Summary: Researchers made a significant discovery in understanding the mechanisms behind protein accumulation in neurodegenerative diseases like Alzheimer’s. By studying fruit flies, the team found that a reduction in mitochondria within neuron axons leads directly to this detrimental protein buildup.
They pinpointed a rise in the protein eIF2β as a critical factor; reducing its levels restored protein recycling and improved neuron function. This breakthrough suggests a new target for therapies aimed at treating conditions like Alzheimer’s and ALS, potentially improving outcomes for patients.
Key Facts:
- The study revealed that depletion of mitochondria in neuron axons causes abnormal protein accumulation, a hallmark of diseases like Alzheimer’s.
- Researchers identified an increase in the protein eIF2β as a key contributor to this process; adjusting its levels could reverse the effects.
- The findings, derived from genetic studies in fruit flies, open the door to developing new treatments that could target mitochondrial health or regulate protein levels to combat neurodegenerative diseases.
Source: Tokyo Metropolitan University
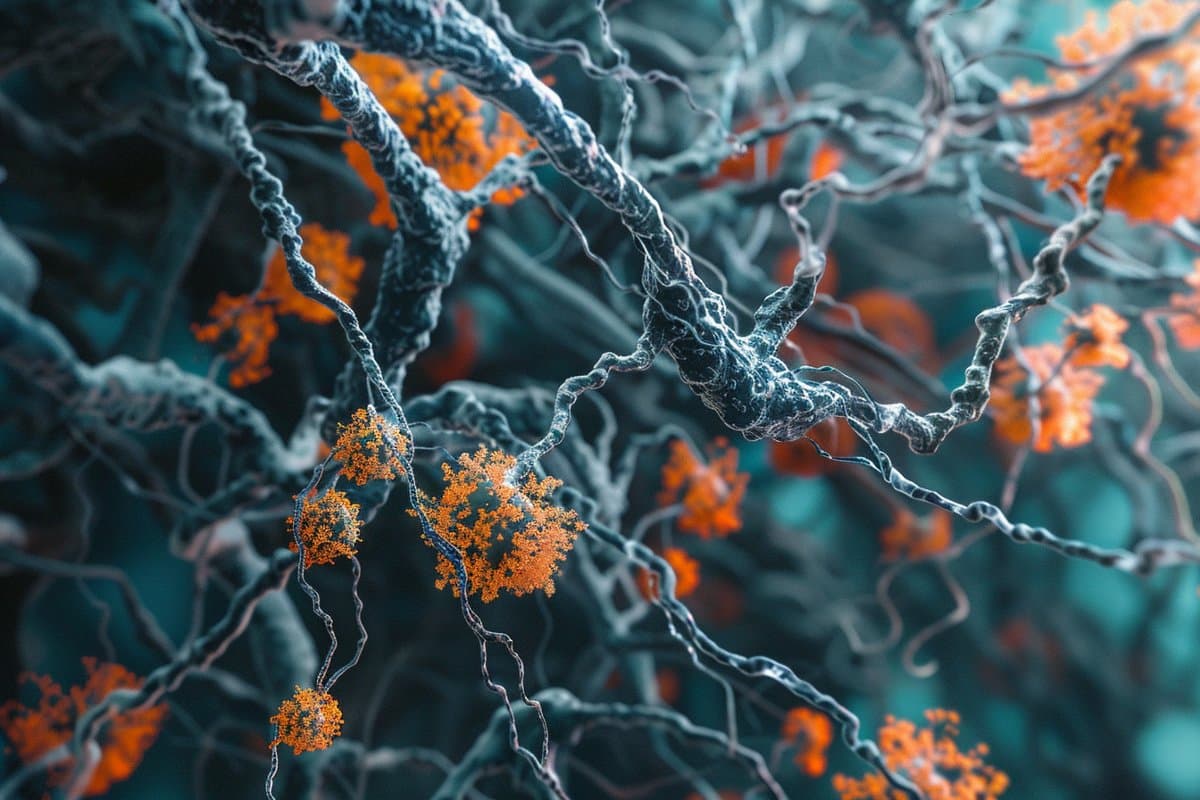
Researchers from Tokyo Metropolitan University have identified how proteins collect abnormally in neurons, a feature of neurodegenerative diseases like Alzheimer’s. They used fruit flies to show that depletion of mitochondria in axons can directly lead to protein accumulation.
At the same time, significantly high amounts of a protein called eIF2β were found. Restoring the levels to normal led to a recovery in protein recycling. Such findings promise new treatments for neurodegenerative diseases.
Every cell in our bodies is a busy factory, where proteins are constantly being produced and disassembled. Any changes or lapses in either the production or recycling phases can lead to serious illnesses. Neurodegenerative diseases such as Alzheimer’s and Amyotrophic Lateral Sclerosis (ALS), for example, are known to be accompanied by an abnormal build-up of proteins in neurons. However, the trigger behind this accumulation remains unknown.
A team led by Associate Professor Kanae Ando of Tokyo Metropolitan University have been trying to determine the causes of abnormal protein build-up by studying Drosophila fruit flies, a commonly studied model organism that has many key similarities with human physiology.
They focused on the presence of mitochondria in axons, the long tendril-like appendages that stretch out of neurons and form the necessary connections that allow signals to be transmitted inside our brains. It is known that the levels of mitochondria in axons can drop with age, and during the progress of neurodegenerative diseases.
Now, the team have discovered that the depletion of mitochondria in axons has a direct bearing on protein build-up. They used genetic modification to suppress the production of milton, a key protein in the transport of mitochondria along axons.
It was found that this led to abnormal levels of protein building up in fruit fly neurons, a result of the breakdown of autophagy, the recycling of proteins in cells. Through proteomic analysis, they were able to identify a significant upregulation in eIF2β, a key subunit of the eIF2 protein complex responsible for the initiation of protein production (or translation).
The eIF2α subunit was also found to be chemically modified. Both of these issues hamper the healthy action of eIF2.
Importantly, by artificially suppressing levels of eIF2β, the team discovered that they could restore the autophagy that was lost and regain some of the neuron function that was impaired due to axonal mitochondria loss. This not only shows that depletion of mitochondria in axons can cause abnormal protein accumulation, but that this happens via upregulation of eIF2β.
As populations age and the prevalence of neurodegenerative conditions continues to increase, the team’s findings present a vital step in developing therapies to combat these serious illnesses.
Abstract
Axonal distribution of mitochondria maintains neuronal autophagy during aging via eIF2β
Neuronal aging and neurodegenerative diseases are accompanied by proteostasis collapse, while cellular factors that trigger it are not identified.
Impaired mitochondrial transport in the axon is another feature of aging and neurodegenerative diseases. Using Drosophila, we found that genetic depletion of axonal mitochondria causes dysregulation of translation and protein degradation.
Axons with mitochondrial depletion showed abnormal protein accumulation, and autophagic defects. Lowering neuronal ATP levels by blocking glycolysis did not reduce autophagy, suggesting that autophagic defects are associated with mitochondrial distribution.
We found eIF2β was upregulated by depletion of axonal mitochondria via proteome analysis. Phosphorylation of eIF2α, another subunit of eIF2, was lowered, and global translation was suppressed.
Neuronal overexpression of eIF2β phenocopied the autophagic defects and neuronal dysfunctions, and lowering eIF2β expression rescued those perturbations caused by depletion of axonal mitochondria.
These results indicate the mitochondria-eIF2β axis maintains proteostasis in the axon, of which disruption may underly the onset and progression of age-related neurodegenerative diseases.
