New research has uncovered a social world of viruses full of cheating, cooperation and other intrigues, suggesting that viruses make sense only as members of a community.

Introduction
Ever since viruses came to light in the late 1800s, scientists have set them apart from the rest of life. Viruses were far smaller than cells, and inside their protein shells they carried little more than genes. They could not grow, copy their own genes or do much of anything. Researchers assumed that each virus was a solitary particle drifting alone through the world, able to replicate only if it happened to bump into the right cell that could take it in.
This simplicity was what attracted many scientists to viruses in the first place, said Marco Vignuzzi, a virologist at the Singapore Agency for Science, Research and Technology Infectious Diseases Labs. “We were trying to be reductionist.”
That reductionism paid off. Studies on viruses were crucial to the birth of modern biology. Lacking the complexity of cells, they revealed fundamental rules about how genes work. But viral reductionism came at a cost, Vignuzzi said: By assuming viruses are simple, you blind yourself to the possibility that they might be complicated in ways you don’t know about yet.
For example, if you think of viruses as isolated packages of genes, it would be absurd to imagine them having a social life. But Vignuzzi and a new school of like-minded virologists don’t think it’s absurd at all. In recent decades, they have discovered some strange features of viruses that don’t make sense if viruses are lonely particles. They instead are uncovering a marvelously complex social world of viruses. These sociovirologists, as the researchers sometimes call themselves, believe that viruses make sense only as members of a community.
Granted, the social lives of viruses aren’t quite like those of other species. Viruses don’t post selfies to social media, volunteer at food banks or commit identity theft like humans do. They don’t fight with allies to dominate a troop like baboons; they don’t collect nectar to feed their queen like honeybees; they don’t even congeal into slimy mats for their common defense like some bacteria do. Nevertheless, sociovirologists believe that viruses do cheat, cooperate and interact in other ways with their fellow viruses.
The field of sociovirology is still young and small. The first conference dedicated to the social life of viruses took place in 2022, and the second will take place this June. A grand total of 50 people will be in attendance. Still, sociovirologists argue that the implications of their new field could be profound. Diseases like influenza don’t make sense if we think of viruses in isolation from one another. And if we can decipher the social life of viruses, we might be able to exploit it to fight back against the diseases some of them create.
Under Our Noses
Some of the most important evidence for the social life of viruses has been sitting in plain view for nearly a century. After the discovery of the influenza virus in the early 1930s, scientists figured out how to grow stocks of the virus by injecting it into a chicken egg and letting it multiply inside. The researchers could then use the new viruses to infect lab animals for research or inject them into new eggs to keep growing new viruses.
In the late 1940s, the Danish virologist Preben von Magnus was growing viruses when he noticed something odd. Many of the viruses produced in one egg could not replicate when he injected them into another. By the third cycle of transmission, only one in 10,000 viruses could still replicate. But in the cycles that followed, the defective viruses became rarer and the replicating ones bounced back. Von Magnus suspected that the viruses that couldn’t replicate had not finished developing, and so he called them “incomplete.”

In later years, virologists named the boom and bust of incomplete viruses “the von Magnus effect.” To them, it was important — but only as a problem to solve. Since no one had seen incomplete viruses outside of a lab culture, virologists figured they were artificial and came up with ways to get rid of them.
“You have to eliminate these from your lab stocks because you don’t want them to interfere with your experiments,” said Sam Díaz-Muñoz, a virologist at the University of California, Davis, recalling the common view within the field. “Because this is not ‘natural.’”
Researchers in the 1960s observed that incomplete viral genomes were shorter than those of typical viruses. That finding strengthened the view of many virologists that incomplete viruses were defective oddities, lacking the genes needed to replicate. But in the 2010s, inexpensive, powerful gene-sequencing technology made it clear that incomplete viruses were actually abundant inside our own bodies.
In one study, published in 2013, researchers at the University of Pittsburgh swabbed the noses and mouths of people sick with the flu. They pulled out the genetic material from influenza viruses in the samples and discovered that some of the viruses were missing genes. These stunted viruses came into existence when infected cells miscopied the genome of a functional virus, accidentally skipping stretches of genes.
Other studies confirmed this discovery. They also revealed other ways that incomplete viruses can form. Some kinds of viruses carry garbled genomes, for example. In these cases, an infected cell started copying a viral genome only to reverse partway through and then copy the genome backward to its starting point. Other incomplete viruses form when mutations disrupt the sequence of a gene so that it can no longer make a functional protein.

Introduction
These studies demolished the old assumption that von Magnus’ incomplete viruses were only an artifact of lab experiments. “They’re a natural part of virus biology,” Díaz-Muñoz said.
Discovering incomplete viruses in our own bodies has inspired a new surge of scientific interest in them. Influenza is not unique: Many viruses come in incomplete forms. They make up the majority of viruses found in people sick with infections such as respiratory syncytial virus (RSV) and measles.
Scientists have also come up with new names for von Magnus’ incomplete viruses. Some call them “defective interfering particles.” Others call them “nonstandard viral genomes.”
Díaz-Muñoz and colleagues have another name for them: cheaters.
A Viral Grift
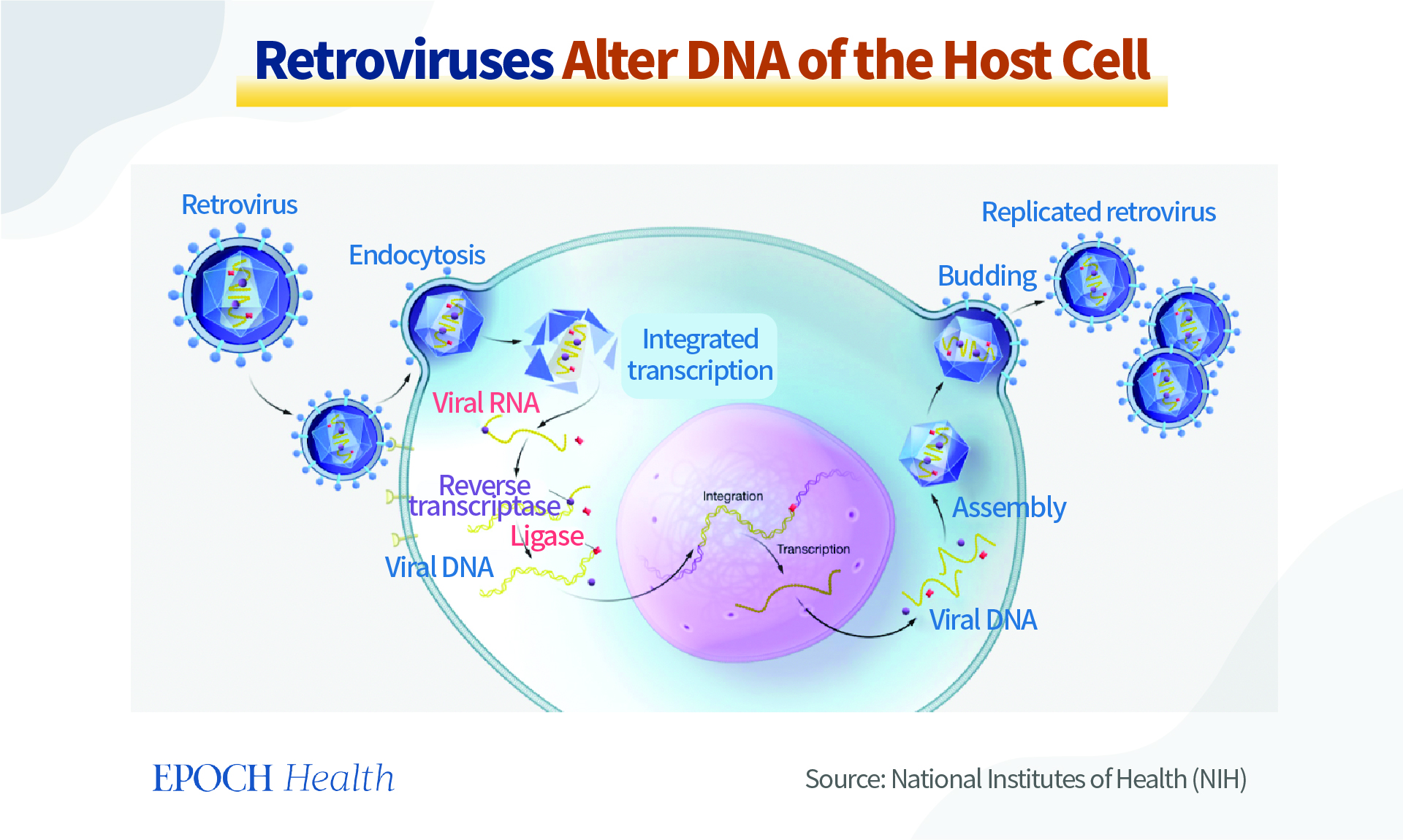
Incomplete viruses can typically get into cells, but once inside, they cannot replicate on their own. They lack some of the genes essential for hijacking their host’s protein-making machinery, such as the one for a gene-copying enzyme known as a polymerase. In order to replicate, they have to cheat. They have to take advantage of their fellow virus.
Fortunately for the cheaters, cells are often infected by more than one viral genome. If a functional virus shows up in a cheater’s cell, it will make polymerases. The cheater can then borrow the other virus’s polymerases to copy its own genes.
In such a cell, the two viruses race to make the most copies of their own genome. The cheater has a profound advantage: It has less genetic material to replicate. The polymerase therefore copies an incomplete genome more quickly than a complete one.
Their edge grows even larger over the course of an infection, as incomplete viruses and functional ones move from cell to cell. “If you’re half as long, that doesn’t mean you get a two-times advantage,” said Asher Leeks, who studies social evolution in viruses as a postdoc at Yale University. “That can mean you get a thousand-times advantage or more.”
Other cheater viruses have working polymerases, but they lack the genes for making protein shells to enclose their genetic material. They replicate by lying in wait for a functional virus to show up; then they sneak their genome into the shells it produces. Some studies suggest that cheater genomes may be able to get inside shells faster than functional ones.

Introduction
Whichever strategy an incomplete virus uses to replicate, the result is the same. These viruses don’t pay the cost of cooperation, even as they exploit the cooperation of other viruses.
“A cheater does poorly on its own, it does better in relation to another virus, and if there are a lot of cheaters, there’s no one to exploit,” Díaz-Muñoz said. “From an evolutionary perspective, that’s all you need to define cheating.”
The last part of that definition poses a puzzle. If cheaters are so amazingly successful — and, indeed, they are — they ought to drive viruses to extinction. As generations of viruses burst out of old cells and infect new ones, cheaters ought to get more and more common. They should keep replicating until the functional viruses disappear. Without any functional viruses left, the cheaters can’t replicate on their own. The entire population of viruses should get sucked into oblivion.
Of course, viruses such as influenza are clearly escaping this swift extinction, and so there must be more to their social lives than a death spiral of cheating. Carolina López, a virologist at Washington University School of Medicine in St. Louis, believes that some viruses that look like they’re cheating may actually play a more benign role in viral societies. Instead of exploiting their fellow viruses, they cooperate, helping them thrive.
“We think of them as part of a community,” López said, “with everybody playing a critical role.”
Burnout Prevention
López’s initiation into the world of sociovirology started in the early 2000s as she studied Sendai virus, a pathogen that infects mice. Researchers had known for years that two strains of Sendai virus behaved differently. One, called SeV-52, was good at escaping the notice of the immune system, allowing the virus to cause a massive infection. But mice infected with another strain, SeV-Cantell, mounted a swift, powerful defense that helped them quickly recover. The difference, López and her colleagues found, was that SeV-Cantell produced a lot of incomplete viruses.
How were incomplete viruses triggering the mice’s immune systems? After a series of experiments, López and her colleagues established that incomplete viruses cause their host cells to activate an alarm system. The cells produce a signal called interferon, which lets neighboring cells know an invader has arrived. Those cells can prepare defenses against the viruses and prevent the infection from spreading like wildfire through the surrounding tissue.

This phenomenon wasn’t a quirk of Sendai virus, nor of the mouse immune system. When López and her colleagues turned their attention to RSV), which sickens over 2 million people in the United States every year and causes thousands of deaths, they found that incomplete viruses produced in natural infections also triggered a strong immune response from infected cells.
This effect puzzled López. If incomplete viruses were cheaters, it didn’t make sense for them to provoke a host to cut an infection short. Once the immune system destroyed the functional viruses, the cheaters would be left without any victims to exploit.
Lopez found that her results made sense if she looked at the viruses in a new way. Instead of focusing on the idea that the incomplete viruses were cheating, López began to think about them and the functional viruses as working together toward the shared goal of long-term survival. She realized that if functional viruses replicated uncontrollably, they might overwhelm and kill their current host before transmission to a new host could take place. That would be self-defeating.
“You need some level of immune response for just keeping your host alive long enough for you to move on,” López said.
That’s where the incomplete viruses come in, she said. They might rein in the infection so that their host has a chance to pass viruses onto the next host. In that way, the functional and incomplete viruses might be cooperating. The functional viruses produce the molecular machinery to make new viruses. Meanwhile, the incomplete viruses slow the functional viruses down to avoid burning out their host, which would end the entire community’s infectious run.
In recent years, López and her colleagues have found that incomplete viruses can curb infections in a number of ways. They can trigger cells to respond as if they were under stress from heat or cold, for example. Part of a cell’s stress response shuts down the protein-building factories to save energy. In the process, it also halts the production of more viruses.

Introduction
Christopher Brooke, a virologist at the University of Illinois Urbana-Champaign, agrees with López that viruses exist in communities. What’s more, he suspects that incomplete viruses have other jobs in cells that he and his fellow scientists have yet to figure out.
Brooke is looking for evidence of these jobs in influenza viruses. A complete influenza virus has eight gene segments, which typically make 12 or more proteins. But when infected cells produce incomplete viruses, they sometimes skip the middle of a gene and stitch the beginning to the end. Despite this drastic change, these altered genes still produce proteins — but new proteins that may have new functions. In a study published in February, Brooke and his colleagues discovered hundreds of these new proteins in flu-infected cells. Because these proteins are new to science, the researchers are trying to figure out what they do. Experiments on one of them suggest that it latches on to polymerase proteins made by intact viruses and blocks them from copying new viral genomes.
For now, however, scientists are largely ignorant of what incomplete viruses accomplish by producing so many strange proteins. “My limited imagination isn’t going to touch a fraction of what’s possible,” Brooke said. “This is raw material for the virus to play with.” But he doubts that the incomplete viruses producing all these strange proteins are cheaters.
“If they really were acting as pure cheaters, I would predict that there would be substantial selective pressure to minimize their production,” Brooke said. “And yet we see them all the time.”
Blurred Lines
Sociovirologists are now trying to figure out just how much cheating and cooperation are going on in the viral world. Scientists who study animal behavior know how hard this can be. An individual may cheat in some situations and cooperate in others. And it’s also possible for a behavior that looks like cooperation to evolve through selfish cheating.
Leeks agrees that incomplete viruses may be productive parts of the viral community. But he thinks it’s always important to consider the possibility that even when they look like they’re cooperating, they are still actually cheating. Evolutionary theory predicts that cheating will often arise in viruses, thanks to their tiny genomes. “In viruses, conflict is dominant,” Leeks said.

Introduction
In fact, cheating can produce adaptations that look like cooperation. One of Leeks’ favorite examples of this hidden conflict is the nanovirus, which infects plants such as parsley and fava beans. Nanoviruses replicate in an astonishing way. They have eight genes in total, but each viral particle has just one of the eight genes. Only when all nanovirus particles, each carrying one of the eight different genes, are infecting the same plant at once can they replicate. The plant cells make proteins from all eight genes, along with new copies of their genes, which then get packaged into new shells.
You might look at nanoviruses and see a textbook case of cooperation. After all, the viruses have to work together for any of them to have a chance to replicate. The arrangement is reminiscent of a beehive’s division of labor, in which the insects split the work of gathering nectar, tending to larvae and scouting new locations for the hive to move to.
But Leeks and his colleagues have charted how nanoviruses — and other so-called multipartite viruses — may have evolved through cheating.
Underneath the façade of cooperation lies viral cheating.
Imagine that the ancestor of nanoviruses started off with all eight genes packaged in one viral genome. The virus then accidentally produced incomplete cheaters that had only one of the genes. That cheater will thrive, as the fully functional viruses copy its gene. And if a second cheat evolves, carrying a different gene, it will get the same benefit of exploiting the intact viruses.
When Leeks and his colleagues built a mathematical model for this evolutionary scenario, they found that viruses can readily break apart into more cheats. They will keep breaking apart until none of the original viruses that could replicate on their own are left. Nanoviruses may now depend on each other for survival, but only because their ancestors freeloaded off each other. Underneath the façade of cooperation lies viral cheating.
Sorting out the nature of virus societies will take years of research. But solving the mystery may bring a tremendous payoff. Once scientists understand the social behavior of viruses, they may be able to turn viruses against one another.
Turning the Tables
In the 1990s, evolutionary biologists were able to help inform the development of antiviral medicines. When people with HIV took a single antiviral drug, the virus quickly evolved the ability to evade it. But when doctors instead prescribed medicines that combined three antivirals, it became much harder for the viruses to escape them all. The chance that a virus could gain mutations to resist all three drugs was astronomically small. As a result, HIV drug cocktails remain effective even today.
Sociovirologists are now investigating whether evolutionary biology can again help in the fight against viruses. They are looking for vulnerabilities in the way viruses cheat and cooperate, which they can exploit to bring infections to a halt. “We see it as turning the tables on the virus,” Vignuzzi said.
Vignuzzi and his colleagues tested this idea in mice with Zika virus. They engineered incomplete Zika viruses that could ruthlessly exploit functional ones. When they injected these cheaters into infected mice, the population of functional viruses inside the animals quickly collapsed. The French company Meletios Therapeutics has licensed Vignuzzi’s cheater viruses and has been developing them as a potential antiviral drug for a variety of viruses.
At New York University, Ben tenOever and his colleagues are engineering what might be an even more effective cheater from influenza viruses. They’re taking advantage of a quirk of virus biology: Every now and then, the genetic material from two viruses that infect the same cell will end up packaged into one new virus. They wondered if they could create a cheating virus that could readily invade the genome of a functional influenza virus.

Introduction
The NYU team harvested incomplete viruses from influenza-infected cells. From this batch, they identified a super-cheater that was remarkably good at slipping its genes into fully functional influenza viruses. The resulting hybrid virus was bad at replicating, thanks to the cheater’s disruption.
To see how this super-cheater would perform as an antiviral, tenOever and his colleagues packaged it into a nasal spray. They infected mice with a lethal strain of influenza and then squirted the super-cheater into the animals’ noses. The super-cheater virus was so good at exploiting functional viruses and slowing their replication that the mice managed to recover from the flu within a couple weeks. Without help from the super-cheaters, the animals died.
The researchers got even better results when they sprayed the super-cheaters into the noses of mice before they got infected. The super-cheaters lay in wait inside the mice and attacked the functional flu viruses as soon as they arrived.
Then tenOever and his colleagues moved to ferrets for their experiments. Ferrets experience influenza infections more like humans do: In particular, unlike with mice, influenza viruses will readily spread from a sick ferret to a healthy one in an adjacent cage. The scientists found that the nasal spray quickly drove down the number of flu viruses in infected ferrets, just as they saw in mice. However, the scientists got a surprise when they looked at the viruses that the infected ferrets passed to healthy animals. They transmitted not only normal viruses but also super-cheaters stowed away inside their protein shells.
RELATED:
- Viruses Can Scatter Their Genes Among Cells and Reassemble
- Viruses Have a Secret, Altruistic Social Life
- How Many Microbes Does It Take to Make You Sick?
- Viruses Would Rather Jump to New Hosts Than Evolve With Them
That finding raises the tantalizing possibility that super-cheaters might be able to stop the spread of a new strain of influenza. If people received sprays of super-cheater viruses, they could rapidly recover from infections. And if they did pass on the new virus strain to others, they would also pass along the super-cheater to stop it. “It’s a pandemic neutralizer,” tenOever said.
That’s true in concept, at least. TenOever would need to run a clinical trial in humans to see if it would work as it does in animals. However, regulators have had qualms about approving such an experiment, he said, as that would not simply be giving people a drug that would work on viruses in their own bodies, but also one that could spread to others, whether they consented to it or not. “That seems to be the kiss of death,” tenOever said, for his hopes of turning the science of social viruses into medicine.
Díaz-Muñoz thinks that it’s right to be cautious about harnessing sociovirology when we still have so much to learn about it. It’s one thing to create medicines from inert molecules. It’s quite another to deploy the social life of viruses. “It is a living, evolving thing,” Díaz-Muñoz said.