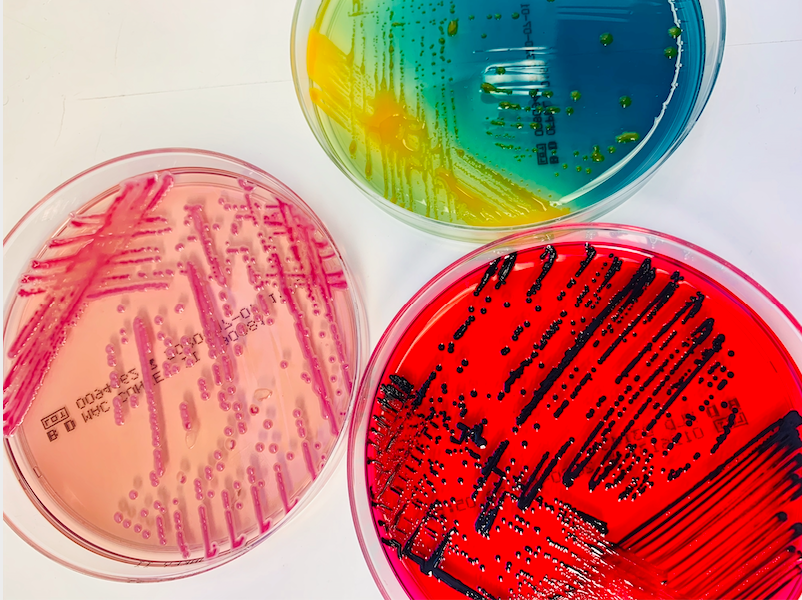
Growth of bacterial cultures in Petri dishes [Sylvia Suter, University Hospital Basel]
Clinical bacteriology relies on the ability to identify cultured isolates. However, unknown isolates are common in hospital settings. Now, researchers at the University of Basel, have established a new study algorithm—NOVA (Novel Organism Verification and Analysis)—to analyze bacterial isolates that cannot otherwise be characterized using conventional identification procedures.
This work is published in BMC Microbiology in the paper, “Novel Organism Verification and Analysis (NOVA) study: Identification of 35 clinical isolates representing potentially novel bacterial taxa using a pipeline based on whole genome sequencing.”
The team, which has been collecting and analyzing patient samples containing unknown bacterial isolates since 2014, have discovered more than thirty new species of bacteria, some of which are associated with clinically relevant infections.
In this work, the researchers led by Daniel Goldenberger, PhD, at the University of Basel, analyzed 61 unknown bacterial pathogens found in blood or tissue samples from patients with a wide range of medical conditions. Conventional laboratory methods, such as mass spectroscopy or sequencing a small part of the bacterial genome, had failed to produce results for all these isolates. Researchers sequenced the complete genome of the bacteria.
Out of 61 analyzed bacteria, 35 represent potentially novel species. And 27 of 35 strains were isolated from deep tissue specimens or blood cultures. The authors noted that, “Corynebacterium sp. (n = 6) and Schaalia sp. (n = 5) were the predominant genera. Two strains each were identified within the genera Anaerococcus, Clostridium, Desulfovibrio, and Peptoniphilus, and one new species was detected within Citrobacter, Dermabacter, Helcococcus, Lancefieldella, Neisseria, Ochrobactrum (Brucella), Paenibacillus, Pantoea, Porphyromonas, Pseudoclavibacter, Pseudomonas, Psychrobacter, Pusillimonas, Rothia, Sneathia, and Tessaracoccus.”
Most of the newly identified species belong to the Corynebacterium and Schaalia genera, both gram-positive bacilli. “Many species in these two genera are found in the natural human skin microbiome and the mucosa. This is why they are frequently underestimated, and research into them is sparse,” explained Goldenberger. They can, however, cause infections when they enter into the bloodstream—due to a tumor, for example.
The researchers classified the remaining 26 strains as hard to identify. An evaluation of the patient data showed that seven out of the 35 new strains were clinically relevant, meaning that they can cause bacterial infections in humans. “Such direct links between newly identified species of bacteria and their clinical relevance have rarely been published in the past,” said Goldenberger.
One of the hard-to-identify pathogens might be clinically relevant, too. It was found in the inflamed thumb of a patient after a dog bite. A Canadian research group also recently isolated this bacterium from wounds caused by dog or cat bites. “This has led us to assume that it is an emerging pathogen which we need to monitor,” said Goldenberger. The Canadian researchers appropriately named the bacterium Vandammella animalimorsus (animal bite Vandammella) in 2022.
Naming their new species is the next item on the Basel team’s to-do list, too. They are working closely with Peter Vandamme, a professor from the University of Ghent and a specialist in bacteria classification. Two of the bacteria have been named already. One is Pseudoclavibacter triregionum—referring to Basel’s location near the borders of Switzerland, France, and Germany.
