Engaging the brain’s plasticity by stimulating the locus coeruleus, a region in the brainstem, could be a clinically relevant approach to optimize the efficacy of cochlear implants in restoring hearing in the deaf, claims a study published in the journal Nature on December 21, 2022. The study “Locus coeruleus activity improves cochlear implant performance,” uses rat models fitted with multichannel cochlear implants to examine neuromodulation and plasticity in learning and performance following cochlear implantation.

Lead author of the study, Erin Glennon, PhD, a medical student at NYU Grossman School of Medicine said, “Our findings suggest that differences in neuroplasticity, particularly in parts of the brain such as the locus coeruleus, may help explain why some cochlear implant users improve faster than others.”
Co-senior author Robert Froemke, PhD, a professor of genetics at NYU Langone, said, “improving neuroplasticity in the locus coeruleus may speed up and bolster the effectiveness of cochlear implants.”
Cochlear implants are the first neuroprosthetic electronic devices to restore a human sense. Despite their success in enabling some recipients to understand speech within a few hours, it can take months or years before implantation results in an optimal perception of speech in others.
Experts believe that differences in neuroplasticity in the central auditory system may be responsible for this variable effectiveness. However, technical challenges in monitoring and manipulating neural activity in humans and animal models have left unanswered questions regarding neural mechanisms that control the brain’s ability to adapt to the implant.
Lina Reiss, PhD, associate professor of otolaryngology and biomedical engineering at Oregon Health & Science University said, “Clinically, this [study] might pave the way for novel treatments or even behavioral training strategies to better engage the locus coeruleus to speed up re-learning auditory processing through a cochlear implant. Stimulation of the locus coeruleus may also help poorly performing patients improve further even if they have plateaued.” (Reise studies pitch and speech perception in children and adults with cochlear implants and mechanisms of hearing loss after cochlear implantation. She was not involved in the current study.)
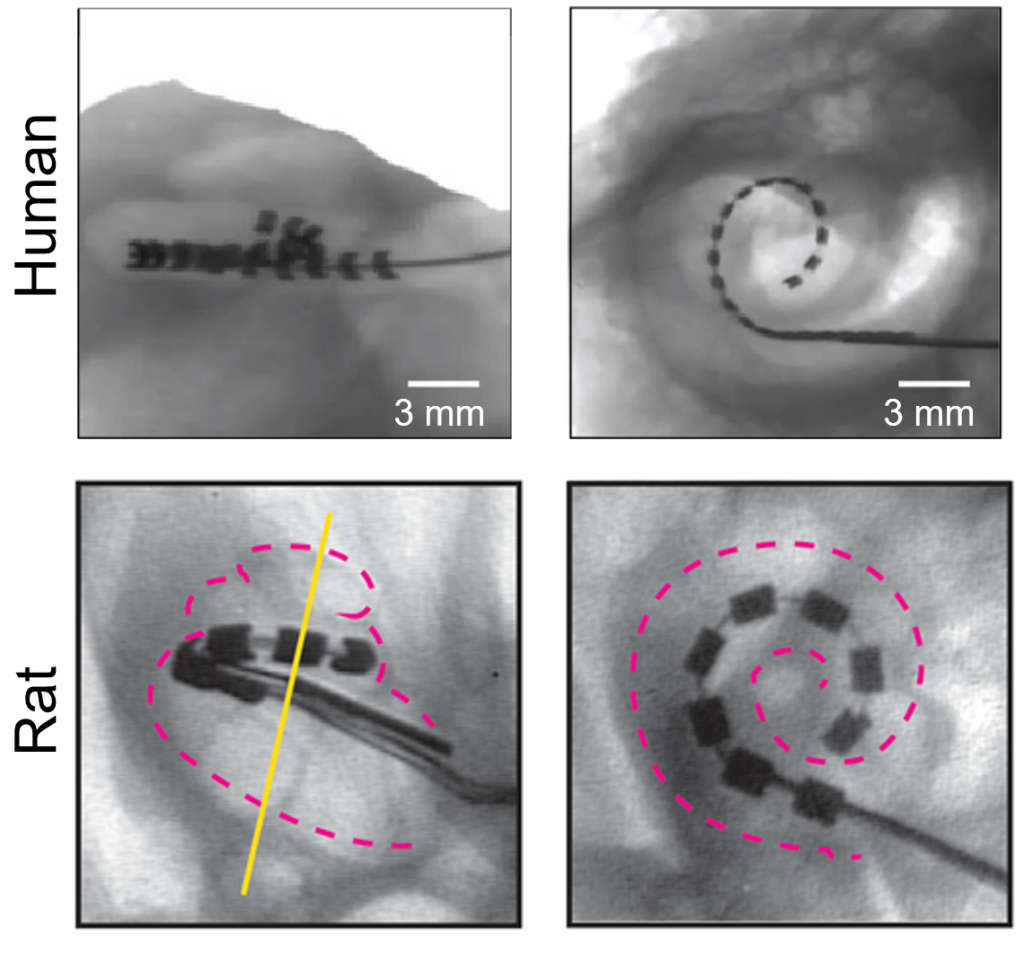
Cochlear implants consist of an externally worn microphone, sound processor and transmitter, and an implanted electrode system that receives signals from the external system and stimulates nerves in the inner ear.
Noradrenaline produced by the locus coeruleus is a key factor in inducing neuroplasticity. Earlier studies by the same group had shown electric stimulation of the locus coeruleus in normal rats increases neuroplasticity, accelerates learning new reward associations, and influences how the brain represents sound. The current study builds on their earlier work to demonstrate stimulation of the locus coeruleus hastens hearing in cochlear implant recipients. The investigators analyzed behavioral responses and neural activity in the locus coeruleus and the auditory cortex of deafened rats with multi-channel cochlear implants.
First, they trained normal rats on an auditory task that rewarded the animals on successful performance. The rats were trained to press a button when they heard a specific sound and to ignore the button if they heard a different tone. The rats showed substantial differences in learning rates and peak performance. Using photometry of the locus coeruleus, the researchers could predict when rats began responding to sounds and exhibited long-term accuracy in hearing.
As expected, deafened rats could not complete the task. The deafened rats were then given cochlear implants and retrained to perform the same task. Next, the researchers separated deafened rat models with the implanted neuroprosthetic into two sets, stimulating one group in the locus coeruleus with optogenetic stimulation while the other set of rats received no stimulation.
They found rats that were stimulated learned faster with higher long-term accuracy. In the reward-based auditory task, the stimulated rats showed enhanced performance and corresponding responses in the auditory cortex. Rats that received an optogenetic boost in the locus coeruleus could successfully complete the auditory task within three days while those that did not receive the boost took up to 16 days.
Activity in the locus coeruleus changed as the rats learned to use their implants. At initial stages, the locus coeruleus showed peak activity only when the animals received the reward, but later, activity peaked immediately following the tone. The speed of this change of activity in the locus coeruleus mirrored the animals’ ability to consistently succeed at the task.
“Previous studies have focused on the peripheral factors that govern variability—this study is innovative in finding a way to investigate central processing factors in an animal model, by focusing on the locus coeruleus,” said Reiss. “The findings have implications for our understanding of individual differences in how fast people can re-learn to hear through a cochlear implant, from the central auditory processing aspect.”
In future projects, the team intends to explore ways of stimulating the locus coeruleus in humans. “We need to determine what noninvasive mechanisms may be used to trigger the brain region,” said Mario Svirsky, PhD, professor of otolaryngology at NYU Langone and co-senior author of the study. Svirsky cautions that the current study tested hearing in rats using simple sounds in a straightforward task, while humans need to respond to nuanced speech patterns in noisy environments. Translating the insights from the current study to humans will require further research.

