My mother, who’s 89 years, thinks FaceTime involves a washcloth and some CoverGirl. So, she was understandably puzzled when I sat her in front of a computer for her first-ever telehealth visit.
“I don’t know if I’m going to like this. What’s this new doctor’s name?”
Fortunately, the physician was prompt, and he appeared on the screen smiling in a white lab coat with his name stitched above the breast pocket.
“Hello Connie. I’m Dr X. How are you feeling today?”
“Everything hurts.”
“I’m sorry to hear that, but I’m here to help…”
For the next hour, Dr X conducted a thorough and professional video exam. He was engaged and empathetic and summarized the key takeaways. So, I was surprised after the call ended when my mother said: “I don’t trust that guy.”
“Why not, Mom? He was great.”
“Did you notice the plant in his office?”
“Uh, yeah.”
“It was dying. Leaves turning brown. Do you want someone who can’t take care of a plant taking care of your mother?”
Now, I’m willing to bet that doctor had no idea his plant needed water, or that it was even in the room. But that one little detail kiboshed his entire effort to appear competent and win my mother’s trust.
It may seem unfair, but recent research suggests that your background during virtual visits is important. And it matters now more than ever: Telehealth has become a crucial part of modern healthcare provider services. Many patients now prefer telehealth, particularly for routine care, mental health care, minor illness, and chronic disease management. As always, projecting professionalism and building patient rapport are key. But in telehealth, like it or not, that also requires paying attention to what’s behind you.
“A background has measurable impact on patients’ telehealth experiences, which suggests a need for careful selection and design,” said Morgan Stosic, PhD, a social psychologist and researcher at the University of Maine.
Stosic authored a study, published in Telemedicine and e-Health in 2022, that found certain videoconferencing elements can help doctors convey more warmth (family photos) and competency (diplomas) and better connect with patients. Other elements, however, can distract patients (artwork, eg) and compromise the recall of clinical information.
Another study, conducted at Durham University in the United Kingdom and published in PLOS One in September, examined the impact of six different Zoom backgrounds on viewer perceptions of trust and competency. Backgrounds with books and (non-dying!) house plants engendered the most trust and competency, while backdrops with home-living spaces and novelty items encouraged the least.
“First impressions are formed instantly,” the Durham researchers wrote. “Within the first few seconds of meeting someone, we spontaneously draw inferences about their character traits.” Online, these inferences are influenced by the environment the person is in.
“Patients think they’re choosing the best doctor, but they really don’t have the tools and data to support that choice,” explained Ernesto Gutierrez, MD, a healthcare business coach in Spain whose online company (Practice Growth Formula) helps physicians present more effectively. “The only thing patients have is perceived expertise. So, a doctor needs to be thinking, ‘How do I engineer this perception with my telehealth patients?'”
To help you avoid the same fate as Dr X, Medscape Medical News spoke with practicing clinicians, telehealth trainers, researchers, and related experts. Here are their best tips for perfecting your webside manner.
1. Blurred, Virtual, or Real?
It’s tempting to take the easy way out and blur your background or choose a virtual one. But Erin Hulfish, MD, the director of telehealth education at the Renaissance School of Medicine at Stony Brook University, in NY, recommended against that.
“Those backgrounds can lead to a sense of mistrust,” she said. “Patients could think there’s somebody else in the room or wonder what is being hidden. They may worry about privacy and not speak honestly.”
She encourages her students to use real backgrounds that are clean and professional, “just like a patient would experience during a normal face-to-face appointment.” Avoid any messiness or disorganization. Having everything in its place subconsciously reassures patients that their care will be just as meticulous.
2. Books
Literacy is generally associated with intelligence and academic performance. So, having medical books on a shelf can make you appear smart and competent, as the Durham study found.
But there are times when books can interfere with that perception, namely when:
- There are so many it looks like you’re in a public library.
- You’re the author, and you give the impression of trying to make a sale.
- The titles are polarizing (Vladimir Putin: Life Coach), worrisome (This is Going to Hurt), or just plain weird (Knitting with Dog Hair).
3. Plants
Background greenery promoted feelings of competence and trustworthiness in the Durham study because of the “established human preference for natural environments,” said researchers. Flowers would probably have a similar effect, added Stosic, giving your professional space “a bit of life.”
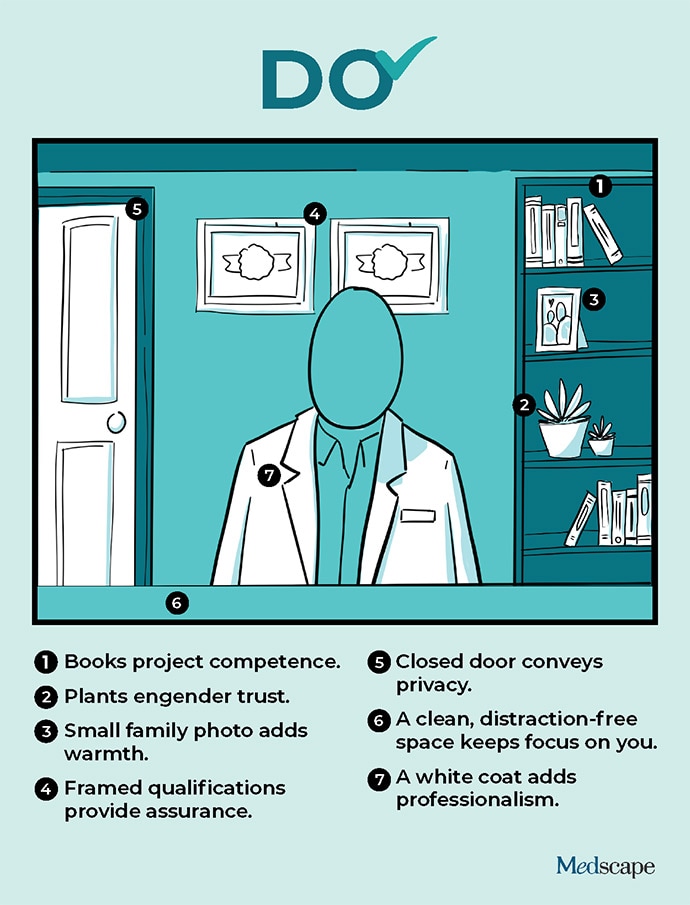
However, avoid lots of plants or a big bouquet. These can be distracting. A single healthy floor plant or orchid will do.
4. Artwork
In general, artwork of all types is distracting and should be avoided. This is especially true for the Banksy you bought at auction: Kids’ drawings and, of course, any portraits or busts of you. There are exceptions, though:
- In the Durham study, a small family photo engendered feelings of warmth toward doctors. It’s also another way to make a professional environment less antiseptic.
- Framed diplomas, certificates of recognition, hospital affiliations, and even awards (sans league bowling trophies) “provide patients with a sense of assurance,” said Hulfish. You’re educated, you’re professional, and you’re recognized for it.
5. Doors
If there’s a door in your background, close it. You wouldn’t leave the door of an exam room open when you’re with a patient, and the same logic applies here.
“Closed doors convey privacy,” said Hulfish, “and that’s important to virtual patients.” She recommended locking the door or hanging a “Virtual Exam in Progress” sign outside to prevent interruptions.
6. Desks
By its very nature, telehealth separates you from your patients. Positioning yourself closer to the camera and looking at the lens rather than the screen for better eye contact help broach this divide, but making a connection is still the medium’s biggest challenge.
So, Stosic recommends never putting anything additional between you and your patients, such as a desk. Either stand or, if you’re sitting at one, pull the computer closer so it’s not obvious.
7. Novelty Items
Ironically, Stosic’s study found that the more viewers liked a doctor’s background, the less likely they were to remember clinical information.
Again, you don’t want to distract them. A few strategically placed elements that convey warmth and competency are fine, but patients don’t need to see your signed Michael Jordan basketball or the rainbow trout you caught in Patagonia. Their focus should stay on you.
8. Mobile Phone
Keep it out of the picture, said Stosic. Even if it’s in silent mode, patients don’t know that. Plus, you may be tempted to glance at texts or notifications.
Similarly, avoid doing nonemergency telehealth calls from your car, an airport, or anyplace that isn’t professional and where patients can tell they don’t have your full attention.
9. Pets
Although some doctors use pets to connect with patients, the experts Medscape Medical News spoke with said the risks outweigh the rewards.
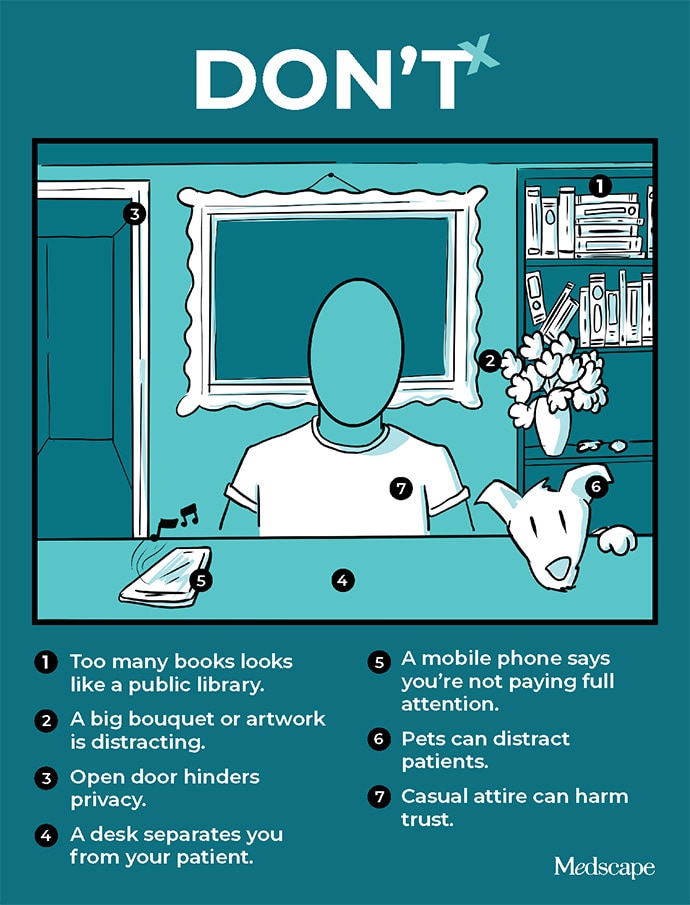
If the pet is in view, even if it’s dozing, the patient may pay less attention to you. Plus, there’s always the chance it’ll make noise and disrupt the call.
The only exception is using the pet to establish rapport with a new patient and then letting it out of the room before starting the visit.
10. Attire
What you’re wearing isn’t technically part of your background, but it is an important element of your presentation.
“A lot of doctors think it’s okay to conduct telehealth visits in a more casual and relaxed manner,” said Gutierrez. “But you have to look the part. If you don’t, you can spend the next hour being an amazing doctor, but [because first impressions are so important] your patients will have worse treatment adherence and less trust in you.”
Stosic’s research shows that patients are more comfortable when their doctors are in white lab coats. And although she hasn’t studied name tags specifically, she speculates they probably add to the sense of competency and professionalism. Plus, it helps new patients remember your name.
Other tips:
- Avoid decorating your lab coat or name tag with smileys, baubles, or other distractions.
- Simple earrings and rings are fine but save the fancy watches and other bling for the annual hospital gala. Not only is it distracting but it may rub some patients the wrong way.
- Make sure your white coat is clean.
- Forget the stethoscope around your neck; you won’t be using it.
Bonus Tip: Trust Your Gut
If all this seems like a lot, know that the idea is not to agonize over every background detail. It’s to be more thoughtful about the impression you aspire to create in the burgeoning field of telehealth.
This leads to Hulfish’s “most important” tip: Record yourself.
“That’s what we do with our med students,” Hulfish said. “Just as in any speaking course, we have them watch themselves on video. ‘How do I look? Is this the best camera angle, lighting, and background for me? What are my mannerisms?'”
“We are our own best critics.”