Day: 05/15/2022
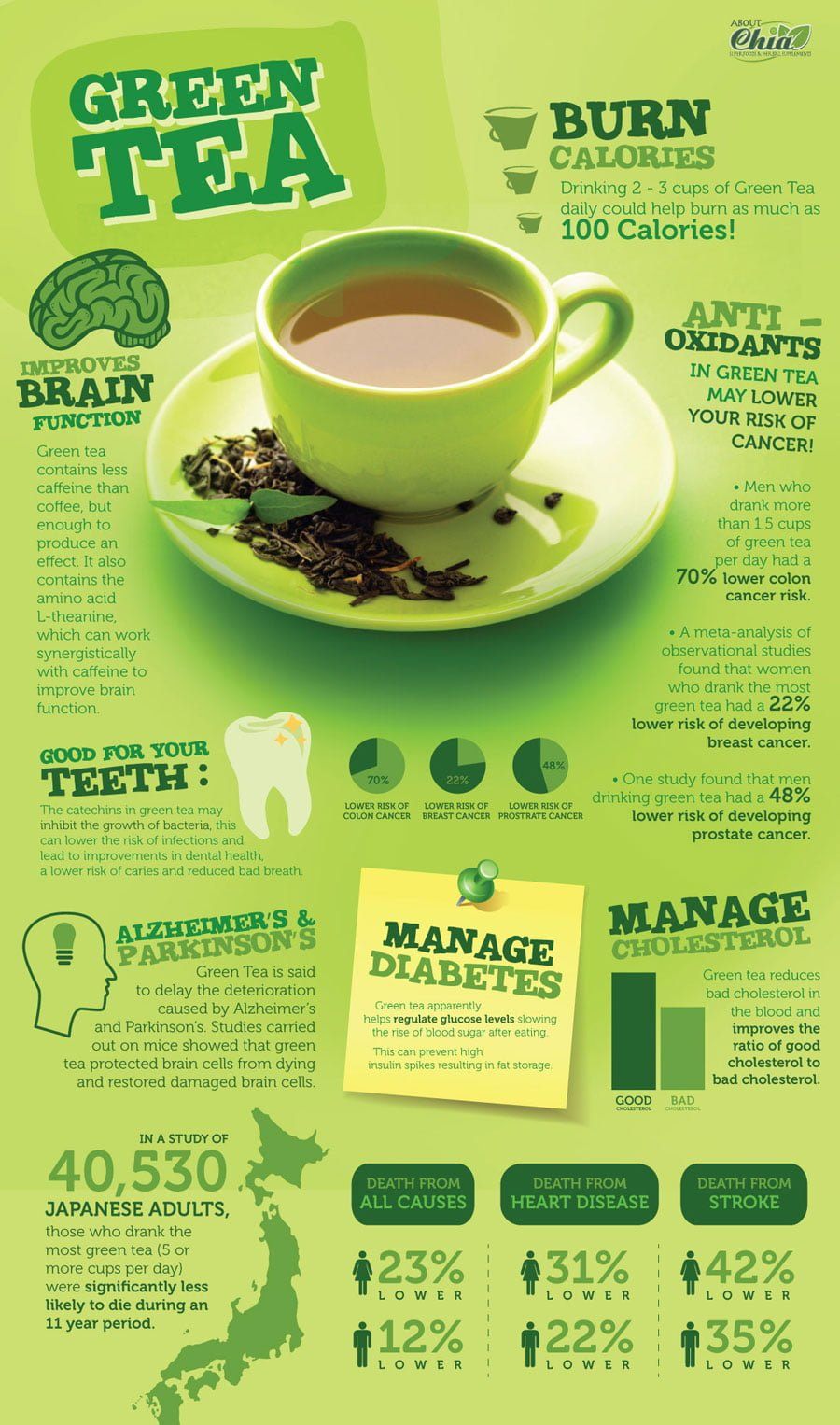
5 Proven Health Benefits of Green Tea
Green tea may help to improve weight loss efforts
Green tea reduces BMI and body weight
An analysis of randomized controlled studies found that people who drank green tea experienced a significant reduction in BMI and body weight. No significant improvement was however observed with regards to waist circumference and green tea consumption.1
This analysis consisted of 26 studies with a total of 1,344 participants, which revealed that body weight and BMI changed significantly after consumption of green tea of less than 800 mg/day for periods of 12 weeks or more.
Green tea extract improves gut health in mice
Green tea has been shown to reduce obesity and several inflammatory biomarkers associated with bad health in an animal study. Mice that consumed a diet supplemented with 2% green tea extract did much better compared to mice that consumed a diet without the green tea.2
The benefits seem to be as a result of improved gut health, such as more beneficial microbes in the mice’s intestines and less intestinal wall permeability, a condition known as “leaky gut” in humans.
This research provides proof that green tea promotes good gut bacteria growth, which subsequently results in a series of significant obesity risk reducing benefits.
Green tea compound EGCG slows weight gain in mice
In another study of obese mice, those that consumed a green tea compound known as EGCG together with a high-fat diet gained weight significantly slower compared to a control group that didn’t consume the green tea supplement.3
Two groups of mice were given a high-fat diet. The mice that consumed the EGCG compound together with the high-fat diet gained weight 45% slower compared to the control group consuming the identical diet without the EGCG compound. The results indicate that supplementing with green tea or EGCG will help gain weight slower.
As well as slower weight gain, the mice consuming the green tea compound exhibited an almost 30% increase in fecal lipids, which suggests that the absorption of fat was restricted by the EGCG. So not only does EGCG reduce the ability to absorb fat, but it also enhances the ability to use fat.
Appetite didn’t seem to be suppressed by the green tea, and both groups of mice could feed at any time and ate the same amount of high-fat food.
Greater gestational weight gain linked to higher BMI z score for girls, not boys
Girls whose mothers had high gestational weight gain have a greater BMI z score than girls whose mothers had normal gestational weight gain, but a similar difference is not observed for boys, according to study data.
“Girls appear to be more vulnerable than boys to the adverse effects of high pregnancy weight gain,” Beth Widen, PhD, RD, assistant professor in the department of nutritional sciences at the University of Texas at Austin, told Healio. “We observed that girls exposed to high prenatal weight gain have more adverse growth and adiposity patterns from mid-childhood and into early adolescence, compared to girls exposed to other weight prenatal change patterns.”

Widen and colleagues analyzed data from the Columbia Center for Children’s Environmental Health Mothers and Newborns Study, a prospective birth cohort in which Dominican and African American expectant mothers were enrolled during their third trimester of pregnancy at New York-Presbyterian Hospital and Harlem Hospital Center. Women aged 18 to 35 years with no self-reported diabetes, hypertension, HIV, drug use or smoking during pregnancy were included. Demographics were collected during a third trimester interview. Prenatal medical history, including prenatal weight measurements and gestational age at delivery, was obtained through medical records. Up to seven child height and weight measurements were recorded at age 5, 7, 9 and 11 years as well as during as many as three other project visits. Researchers used a latent class model to jointly fit prenatal weight patterns with sex-specific child body composition trajectories for body fat percentage, weight circumference and BMI z score.
The findings were published in Obesity.
There were 337 mother-child pairings included in the study. Of the mothers, 54% had a normal-weight BMI before pregnancy, 23.1% had overweight and 22.8% had obesity.
Researchers classified mothers into four gestational weight-change trajectories:
- “rapid, slow, moderate,” with high weight gain in the first trimester that slowed during the second and third trimesters;
- “loss, moderate, rapid,” with weight loss in the first trimester followed by higher weight gain in the second and third trimesters;
- “slow, moderate, moderate,” with slow weight gain in the first trimester before increasing to more than 1 lb per week in the second and third trimesters; and
- “always slow,” in which weight gain was moderate throughout pregnancy.
Researchers identified four child body composition trajectories from the joint model stratified by sex. There were differences in the divergence of growth patterns between boys and girls. The biggest difference was observed in offspring of mothers with a “rapid, slow, moderate” gestational weight gain, in which girls had higher estimates for BMI z score, waist circumference and body fat percentage than girls from mothers of other gestational weight gain patterns. Boys with mothers in the “rapid, slow, moderate” gestational weight gain trajectory had the second highest estimated BMI z score after age 10 years compared with the other trajectories, but waist circumference was lower than the other three groups. Girls of mothers in the “loss, moderate, rapid” group had lower trajectories for BMI z score, waist circumference and body fat percentage than the other groups, whereas boys from mothers in the “loss, moderate, rapid” group had similar composition compared with the other gestational weight trajectories.
Boys from mothers in the “slow, moderate, moderate” trajectory had a higher BMI z score and body fat percentage in early adolescence than those from mothers in other trajectories. Boys with mothers in the “always slow” gestational weight change trajectory had a lower BMI z score and body fat percentage than other groups but had the highest estimated waist circumference in early adolescence.
“The sex specific associations were really surprising and highlight the need to examine for sex-specific effects in epidemiologic and clinical research rather than only controlling for sex as a covariate,” Widen said.
In addition, Widen said more research is needed to assess the roles of diet and physical activity during pregnancy and whether patterns are associated with prenatal weight change and offspring body composition.
13 Things To Know About Paxlovid, the Latest COVID-19 Pill
Yale experts answer commonly asked questions about the oral antiviral medication.
[Originally published: March 10, 2022. Updated: May 12, 2022]
Note: Information in this article was accurate at the time of original publication. Because information about COVID-19 changes rapidly, we encourage you to visit the websites of the Centers for Disease Control & Prevention (CDC), World Health Organization (WHO), and your state and local government for the latest information.
Paxlovid is the latest COVID-19 treatment that’s been all over the news. The drug was granted an emergency use authorization (EUA) by the Food and Drug Administration (FDA) in December for anyone ages 12 and older who weighs at least 88 pounds, and is at high risk for severe disease. Pfizer recently began Phase 2 and 3 trials in children and teens ages 6 to 17.
Paxlovid is an oral antiviral pill that can be taken at home to help keep high-risk patients from getting so sick that they need to be hospitalized. So, if you test positive for the coronavirus and a health care provider writes you a prescription, you can take pills at home and lower your risk of going to the hospital.
The drug, developed by Pfizer, has a lot of positives: It had an 89% reduction in the risk of hospitalization and death in the clinical trial that supported the EUA, a number that was high enough to prompt the National Institutes of Health (NIH) to prioritize it over other COVID-19 treatments; it’s cheaper than many other COVID-19 drugs (it’s provided for free by the U.S. government while there is a public health emergency); and, perhaps most reassuring, it is expected to work against the Omicron variant.
“I think it is the beginning of a ‘game-changer,’” says Scott Roberts, MD, a Yale Medicine infectious diseases specialist. “It’s really our first efficacious oral antiviral pill for this virus. It shows clear benefit, and it really can prevent hospitalization and death in people who are at high risk.”
It’s important to note that Paxlovid (the brand name for the drug, which is made up of two generic medications—nirmatrelvir and ritonavir) isn’t the only pill available to treat COVID-19. The FDA also granted an EUA in December to a pill from Merck called molnupiravir (Lagevrio), but some studies suggest that molnupiravir has only a 30% reduction in the risk for hospitalization and death from COVID-19.
And as far as convenience, this medication is considered an improvement over treatments like remdesivir (approved by the FDA in October 2020), which is administered by intravenous (IV) injection.
We asked Yale Medicine infectious diseases experts common questions about Paxlovid. Below are their responses.
1. How does Paxlovid work?
Paxlovid is an antiviral therapy that consists of two separate medications packaged together. When you take your three-pill dose, two of those pills will be nirmatrelvir, the drug that inhibits the SARS-CoV-2 protein from replicating. The other is ritonavir, a drug that was once used to treat HIV/AIDS but is now used to boost levels of antiviral medicines.
As a COVID-19 treatment, ritonavir essentially shuts down nirmatrelvir’s metabolism in the liver, so that it doesn’t move out of your body as quickly, which means it can work longer—giving it a boost to help fight the infection.
2. When should I take Paxlovid?
You have to take Paxlovid within five days of developing symptoms.
Like all antivirals, Paxlovid works best early in the course of an illness—in this case, within the first five days of symptom onset, says Jeffrey Topal, MD, a Yale Medicine infectious diseases specialist who is involved in determining COVID-19 treatment protocols for Yale New Haven Hospital patients.
“Once you’ve been ill with the virus for more than a week, the damage done to the body in a severe case can’t be undone by the antiviral,” he says.
3. How often do I take Paxlovid?
You take three Paxlovid pills twice daily for five days for a full course that adds up to 30 pills. It helps that the pills are packaged in a “dose card,” basically a medication blister pack that allows you to punch out the pills as needed.
4. Is Paxlovid similar to Tamiflu?
“I think it’s a good comparison,” says Dr. Roberts. Tamiflu is an antiviral drug that reduces flu symptoms. Both are prescription-only oral antiviral pills given early in illness.
Tamiflu is taken twice a day for five days, and it must be started within 48 hours of flu onset. “When you give a patient Tamiflu beyond that, it doesn’t really change the course of their flu,” Dr. Roberts says.
But there are also differences between the two, starting with the way they were studied, Dr. Topal adds. Researchers showed that Paxlovid can prevent hospitalization and death. But since influenza causes fewer severe cases, clinical trials focused on whether Tamiflu could shorten the length of flu illness—which it did, he says.
5. Can anyone get a Paxlovid prescription?
The FDA authorized Paxlovid for people ages 12 and older who weigh at least 88 pounds. But in order to qualify for a prescription, you must also have had a positive COVID-19 test result and be at high risk for developing severe COVID-19.
That means you must either have certain underlying conditions (including cancer, diabetes, obesity, or others) or be 65 or older (more than 81% of COVID-19 deaths occur in in this group). The more underlying medical conditions a person has, the higher their risk for developing a severe case of COVID-19, according to the CDC.
The hope is that the restrictions on who can take Paxlovid will be relaxed over time. The FDA granted the EUA in December, just as a staggering number of people were infected with Omicron and the need for care skyrocketed, leading to supply issues.
6. How well does Paxlovid work?
When it applied for FDA authorization, Pfizer presented data from a clinical trial conducted between mid-July and early December in 2021. The data showed that participants (all of whom were unvaccinated) who were given Paxlovid were 89% less likely to develop severe illness and death compared to trial participants who received a placebo. (While the recommendation is to take Paxlovid within five days of symptom onset, participants in the clinical trial took the drug within three days.)
Scientists will continue to study the drug’s effectiveness as it is used to treat patients in the real world.
7. What do we know about how Paxlovid works in kids?
Pfizer launched a clinical trial in March to study the safety and efficacy of Paxlovid in children and teenagers ages 6 to 17 who have COVID-19 symptoms and test positive for the virus, and who are neither hospitalized nor at risk for severe disease.
While Paxlovid is authorized for use in adolescents and teenagers ages 12 and up, and weighing at least 88 pounds, that age group wasn’t tested in the original clinical trial. But because many children reach 88 pounds—considered to be an adult weight—the FDA has allowed extensions of EUAs for medications such as monoclonal antibodies and remdesivir in younger age groups, adds Dr. Topal.
“Based on the pharmacokinetics of the drugs in Paxlovid, the differences in metabolism and excretion—liver and kidney function specifically—of these drugs in this age group are thought to be similar to that of adults,” Dr. Topal says.
8. Does Paxlovid work against Omicron?
Paxlovid’s clinical trials took place before Omicron became predominant, but Pfizer says the drug works against the highly contagious variant. Three laboratory-based studies claim to back this up—two of those studies were conducted by Pfizer, while the third was done by Pfizer in partnership with the Icahn School of Medicine at Mount Sinai. These studies have not yet been published in peer-reviewed medical journals.
9. What are the side effects from Paxlovid?
Most people who take Paxlovid should not experience serious side effects, explains Dr. Roberts. “Paxlovid is usually very well-tolerated,” he says. Common side effects, which are usually mild, include:
- Altered or impaired sense of taste
- Diarrhea
- Increased blood pressure
- Muscle aches
Since Paxlovid is cleared by the kidneys, dose adjustments may be required for patients with mild-to-moderate kidney disease, explains Dr. Topal. “For patients with severe kidney disease—or who are on dialysis—or those with severe liver disease, Paxlovid is not recommended; the levels of the drug can become too high and could cause increased side effects,” he says.
It’s worth noting that Paxlovid is still being studied, so it is possible that all of the risks are not yet known. (The FDA has provided a fact sheet on Paxlovid with a full list of known side effects.)
10. Can I take Paxlovid if I’m taking other medications?
There is a long list of medications Paxlovid may interact with, and in some cases, doctors may not prescribe Paxlovid because these interactions may cause serious complications.
The list of drugs that Paxlovid interacts with includes some organ anti-rejection drugs that transplant patients take, as well as more common drugs like some used to treat heart arrhythmias. Paxlovid also decreases the metabolism of anticoagulants, or blood thinners, that many older adults depend on, driving up levels of those medications in the body to a point where they are unsafe, Dr. Topal explains.
It also interacts with cholesterol-lowering medications like Lipitor, but that’s less challenging for patients to overcome. “If you stop taking your Lipitor for five days, nothing bad is going to happen,” he adds.
If you are pregnant or breastfeeding, the FDA recommends discussing your options and specific situation with your health care provider, since there is no experience using the drug in these populations. If you could become pregnant, it’s recommended that you use effective barrier contraception or do not have sexual activity while taking Paxlovid.
11. What is the rebound effect of Paxlovid?
There have been reports of a “rebound” of COVID-19 symptoms in some people who have completed the five-day course of Paxlovid; in those cases, symptoms have recurred four or five days after completing the treatment. Some have also reported having a positive COVID-19 test after being treated with the drug. Pfizer had said that in the clinical trial for Paxlovid, several participants appeared to have a rebound in virus levels “around day 10 or day 14,” although this also occurred in some people who were given a placebo.
“This is being closely investigated and we should have more guidance soon,” says Dr. Roberts. “The hypothesis is that the immune system didn’t have a chance to see the full extent of the virus, since Paxlovid suppressed replication early in disease,” he says.
There is currently no evidence to support a second course of Paxlovid in these situations, but scientists are studying the effects of longer treatment durations, longer periods of isolation, and other ways of managing the problem, he adds.
For anyone who experiences a rebound, Pfizer recommends reporting it to them on its portal for adverse events associated with Paxlovid.
12. If I’m not eligible for Paxlovid, is there something else I can take?
There are other therapies for COVID-19, and anyone who cannot take Paxlovid—perhaps because it would interact with another medication—should talk to their doctor about the best approach for their situation.
13. Do I still need to be ‘up to date’ on vaccination if Paxlovid is available?
Vaccination remains a key part of prevention, even as more drugs become available, says Dr. Topal. He pictures prevention as an upside-down pyramid. Vaccination, mitigation efforts, such as masking, and testing would be at the base—and medications at the top point.
“Early testing is key to making these drugs work,” he says. “It’s always been the Achilles’ heel of these antiviral drugs that most people don’t get tested—or they don’t have access to testing.”
He encourages taking a test even if you think you only have a cold or allergies—and if you can get one. “Home testing is a huge part of the way to really ‘operationalize’ these medications,” he says, adding that while home tests may not be as highly sensitive as the laboratory-based polymerase chain reaction (PCR) tests, they are still very helpful in making a diagnosis.
Dr. Topal says people also should remember that Paxlovid, even with its high efficacy, is not perfect, and even if it were, viruses can mutate and develop resistance to antiviral medications. “Will some people still be hospitalized? Yes—no medication is perfect,” he says. “But for many high-risk patients, this medication can really reduce that risk.”
If you are experiencing symptoms of COVID-19 and think you are eligible for a treatment, you can visit the government Test-to-Treat Locater. You can use the site to search for the places near you where you can fill a COVID-19 prescription, or identify sites that provide testing, medical care, and COVID-19 medications.
Information provided in Yale Medicine articles is for general informational purposes only. No content in the articles should ever be used as a substitute for medical advice from your doctor or other qualified clinician. Always seek the individual advice of your health care provider with any questions you have regarding a medical condition.
SURMOUNT-1: Adults achieve weight loss of 16% or more at 72 weeks with tirzepatide
Adults with overweight or obesity taking the once-weekly GIP/GLP-1 receptor agonist tirzepatide achieved a mean weight loss of at least 16% at 72 weeks, according to topline results from the SURMOUNT-1 clinical trial.
In a phase 3 trial with 2,539 participants, tirzepatide (Eli Lilly) met both primary endpoints for mean percentage change in body weight from baseline and percentage of participants with a 5% reduction in body weight compared with placebo. Adults randomly assigned to receive tirzepatide had a mean weight loss of 16% with 5 mg, 21.4% with 10 mg, and 22.5% with 15 mg compared with a 2.4% mean weight loss for those assigned placebo. Of those assigned tirzepatide, 89% achieved a weight loss of at least 5% compared with 28% in the placebo group.

“This study shows that highly significant weight loss, in line with what is achieved with surgical procedures, can be achieved with tirzepatide,” Louis J. Aronne, MD, FACP, DABOM, the Sanford I. Weill Professor of Metabolic Research at Weill Cornell Medicine at New York-Presbyterian/Weill Cornell Medical Center and investigator in the SURMOUNT-1 trial, told Healio. “The mean BMI was about 38 kg/m2 to start and was reduced to about 30 kg/m2 with many subjects getting into the normal range.”
Tirzepatide met all key secondary endpoints, with 55% of those receiving 10 mg and 63% of those receiving 15 mg achieving a body weight reduction of at least 20% compared with 1.3% of the placebo group. In an additional secondary endpoint analysis not controlled for type 1 error, 32% of those receiving 5 mg tirzepatide lost at least 20% of body weight, according to the release.
“For perspective, a 5% weight loss reduces the risk of developing diabetes by 50%, and a 10% weight loss reduces it by 80%,” Aronne said. “Lap band produces about 17% weight loss, and sleeve gastrectomy 25% mean weight loss. The gap between diets and bariatric surgery is being filled by medical therapy.”
The safety and tolerability profile for tirzepatide was similar to that those of other incretin-based therapies approved for obesity treatment. Most side effects were mild to moderate; the most common were nausea, diarrhea, constipation and vomiting.
Participants with prediabetes at the start of the trial will remain enrolled for an additional 104 weeks beyond the initial 72-week trial period to evaluate the impact of body weight and potential differences in type 2 diabetes progression with tirzepatide compared with placebo.
The SURMOUNT-1 results will be presented at an upcoming medical meeting and submitted to a peer-reviewed journal, according to the release. Additional studies are ongoing.
PERSPECTIVE
This is extremely exciting, albeit preliminary data showing bariatric surgery-level weight loss from a medication, one that likely affords numerous other metabolic benefits, including diabetes improvement and prevention and possibly long-term cardiovascular benefit. Continued development of tirzepatide and similar agents could portend a sea change in obesity treatment, similar to how cholesterol and heart disease management was transformed by the advent of statin medications and how HIV management was transformed by antiretroviral medications.
Scott Kahan, MD, MPH
Endocrine Today Editorial Board Member
Director, National Center for Weight and Wellness
Faculty member, Johns Hopkins Bloomberg School of Public Health
New IDSA guidance covers drug interactions with Paxlovid
The Infectious Diseases Society of America issued guidance to help clinicians manage drug interactions between Paxlovid and the 100 most prescribed medications.
Additionally, the FDA said there is no evidence to suggest that a longer course of Paxlovid will benefit patients who experience a rebound in COVID-19 symptoms after completing a 5-day course of the medication.

Pfizer received an emergency use authorization for Paxlovid — which consists of the protease inhibitor nirmatrelvir and a low dose of ritonavir — in late December, making it the first available oral antiviral for COVID-19. It has been shown to reduce the risk for hospitalization and death from COVID-19 by close to 90%.
The Biden administration announced last month that it was purchasing 20 million courses of Paxlovid, which is a focus of its test-to-treat initiative. The medication is now available at many U.S. pharmacies after an initial supply shortage, said Jason Gallagher, PharmD, a clinical professor at Temple University School of Pharmacy in Philadelphia.

Jason Gallagher
“Availability has improved considerably in the past few months, and it is much easier to access than many people think,” Gallagher told Healio. “Perceptions are not in line with the reality of the current supply.”
Reported cases of relapse following a 5-day course of Paxlovid for COVID-19 are mostly anecdotal, Gallagher said, “but that doesn’t mean they are not real.”
“The relapse rate in the study that led to its approval was similar between the Paxlovid and placebo groups — about 2% — but that was in an unvaccinated population with different variants,” he explained.
In a recent update for providers, the FDA said it was aware of reports of patients developing COVID-19 symptoms after completing a course of Paxlovid, including some who tested negative for SARS-CoV-2 and then positive again, but that there is “no evidence of benefit at this time for a longer course of treatment” — for example, 10 days instead of 5.
The FDA reanalyzed clinical trial data and said the reports “do not change the conclusions from the Paxlovid clinical trial, which demonstrated a marked reduction in hospitalization and death.”
“The only duration of therapy for Paxlovid that we have evidence to support is the 5-day course that received the EUA,” Gallagher said. “EUAs are specific, and prescribers do not have a choice but to follow it. There is no specific guidance, but FDA has said that if someone does relapse on Paxlovid there is nothing preventing a second course from being prescribed.”
In the event a second course is prescribed, the IDSA says the duration of therapy should be used to guide adjustments to concomitant medications.
Paxlovid is authorized to treat mild-to-moderate COVID-19 in patients aged 12 years or older who are at high risk for progression to severe disease and weigh at least 40 kg. IDSA guidelines state that Paxlovid should be initiated within 5 days of symptom onset. Additionally, the guidance says patients with mild-to-moderate COVID-19 who are at high risk for progression to severe disease and who are admitted to the hospital for something other than COVID-19 can also receive Paxlovid.
“That covers a lot of people,” he said. “People with diabetes, people who are obese, elderly people, immunocompromised people.”
He said the potential for drug interactions with Paxlovid may have “scared away” many prescribers. However, among the top 100 most prescribed drugs, the IDSA said only two have interactions so severe that Paxlovid should be avoided altogether: rivaroxaban and salmeterol.
“A few combinations rule out Paxlovid use, but most can be managed during the 5 days of therapy. There are other drugs that cannot be combined with Paxlovid, so each patient needs individual assessment done,” Gallagher said.
According to the IDSA guidance, clinicians should obtain a complete list of a patient’s current medications including over-the-counter agents and herbal supplements — confirming that the patient is taking each medication as prescribed. They should review the FDA Paxlovid health care provider fact sheet to identify any medications contraindicated with Paxlovid, review potential drug interactions between Paxlovid and the patient’s current medications, and advise patients of any dose adjustments.
References:
IDSA. Management of drug interactions with nirmatrelvir/ritonavir (Paxlovid): Resource for Clinicians. https://www.idsociety.org/paxlovid. Accessed on May 9, 2022.
Steroids may reduce risk for death after severe COVID-19 hospitalization
Anti-inflammatory medications like steroids at hospital discharge may reduce post-acute infection mortality risk in patients who experienced hyperinflammation from severe COVID-19, according to data published in Frontiers in Medicine.
“Patients who have recovered from COVID-19 are at increased risk for hospitalization and death within 6-12 months after the initial episode,” Arch G. Mainous III, PhD, of the University of Florida, and colleagues wrote. “This morbidity and mortality is typically not listed or considered as a COVID-19 linked hospitalization or death in the medical records and thus are underreported as a post-acute COVID-19 sequelae. The reason for this phenomenon of severe outcomes as post-acute sequelae of COVID-19 is not well understood.

“Moreover, even 40-60 days post-acute COVID-19 infection there is evidence of a significant remaining inflammatory response in patients,” they added. “… Following from this hyperinflammation, the use of steroids as anti-inflammatory treatments among patients with high inflammation during the initial COVID-19 episode may do more than just help in the initial episode but may act as a buffer to the downstream morbidity and mortality from the initial COVID-19 episode.”
To examine the relationship between systemic inflammation in hospitalized adults with COVID-19 and post-recovery mortality, Mainous and colleagues analyzed a longitudinal cohort of patients within a large health care system. Patients included in the analysis were aged 18 years or older and tested for COVID-19 between Jan. 1, 2020, and Dec. 31, 2021, in the University of Florida Health System. Patients were only included if they were hospitalized for COVID-19.
Patients were considered to be hospitalized if they were admitted within 30 days of a positive COVID-19 test. Additionally, patients were only included in the final analysis if they retained at least 365 days of follow-up.
C-reactive protein (CRP) was the unit used to measure inflammation, and patients were only included if they underwent one CRP test “within their initial COVID-19 episode of care,” the researchers wrote. If multiple tests were performed, the highest value was used for the analysis. Mainous and colleagues also assessed intravenous dexamethasone administered during hospitalization, as well as prescriptions for oral dexamethasone that were prescribed at the hospital or post-discharge.
The primary outcome was 365-day all-cause mortality, derived from electronic health records and the Social Security Death Index. However, patients were censored at the date of their death and causes of death were not reliably reported, the researchers wrote.
According to the researchers, higher-than-normal CRP was associated with other markers of severe COVID-19, including the use of supplemental oxygen and intravenous dexamethasone.
In addition, increased CRP correlated with an increased mortality risk following recovery from acute COVID-19, with an unadjusted hazard ratio of 1.6 (95% CI, 1.18-2.17) and an adjusted hazard ratio of 1.61 (95% CI, 1.19-2.2). Meanwhile, oral steroid prescription at hospital discharge was associated with a lower risk for death (HR = 0.49; 95% CI, 0.73-0.94).
“Hyperinflammation present with severe COVID-19 is associated with an increased mortality risk after hospital discharge,” Mainous and colleagues wrote. “Although suggestive, treatment with anti-inflammatory medications like steroids upon hospital discharge is associated with a decreased post-acute COVID-19 mortality risk.
“This suggests that treating inflammation may also benefit other post-acute sequelae like long COVID,” they added. “A reconceptualization of COVID-19 as both an acute and chronic condition may be useful.”
New tool assessing symptoms of long COVID was developed with help from patients
Researchers in the United Kingdom developed a novel tool they said can assess the symptoms of long COVID and help deliver clinical care.
With input from patients, Sarah E. Hughes, PhD, MHSc, and colleagues created the Symptom Burden Questionnaire for Long COVID (SBQ-LC) to fill the need for a comprehensive, patient-reported outcome measure (PROM) that is specific to long COVID, Hughes said.

Sarah Hughes
“When reviewing existing measures, individuals living with long COVID told us that these PROMs did not fully capture their lived experience,” Hughes, a research fellow in the Centre for Patient-Reported Outcomes Research at the University of Birmingham, told Healio.
Hughes and colleagues used data collected from 13 adults with long COVID and published systematic reviews of long COVID symptoms to create the questionnaire, which was then field tested by 274 adults with long COVID.
The questionnaire is composed of 17 independent scales including symptoms involving breathing, circulation, fatigue, reproductive and sexual health, and pain. Using the questionnaire, users rate their symptom burden from the past 7 days using a dichotomous response or four-point rating scale.
According to the study, each of the 17 scales provides coverage of a different symptom domain and returns a summed score that can be transformed to a linear score numbering from 0 to 100, with higher scores representing a higher symptom burden.
“The SBQ-LC is a comprehensive patient-reported outcome measure of symptom burden, developed with extensive lived experience input and according to regulatory guidance. It is one of the first condition-specific PROMs available for long COVID research and clinical care,” Hughes said. “We hope it may be adopted widely for use as part of a core outcome set for long COVID to enable comparative global data.”
Hughes said the questionnaire is available for use by researchers and clinicians upon completion of a license agreement.
References:
Lung ultrasound a promising tool to monitor COVID-19 lung changes after discharge
Lung ultrasound findings significantly improved from hospitalization to 2 to 3 months after discharge in COVID-19 survivors, according to results of a study published in Respiratory Medicine.
“Several studies have … assessed the dynamic changes in lung ultrasound findings during a COVID-19 infection and found that lung ultrasound can be used to monitor disease progression during hospitalization,”Caroline Espersen, MD, researcher in the department of cardiology at Herlev and Gentofte Hospital at the University of Copenhagen in Denmark, and colleagues wrote. “However, whether the lung ultrasound findings detected during the initial COVID-19 infection resolve or persist after hospital discharge is less well investigated.”

The prospective, longitudinal study enrolled 71 adults with COVID-19 (mean age, 64 years; 61% men) in non-ICU hospital units. All patients underwent eight-zone lung ultrasound and blood sampling during hospitalization and again after discharge at 2 to 3 months’ follow-up. Follow-up lung ultrasound was performed a median of 72 days after the initial ultrasound, which was performed a median of 3 days after admission.
One-quarter of patients had acute respiratory distress syndrome, 46% had hypertension and 19% had diabetes.
Overall, 87% of patients had pathologic lung ultrasound findings in one or more zones at baseline compared with 30% during follow-up (P< .001). The proportion of patients with confluent B-lines in at least one zone also decreased from 25% at baseline to 0% at follow-up (P < .001). Researchers reported a decrease from hospitalization to follow-up in the total number of B-lines (median, 17 vs. 4; P < .001) and lung ultrasound score (4 vs. 0; P < .001).
On follow-up lung ultrasound, 28% of patients had three or more B-lines in at least one zone. However, among the 17 patients with ARDS during hospitalization, there was a higher number of B-lines (median, 5 vs. 3), and 47% had three or more B-lines in at least one zone compared with 22% of patients without ARDS.
“Although lung ultrasound is useful for monitoring changes in lung density after discharge in patients hospitalized for COVID-19, the long-term evolution in lung density as well as the association with pulmonary function and symptoms should be investigated further in future longitudinal follow-up studies,” the researchers wrote. “Lung ultrasound could potentially be implemented in a strategy to characterize the longer-term effects of COVID-19 infection on lung density.”
55% of patients have persistent symptoms 2 years after COVID-19 infection
More than half of patients who were hospitalized with COVID-19 reported at least one persistent symptom 2 years post-infection, regardless of initial disease severity, researchers reported.
The most frequently reported symptoms at 2 years were fatigue and muscle weakness.

“Several cohort studies have highlighted that the health effects of COVID-19 could persist up to 1 year after acute infection, most of which had no control groups of individuals who had not contracted COVID-19 and focused only on symptomatic sequelae or respiratory outcomes,”Lixue Huang, MD, from the department of pulmonary and critical care medicine at China-Japan Friendship Hospital at Capital Medical University and the National Center for Respiratory Medicine at the National Clinical Research Center for Respiratory Diseases, Beijing, and colleagues wrote in The Lancet Respiratory Medicine. “Hence, long-term and overall health outcomes of COVID-19 are largely unknown.”
Huang and colleagues reported 2-year follow-up data from an ambidirectional, longitudinal cohort study of 1,192 patients (median age, 57 years; 46% women) who survived COVID-19 and were discharged from Jin Yin-tan Hospital between January and May 2020. Participants completed three follow-up assessments during which the researchers measured health outcomes at 6 months, 12 months and 24 months after COVID-19 symptom onset using 6-minute walking distance, laboratory tests and questionnaires about symptoms, mental health, health-related quality of life, return to work and health care use after discharge. Also included in this study were participants without COVID-19 who were age-, sex- and comorbidities-matched to determine COVID-19 survivor recovery status at 2 years.
Median follow-up after COVID-19 symptom onset was 185 days for the 6-month visit, 349 days for the 12-month visit and 685 days for the 24-month visit.
The proportion of COVID-19 survivors with at least one reported symptom declined from 68% at 6 months to 55% at 2 years (P < .0001). Fatigue or muscle weakness was the most frequently reported symptom, present in 52% of patients at 6 months.
Compared with 26% of patients with a modified British Medical Research Council (mMRC) score of at least 1 at 6 months, 14% of patients had a score of at least 1 at 2 years (P < .0001).
Researchers reported improvement in health-related quality of life in nearly all domains, especially anxiety or depression. The proportion of patients with symptoms of anxiety or depression decreased from 23% at 6 months to 12% at 2 years (P < .0001). The researchers reported a continual decline in the proportion of patients with a 6-minute walking distance less than the lower limit of normal overall and in subgroups of different initial disease severity, with 89% of 494 COVID-19 survivors returning to their original work at 2 years.
Those with long COVID symptoms at 2 years reported more mobility problems (OR = 3.81; 95% CI, 1.62-8.93), more pain or discomfort (OR = 4.42; 95% CI, 3.14-6.21) and more anxiety or depression (OR = 7.46; 95% CI, 4.12-13.52) compared with survivors without long COVID. COVID-19 survivors also reported more problems with usual activity (2% vs. < 1%), more pain or discomfort (23% vs. 5%) and anxiety or depression (12% vs. 5%) at 2 years compared with controls.
Finally, researchers observed a higher proportion of COVID-19 survivors who received higher-level respiratory support during hospitalization with lung diffusion impairment (65% vs. 36%; P = .0009), reduced residual volume (62% vs. 20%; P < .0001) and total lung capacity (39% vs. 6%; P < .0001) compared with controls.
“The COVID-19 survivors had not returned to the same health status as the general population 2 years after acute infection, so ongoing follow-up is needed to characterize the protracted natural history of long COVID; we plan to conduct yearly follow-ups in this cohort,” the researchers wrote. “The value of rehabilitation programs in mitigating the effects of long COVID and in accelerating recovery requires further exploration.”