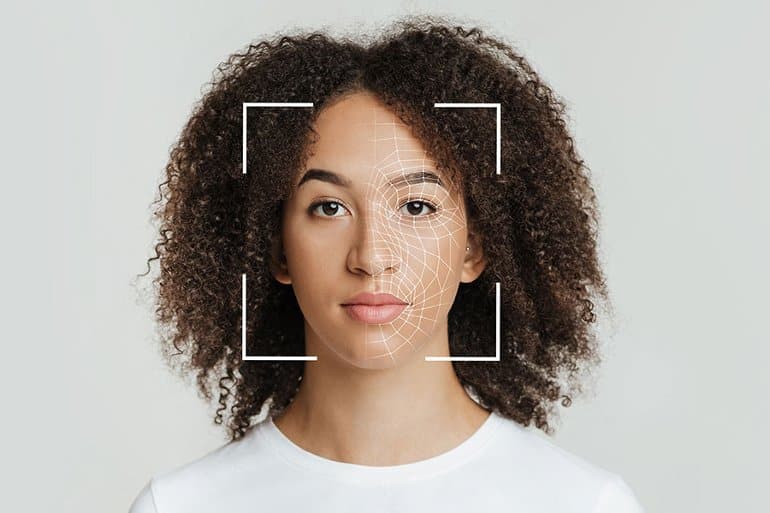
Artificial Neural Networks Model Facial Processing in Autism
Summary: Artificial intelligence helps shed new light on why many with autism have a difficult time when it comes to processing emotions via facial expressions.
Source: MIT
Many of us easily recognize emotions expressed in others’ faces. A smile may mean happiness, while a frown may indicate anger. Autistic people often have a more difficult time with this task. It’s unclear why.
But new research, published June 15 in The Journal of Neuroscience, sheds light on the inner workings of the brain to suggest an answer. And it does so using a tool that opens new pathways to modeling the computation in our heads: artificial intelligence.
Researchers have primarily suggested two brain areas where the differences might lie. A region on the side of the primate (including human) brain called the inferior temporal (IT) cortex contributes to facial recognition.
Meanwhile, a deeper region called the amygdala receives input from the IT cortex and other sources and helps process emotions.
Kohitij Kar, a research scientist in the lab of MIT Professor James DiCarlo, hoped to zero in on the answer. (DiCarlo, the Peter de Florez Professor in the Department of Brain and Cognitive Sciences, is a member of the McGovern Institute for Brain Research and director of MIT’s Quest for Intelligence.)
Kar began by looking at data provided by two other researchers: Shuo Wang at Washington University in St. Louis and Ralph Adolphs at Caltech. In one experiment, they showed images of faces to autistic adults and to neurotypical controls.
The images had been generated by software to vary on a spectrum from fearful to happy, and the participants judged, quickly, whether the faces depicted happiness. Compared with controls, autistic adults required higher levels of happiness in the faces to report them as happy.
Modeling the brain
Kar, who is also a member of the Center for Brains, Minds and Machines, trained an artificial neural network, a complex mathematical function inspired by the brain’s architecture, to perform the same task. The network contained layers of units that roughly resemble biological neurons that process visual information.
These layers process information as it passes from an input image to a final judgment indicating the probability that the face is happy. Kar found that the network’s behavior more closely matched the neurotypical controls than it did the autistic adults.
The network also served two more interesting functions. First, Kar could dissect it. He stripped off layers and retested its performance, measuring the difference between how well it matched controls and how well it matched autistic adults. This difference was greatest when the output was based on the last network layer.
Previous work has shown that this layer in some ways mimics the IT cortex, which sits near the end of the primate brain’s ventral visual processing pipeline. Kar’s results implicate the IT cortex in differentiating neurotypical controls from autistic adults.
The other function is that the network can be used to select images that might be more efficient in autism diagnoses. If the difference between how closely the network matches neurotypical controls versus autistic adults is greater when judging one set of images versus another set of images, the first set could be used in the clinic to detect autistic behavioral traits.
“These are promising results,” Kar says. Better models of the brain will come along, “but oftentimes in the clinic, we don’t need to wait for the absolute best product.”
Next, Kar evaluated the role of the amygdala. Again, he used data from Wang and colleagues. They had used electrodes to record the activity of neurons in the amygdala of people undergoing surgery for epilepsy as they performed the face task.
The team found that they could predict a person’s judgment based on these neurons’ activity. Kar reanalyzed the data, this time controlling for the ability of the IT-cortex-like network layer to predict whether a face truly was happy.
Now, the amygdala provided very little information of its own. Kar concludes that the IT cortex is the driving force behind the amygdala’s role in judging facial emotion.
Noisy networks
Finally, Kar trained separate neural networks to match the judgments of neurotypical controls and autistic adults. He looked at the strengths or “weights” of the connections between the final layers and the decision nodes. The weights in the network matching autistic adults, both the positive or “excitatory” and negative or “inhibitory” weights, were weaker than in the network matching neurotypical controls. This suggests that sensory neural connections in autistic adults might be noisy or inefficient.
To further test the noise hypothesis, which is popular in the field, Kar added various levels of fluctuation to the activity of the final layer in the network modeling autistic adults. Within a certain range, added noise greatly increased the similarity between its performance and that of the autistic adults.
Adding noise to the control network did much less to improve its similarity to the control participants. This further suggest that sensory perception in autistic people may be the result of a so-called “noisy” brain.
Computational power
Looking forward, Kar sees several uses for computational models of visual processing. They can be further prodded, providing hypotheses that researchers might test in animal models.
“I think facial emotion recognition is just the tip of the iceberg,” Kar says.
They can also be used to select or even generate diagnostic content. Artificial intelligence could be used to generate content like movies and educational materials that optimally engages autistic children and adults. One might even tweak facial and other relevant pixels in what autistic people see in augmented reality goggles, work that Kar plans to pursue in the future.
Ultimately, Kar says, the work helps to validate the usefulness of computational models, especially image-processing neural networks. They formalize hypotheses and make them testable. Does one model or another better match behavioral data?
