INTRODUCTION
Mammography has been proven to detect breast cancer at an early stage and, when followed up with appropriate diagnosis and treatment, to reduce mortality from breast cancer. For women at increased risk of breast cancer, other screening technologies also may contribute to the earlier detection of breast cancer, particularly in women under the age of 40 years for whom mammography is less sensitive. The American Cancer Society (ACS) guideline for the early detection of breast cancer, last updated in 2003, stated that women at increased risk of breast cancer might benefit from additional screening strategies beyond those offered to women at average risk, such as earlier initiation of screening, shorter screening intervals, or the addition of screening modalities (such as breast ultrasound or magnetic resonance imaging [MRI]) other than mammography and physical examination. However, the evidence available at the time was insufficient to justify recommendations for any of these screening approaches. The ACS recommended that decisions about screening options for women at significantly increased risk of breast cancer be based on shared decision making after a review of potential benefits, limitations, and harms of different screening strategies and the degree of uncertainty about each.1
Although there still are limitations in the available evidence, additional published studies have become available since the last update, particularly regarding use of breast MRI. The ACS guideline panel has sought to provide additional guidance to women and their health care providers based on these new data.
BACKGROUND
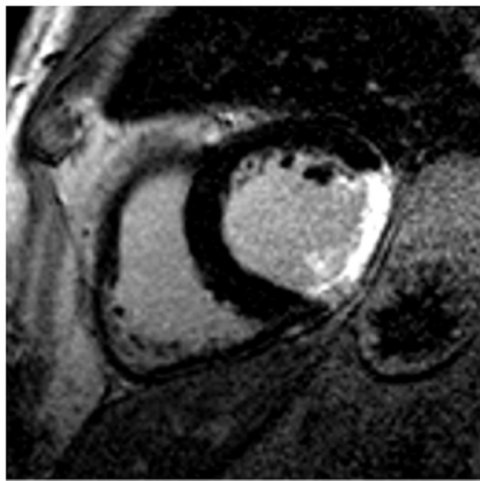
MRI
MRI utilizes magnetic fields to produce detailed cross-sectional images of tissue structures, providing very good soft tissue contrast. Contrast between tissues in the breast (fat, glandular tissue, lesions, etc.) depends on the mobility and magnetic environment of the hydrogen atoms in water and fat that contribute to the measured signal that determines the brightness of tissues in the image. In the breast, this results in images showing predominantly parenchyma and fat, and lesions, if they are present. A paramagnetic small molecular gadolinium-based contrast agent is injected intravenously to provide reliable detection of cancers and other lesions. Thus, contrast enhanced MRI has been shown to have a high sensitivity for detecting breast cancer in high-risk asymptomatic and symptomatic women, although reports of specificity have been more variable.2, [3], [4], [5], [6], [7]–8 This high signal from enhancing lesions can be difficult to separate from fat, leading to the use of subtraction images or fat suppression, or both, to assess disease. Because parenchymal tissue also enhances, but generally more slowly than malignant lesions, and also because contrast can wash out rapidly from some tumors, it is important to look at images at an early time point after contrast injection (typically 1 to 3 minutes). MRI examinations may involve examining images at one time point or, more often, will collect a preinjection image with sequential sets of images after contrast injection (dynamic contrast-enhanced [DCE]-MRI). Both the appearance of lesions and, where available, the uptake and washout pattern can be used to identify malignant disease and discriminate it from benign conditions.
These techniques, which have been widely employed for assessing symptomatic disease, have recently been shown to provide good sensitivity as a screening tool for breast cancer in women at increased risk based on family history.9, [10], [11], [12], [13]–14 The approach requires appropriate techniques and equipment, together with experienced staff. Higher quality images are produced by dedicated breast MRI coils, rather than body, chest, or abdominal coils.
IDENTIFICATION OF WOMEN WITH A HIGH RISK OF BREAST CANCER
Three approaches are available for identifying women with a high risk of breast cancer: family history assessment, genetic testing, and review of clinical history. All contribute to identifying women who are candidates for breast MRI screening.
Family History
Although a high proportion of women in the general population have at least one relative with breast cancer, for the majority of these women, this “family history” either does not increase risk at all (ie, the cancer was sporadic) or is associated with, at most, a doubling of lifetime risk (due to either shared environmental risk factors or an inherited gene of low penetrance). Only 1% to 2% of women have a family history suggestive of the inheritance of an autosomal dominant, high-penetrance gene conferring up to an 80% lifetime risk of breast cancer. In some families, there is also a high risk of ovarian cancer. Features of the family history which suggest the cancers may be due to such a high-penetrance gene include 2 or more close (generally first- or second-degree) relatives with breast or ovarian cancer; breast cancer occurring before age 50 years (premenopausal) in a close relative; a family history of both breast and ovarian cancer; one or more relatives with 2 cancers (breast and ovarian cancer or 2 independent breast cancers); and male relatives with breast cancer.15, [16], [17]–18
Two breast/ovarian cancer susceptibility genes, BRCA1 and BRCA2, have been identified.19,20 Inherited mutations in these genes can be found in approximately 50% of families in which an inherited risk is strongly suspected based on the frequency and age of onset of breast cancer cases, and in most families in which there is a much higher than expected incidence of both breast and ovarian cancer.
Several models can assist clinicians to estimate breast cancer risk or the likelihood that a BRCA mutation is present (Online Supplemental Material). The Gail, Claus, and Tyrer-Cusick models estimate breast cancer risk based on family history, sometimes in combination with other risk factors, such as reproductive history or prior breast biopsies.16,21, [22]–23 Although risk prediction is generally similar for the different models, an individual woman’s risk estimate may vary with different models.21,24,25
Two decision models have been developed to estimate the likelihood that a BRCA mutation is present, BRCAPRO18,26 and the Breast and Ovarian Analysis of Disease Incidence and Carrier Estimation Algorithm (BOADICEA)27; the BOADICEA model also provides estimates of breast cancer risk (Online Supplemental Material).
Genetic Testing
The prevalence of BRCA mutations is estimated to be between 1/500 and 1/1,000 in the general population28; however, in women of Jewish ethnicity, the prevalence is 1/50.29,30 Women with cancer-predisposing mutations in either BRCA1 or BRCA2 have an increased risk of both breast and ovarian cancer. From population-based studies, women with BRCA1 mutations are estimated to have a 65% risk by age 70 years for developing breast cancer (95% confidence interval [CI], 44% to 78%); the corresponding risk for BRCA2 mutations is 45% (95% CI, 31% to 56%).31 Risks estimated from cancer-prone families seen in referral centers are higher, with limit of risk in the 85% to 90% range.31 These mutations follow an autosomal dominant pattern of transmission, which means that the sister, mother, or daughter of a woman with a BRCA mutation has a 50% chance of having the same mutation.
The benefits and risks of genetic testing are beyond the scope of this article, but are reviewed in the American Society of Clinical Oncology policy statement update on genetic testing for cancer susceptibility.32 Genetic testing for a BRCA1 or BRCA2 mutation is generally offered to adult members of families with a known BRCA mutation, or to women with at least a 10% likelihood of carrying such a mutation, based on either validated family history criteria or one of the above-mentioned models. If a woman from a family in which a BRCA mutation has been previously identified does not have that mutation, one can generally safely conclude that her breast cancer risk is no higher than it would have been if she did not have a family history of breast cancer. However, in a high-risk family without a known mutation, failure to find a mutation in a particular member does not reduce her risk estimate.
A high risk of breast cancer also occurs with mutations in the TP53 gene (Li-Fraumeni syndrome) and the PTEN gene (Cowden and Bannayan-Riley-Ruvalcaba syndromes).33 Accurate prevalence figures are not available, but these conditions appear to be very rare.34,35
Clinical Indicators of Risk
Some clinical factors are associated with substantial breast cancer risk. Among women with Hodgkin disease, increased breast cancer risk has been consistently and significantly associated with mantle field radiation treatment. In several studies of women treated between 1955 and 1995, risk was inversely related to age at treatment in patients diagnosed between the ages of 10 to 30 years, with only slight or no increased risk when diagnosis was before age 10 years or after age 30 years.36, [37], [38], [39], [40]–41 Risk following treatment with radiation and chemotherapy was half that of treatment with radiation alone in two studies,39,42 which may reflect the effect of chemotherapy on earlier onset of menopause; risk was equivalent in a third study.43 Risk of breast cancer significantly increased 15 to 30 years after radiation therapy.41 More recently, treatment approaches have used lower doses of radiation and limited-field radiotherapy. In one study, which compared patients who received radiation therapy in 1966 to 1974 and 1975 to 1985, treatment in the later timeframe was not related to increased risk of breast cancer after a median follow up of 13 years, whereas patients treated between 1966 and 1974 were at increased risk, suggesting that Hodgkin disease survivors treated with current approaches will not face substantially increased breast cancer risk.44
Lobular carcinoma in situ (LCIS) and atypical lobular hyperplasia (ALH), together described as lobular neoplasia, are associated with substantially increased risk of subsequent breast cancer, with lifetime risk estimates ranging from 10% to 20%.45 This equates to a continuous risk of about 0.5% to 1.0% per year. The invasive cancers may be ipsilateral or contralateral, are usually invasive lobular cancers, and more than 50% of these diagnoses occur more than 15 years after the original diagnosis of LCIS. Similar findings have been reported by Fisher et al,46 describing a 12-year update of 180 women with LCIS who were treated with local excision alone and followed by the National Surgical Adjuvant Breast Project (NSABP), as well as Li et al, who described the risk of invasive breast cancer among 4,490 LCIS patients using Surveillance, Epidemiology, and End Results (SEER) data between 1988 to 2001.47
A typical ductal hyperplasia (ADH) is part of the continuum of ductal proliferative breast diseases ranging from usual ductal hyperplasia to ductal carcinoma in situ (DCIS). The literature review by Arpino et al45 suggests a 4- to 5-fold increased risk of invasive breast cancer (compared with a 6- to 10-fold risk with LCIS) at a median follow up of 17 years, which is doubled if the woman has an associated family history of breast cancer. It is unclear, however, what percentage of the women with this family history and ADH are at this significantly increased risk because they are carriers of a BRCA1 or 2 gene mutation.
Mammographic density has been shown to be a strong independent risk factor for the development of breast cancer.48, [49], [50]–51 In several studies, women with the most breast density were found to have a 4- to 6-fold increased risk of breast cancer, compared with women with the least dense breasts.52, [53], [54], [55]–56 For example, women with 75% or higher mammographic density had a more than five-fold increased risk of breast cancer, compared with women with less than 1% density.57 In addition, it has been shown that malignant tumors of the breast are more likely to arise in the areas of greatest mammographic density, compared with the more fatty areas of the breast.58
The absolute risk of contralateral breast cancer in women with a personal history of breast cancer is estimated to be 0.5% to 1% per year, or 5% to 10% during the 10 years following diagnosis, significantly higher than that of the general population.59 Hormone therapy and/or chemotherapy for the primary cancer is likely to subsequently lower the risk of contralateral breast cancer.
EVIDENCE AND RATIONALE
Evidence of Efficacy from MRI Screening Studies
In the mid to late 1990s, at least 6 prospective, nonrandomized studies were initiated in The Netherlands, the United Kingdom (UK), Canada, Germany, the United States (US), and Italy to determine the benefit of adding annual MRI to (film) mammography for women at increased risk of breast cancer. Some of the studies included ultrasound and/or clinical breast examination, as well. Despite substantial differences in patient population (age, risk, etc.) and MRI technique, all reported significantly higher sensitivity for MRI compared with mammography (or any of the other modalities). All studies that included more than one round of screening reported interval cancer rates below 10%. Participants in each of these 6 studies had either a documented BRCA1 or BRCA2 mutation or a very strong family history of breast cancer. Some of the studies included women with a prior personal history of breast cancer.
Kriege et al screened 1,909 unaffected women aged 25 to 70 years with an estimated 15% or higher lifetime risk of breast cancer (19% proven to have a BRCA mutation) at 6 centers across The Netherlands.9 After a median of 3 rounds of screening, 50 breast cancers (44 invasive) were diagnosed. Eighty percent of the invasive cancers were detected by MRI, compared with 33% by mammography. However, mammography outperformed MRI for detecting DCIS. Of the invasive cancers, 43% were 1 cm or smaller in diameter, and 33% had spread to axillary lymph nodes. The specificity of MRI was 90%, compared with 95% for mammography.
Leach et al screened 649 unaffected women aged 35 to 49 years who had at least a 25% lifetime risk of breast cancer (19% proven to have a BRCA mutation) at 22 centers in the UK.11 After a median of 3 rounds of screening, 35 cancers (29 invasive) were diagnosed. Sensitivity of MRI was 77%, compared with 40% for mammography, with specificities of 81% and 93%, respectively. MRI was most sensitive and mammography least sensitive for women with BRCA1 mutations. Forty-five percent of the cancers were 1 cm or less in size, and 14% had spread to axillary lymph nodes. There were two interval cancers.
Warner et al screened 236 women aged 25 to 65 years with a BRCA mutation at a single center in Toronto for up to 3 years and detected 22 cancers (16 invasive).14 Sensitivity of MRI was 77%, compared with 36% for mammography, with 50% of the cancers 1 cm or smaller, and 13% were node positive. There was one interval cancer. Specificity was 95% for MRI and 99.8% for mammography.
Kuhl et al screened 529 women aged 30 years and older with a lifetime breast cancer risk of at least 20% at a single center in Bonn for a mean of 5 years.10 They detected 43 cancers (34 invasive), with 1 interval cancer. The sensitivity of MRI was 91%, compared with 33% for mammography. The node positive rate was 16%. Specificity of both MRI and mammography was 97%.
The International Breast MRI Consortium screened 390 women aged 25 years and older with more than a 25% lifetime risk of breast cancer at 13 centers (predominantly in the US) on a single occasion.12 Four cancers were found by MRI, and only one of these by mammography. However, because the patients were not followed after screening, the false-negative rate could not be determined. MRI specificity was 95%, compared with 98% for mammography.
In a study in Italy with 9 participating centers, Sardanelli et al screened 278 women aged 25 years and older; 27% carried a BRCA mutation or had a first-degree relative with a BRCA mutation.13 After a median of 1.4 rounds of screening, 18 cancers (14 invasive) were found. MRI sensitivity was 94%, compared with 59% for mammography, 65% for ultrasound, and 50% for clinical breast examination. MRI specificity was 99%.
Overall, studies have found high sensitivity for MRI, ranging from 71% to 100% versus 16% to 40% for mammography in these high-risk populations. Three studies included ultrasound, which had sensitivity similar to mammography. The Canadian, Dutch, and UK studies9,11,14 reported similar sensitivity (71% to 77%) within CIs for MRI, although the single-center study from Germany10 reported a higher sensitivity, which may reflect the concentration of radiological practice and higher patient volume per radiologist at a single center. There is evidence of a learning curve for radiologists conducting MRI breast screening, with the number of lesions investigated falling with experience.60 The three multicenter studies reflect the likely initial effectiveness of this modality in a population context, and it is expected that, with training and advances in technology, sensitivity will increase further.
Table 2 provides a summary of these six screening studies.
Table TABLE 2. Published Breast MRI Screening Study Results
Most of the available data are based on screening women at high risk due to family history and/or genetic mutations. More recently, smaller studies have provided information on the potential benefit of MRI screening for women with clinical factors that put them at increased risk. Preliminary data were obtained from one retrospective study, in which Port et al61 reviewed the screening results of 252 women with biopsy-confirmed LCIS and 126 women with atypical hyperplasia (either ductal or lobular), of whom half were screened with annual mammography and biennial clinical exams and half were also screened with MRI. The women who were screened with MRI were younger and more likely to have a strong family history. MRI screening offered a small advantage to patients with LCIS, but not atypical hyperplasia, and also resulted in increased biopsies: 6 cancers were detected by MRI in 5 women with LCIS (4% of patients undergoing MRI), and none were detected in women with atypical hyperplasia. Biopsies were recommended for 25% of MRI screened patients; 13% of biopsies had a cancer detected. All of the cancers in women screened with MRI were Stage 0 to I, whereas all of the cancers in women who were not screened with MRI were Stage I to II. Cancer was detected on the first MRI in 4 of 5 patients. The sensitivity of MRI was 75%, the specificity was 92%, and the positive predictive value was 13%.
Technological Limitations and Potential Harms Associated with MRI Screening
Although the efficacy of breast MRI has been demonstrated, it does not achieve perfect sensitivity or specificity in women undergoing screening, and as such, the issue of adverse consequences for women who do, but especially those who do not, have breast cancer is important to address. As with mammography and other screening tests, false negatives after MRI screening can be attributed to inherent technological limitations of MRI, patient characteristics, quality assurance failures, and human error; false positives also can be attributed to these factors, as well as heightened medical-legal concerns over the consequence of missed cancers. A patient’s desire for definitive findings in the presence of a low-suspicion lesion may also contribute to a higher rate of benign biopsies. The consequences of all these factors include missed cancers, with potentially worse prognosis, as well as anxiety and potential harms associated with interventions for benign lesions.
The specificity of MRI is significantly lower than that of mammography in all studies to date, resulting in more recalls and biopsies. Call-back rates for additional imaging ranged from 8% to 17% in the MRI screening studies, and biopsy rates ranged from 3% to 15%.9, [10], [11], [12], [13]–14 However, several researchers have reported that recall rates decreased in subsequent rounds of screening: prevalence screens had the highest false-positive rates, which subsequently dropped to less than 10%.9,62,63 Most call backs can be resolved without biopsy. The call-back and biopsy rates of MRI are higher than for mammography in high-risk populations; while the increased sensitivity of MRI leads to a higher call-back rate, it also leads to a higher number of cancers detected. The proportion of biopsies that are cancerous (positive predictive value) is 20% to 40%.9, [10], [11], [12], [13]–14 Since false-positive results appear to be common, more data are needed on factors associated with lower specificity rates.
Table 3 compares the likelihood of detection and follow-up tests for women who underwent screening MRI and mammography in two screening studies (Dutch and UK). The study populations differed, with the Dutch study having a wider age group and lower risk category, compared with the UK study.9,11 This affected both the prevalence of cancer and the pick-up rate by modality in the two studies. These results, drawn from two trials, demonstrate the relatively high recall rate in the high-risk population, as well as the fact that MRI is a relatively new technique. Despite the high number of recalls, because of the high cancer rate, the rate of benign surgical biopsy in the UK study per cancer detected was similar to that experienced in the population-based national breast screening service. Recalls will inevitably lead to additional investigations, many of which will not demonstrate that cancer is present.
Table TABLE 3. Rates of Detection and Follow-up Tests for Screening MRI Compared with Mammography
Given the high rate of cancer combined with the risk of false-positive scans in a high-risk population undergoing MRI-based screening, the psychological health of these women merits study. In a subgroup of 611 women in the UK study, 89% reported that they definitely intended to return for further screening, and only 1% definitely intended not to return. However, 4% found breast MRI “extremely distressing,” and 47% reported still having intrusive thoughts about the examination 6 weeks afterward.64
In a sample of 357 women from the Dutch study, psychological distress remained within normal limits throughout screening for the group as a whole. However, elevated breast cancer-specific distress related to screening was found in excessive (at least once per week) breast self-examiners, risk overestimators, and women closely involved in the breast cancer case of a sister. At least 35% of the total sample belonged to one of these subgroups. It was recommended that patients in one of these vulnerable subgroups be approached for additional psychological support.65
In a small sample of women from the Toronto study followed over a course of 2 years, there was no evidence of any effect on global anxiety, depression, or breast cancer-related anxiety.66 In another sample of 57 women, almost 50% had elevated baseline general and/or breast cancer-specific anxiety, but in 77% of cases this was attributed by the patients to life events, including relatives with cancer. A nonsignificant increase in general anxiety and breast cancer-related anxiety, compared with baseline, was found in the subset of women recalled for further imaging or biopsies.67 Follow-up time is still insufficient to determine whether anxiety scores return to baseline once the work up has been completed.
There is a special responsibility to alert patients to this technology, with its potential strengths and harms, and to be encouraging, while allowing for shared decision making. The interplay between risks, benefits, limitations, and harms is complicated by the fact that individual women likely will weigh these differently depending on their age, values, perception of risk, and their understanding of the issues. Steps should be taken to reduce anxiety associated with screening and the waiting time to diagnosis, and conscientious efforts should be made to inform women about the likelihood of both false-negative and false-positive findings. How information is conveyed to the patient greatly influences the patient’s response: it is important that providers not convey an undue sense of anxiety about a positive MRI finding. While the high rate of biopsies and further investigations is acceptable in women with a high risk of breast cancer, the number of such investigations in women at lower risk will be much higher than would be appropriate, leading to the need to counsel women in lower risk categories that MRI screening is not advisable and that the harms are believed to outweigh the benefits. Such advice needs to be based on considerations of family history, genetic mutation status, other risk factors, age, and mammographic breast density.
There are substantial concerns about costs of and limited access to high-quality MRI breast screening services for women with familial risk. In addition, MRI-guided biopsies are not widely available. With many communities not providing MRI screening and with MRI-guided biopsies not widely available, it is recognized that these recommendations may generate concerns in high-risk women who may have limited access to this technology.
The ability of MRI to detect breast cancer (both invasive and in situ disease) is directly related to high-quality imaging, particularly the signal-to-noise ratio, as well as spatial resolution of the MR image. In order to detect early breast cancer (ie, small invasive cancers, as well as DCIS), simultaneous imaging of both breasts with high spatial resolution is favored. High spatial resolution imaging should be performed with a breast coil on a high field magnet with thin slices and high matrix (approximately 1 mm in-plane resolution). These technical parameters are considered to be the minimal requirements to perform an adequate breast MRI study. The ability to perform MRI-guided biopsy is absolutely essential to offering screening MRI, as many cancers (particularly early cancers) will be identified only on MRI. The American College of Radiology (ACR) is currently developing an accreditation process for performing breast MRI, and, in addition to the performance of high spatial resolution images, the ability to perform MRI intervention (ie, needle localization and/or biopsy) will be essential in order to obtain accreditation by this group. Accreditation will be voluntary and not mandatory. This guideline will likely be available in 2007.
There is a learning curve with respect to interpretation for radiologists. Published trial sites that experience a high volume of cases are experienced, but community practice groups have reported call-back rates over 50% in the majority of the studies that are interpreted. Experience and familiarity with patterns of enhancement, normal and possibly abnormal, are thought to decrease recall rates and increase positive biopsy rates. The ACR accreditation process will stipulate a minimum number of exams that must be read for training purposes and a minimum number for ongoing accreditation. Sites performing breast MRI are encouraged to audit their call-back rates, biopsy rates, and positive biopsy rates.
Cost-effectiveness
Only limited data are available on the cost-effectiveness of breast MRI screening. One recent study modeled cost-effectiveness for adding MRI to mammography screening for women of different age groups who carry a BRCA1 or BRCA2 mutation.68 The authors concluded that the cost per quality-adjusted life year (QALY) saved for annual MRI plus film mammography, compared with annual film mammography alone, varied by age and was more favorable in carriers of a mutation in BRCA1 than BRCA2 because BRCA1 mutations confer higher cancer risk, and higher risk of more aggressive cancers, than BRCA2 mutations.31 Estimated cost per QALY for women aged 35 to 54 years was $55,420 for women with a BRCA1 mutation and $130,695 for women with a BRCA2 mutation. Cost-effectiveness was increased when the sensitivity of mammography was lower, such as in women with very dense breasts on mammography: estimated costs per QALY were $41,183 for women with a BRCA1 mutation and $98,454 for women with a BRCA2 mutation with dense breast tissue. The most important determinants of cost-effectiveness were breast cancer risk, mammography sensitivity, MRI cost, and quality of life gains from MRI.
An evaluation of the cost-effectiveness of the UK study69 has determined that the incremental cost per cancer detected for women at approximately 50% risk of carrying a BRCA gene mutation was $50,911 for MRI combined with mammography over mammography alone. For known mutation carriers, the incremental cost per cancer detected decreased to $27,544 for MRI combined with mammography, compared with mammography alone. Analysis supporting the introduction of targeted MRI screening in the UK for high-risk women70 identified the incremental cost of combined screening per QALY in 40- to 49-year-old women as $14,005 for a BRCA1 carrier with a 31% 10-year riskthe group in which MRI screening is seen to be most effective; $53,320 for women with a 12% 10-year risk; and $96,379 for women with a 6% 10-year risk. For the 30- to 39-year-old age range, the incremental costs per QALY are $24,275 for a BRCA1 carrier with an 11% 10-year risk and $70,054 for a women with a 5% 10-year risk. Based on these estimates, which are based on costs within the UK National Health Service, MRI screening will be offered to women at familial risk aged 30 to 39 years at a 10-year risk greater than 8%, and to women at familial risk aged 40 to 49 years at a 10-year risk greater than 20%, or greater than 12% when mammography has shown a dense breast pattern.
Evidence Supporting Benefit of MRI Screening Among Women in Different Risk Categories
The guideline recommendations were based on consideration of (1) estimates of level of risk for women in various categories and (2) the extent to which risk groups have been included in MRI studies, or to which subgroup-specific evidence is available. Because of the high false-positive rate of MRI screening, and because women at higher risk of breast cancer are much more likely to benefit than women at lower risk, screening should be recommended only to women who have a high prior probability of breast cancer. There is growing evidence that breast cancer in women with specific mutations may have biological and histological features that differ from sporadic cancers. This may result in observed variations in the sensitivity of MRI relative to mammography in detecting cancer in women with a BRCA mutation and those at high familial risk, but without mutations in these genes.11
Women at Increased Risk Based on Family History
The threshold for defining a woman as having significantly elevated risk of breast cancer is based on expert opinion. Any woman with a BRCA1 or BRCA2 mutation should be considered at high risk. The panel has not restricted its recommendations only to women with BRCA mutations because BRCA testing is not always available or informative, and other risk indicators identify additional subsets of women with increased breast cancer risk. If mutation testing is not available, has been done and is noninformative, or if a woman chooses not to undergo testing, pedigree characteristics suggesting high risk may be considered. Very careful family history analysis is required, using tools such as BRCAPRO.18,26 Risk assessment is likely to offer the greatest potential benefit for women under the age of 40 years. Table 4 provides examples of women with a family history indicative of moderate and high risk. The online supplemental material provides guidance for accessing and using risk assessment models.
Table TABLE 4. Breast Cancer Risks for Hypothetical Patients, Based on 3 Risk Models
Women at Increased Risk Based on Clinical Factors
Additional factors that increase the risk of breast cancer, and thus may warrant earlier or more frequent screening, include previous treatment with chest irradiation (eg, for Hodgkin disease), a personal history of LCIS or ADH, mammographically dense breasts, and a personal history of breast cancer, as discussed above. There are little data to assess the benefit of MRI screening in women with these risk factors. Women at increased risk or who are concerned about their risk may find it helpful to have their provider clarify the bases for MRI screening recommendations, as well as areas of uncertainty. For some women, mammography may be as effective as for women at average risk, and MRI screening may have little added benefit. In contrast, mammography is less effective in women with very dense breasts, and MRI screening may offer added benefit.
Women who have received radiation treatment to the chest, such as for Hodgkin disease, compose a well-defined group that is at high risk. Although evidence of the efficacy of MRI screening in this group is lacking, it is expected that MRI screening might offer similar benefit as for women with a strong family history, particularly at younger ages and within 30 years of treatment. Because of the high risk of secondary breast cancer in this group, MRI screening is recommended based on expert consensus opinion.
While lifetime risk of breast cancer for women diagnosed with LCIS may exceed 20%, the risk of invasive breast cancer is continuous and only moderate for risk in the 12 years following local excision.46 Only one MRI screening study has included a select group of women with LCIS,61 which showed a small benefit over mammography alone in detecting cancer. This benefit was not seen in patients with atypical hyperplasia. MRI use should be decided on a case-by-case basis, based on factors such as age, family history, characteristics of the biopsy sample, breast density, and patient preference.
Although there have been several trials reported looking at the accuracy and positive predictive value of MRI and mammography in women with high breast density, all of these trials have been conducted in women with known or highly-suspected malignancies within the breast.71, [72], [73]–74 To this point, there has been no Phase III randomized trial reported that has shown a reduction in either mortality or in the size of diagnosed breast cancer when comparing breast MRI with mammography in women with high mammographic density.
Scant data are available for MRI screening of women with a personal history of breast cancer. In one study, MRI detected more cancers in women who had both a personal history and a family history, compared with women at high risk based on family history alone.75 While women with a previous diagnosis of breast cancer are at increased risk of a second diagnosis, the ACS panel concluded that the estimated absolute lifetime risk of 10% does not justify a recommendation for MRI screening at the present time.
Limitations of Evidence from MRI Studies and Research Needs
Assiduous attempts were made to base recommendations on solid evidence. However, outcome data from screening MRI studies are not sufficient to form a solid basis for many of the recommendations. It was therefore necessary to rely on available inferential evidence and expert opinion to provide the guidance needed for patients and their health care providers.
Although the literature shows very good evidence for greater sensitivity of MRI than mammography and good evidence for a stage shift toward earlier, more favorable tumor stages by MRI in defined groups of women at increased risk, there are still no data on recurrence or survival rates, and therefore, lead-time bias is still a concern. Further, a large randomized, mortality endpoint study is unlikely to take place, and it will be necessary in the foreseeable future to rely on evidence of stage of disease and types of cancers. In the absence of randomized trials, recurrence and survival data will come from observational study designs.
The age at which screening should be initiated for women at high risk is not well established. The argument for early screening is based on the cumulative risk of breast cancer in women with BRCA1 mutations and a strong family history of early breast cancer, which is estimated to be 3% by age 30 years and 19% by age 40 years.76 Population-based data also indicate that risk for early breast cancer is increased by a family history of early breast cancer.16 Based on these observations, some experts have suggested that breast cancer screening begin 5 to 10 years before the earliest previous breast cancer in the family. In 1997, an expert panel suggested that screening be initiated at some time between the ages of 25 and 35 years for women with a BRCA1 or BRCA2 mutation.77 Because these recommendations were based on limited observational data, the decision regarding when to initiate screening should be based on shared decision making, taking into consideration individual circumstances and preferences. No data are available related to the effectiveness of screening women beyond age 69 years with MRI and mammography versus mammography alone; most of the current data are based on screening in younger women, and thus, similar investigations are needed in older age cohorts. For most women at high risk, screening with MRI and mammography should begin at age 30 years and continue for as long as a woman is in good health.1
Most of the available data are based on annual MRI screening; there is a lack of evidence regarding shorter or longer screening intervals. Further, while good data are available for the first screening exam (ie, the “prevalent screen”), considerably less data are available from subsequent screening exams (ie, “incidence screens”), and the available data include relatively short follow-up times. Most studies of annual MRI have shown few interval cancers, certainly fewer than with mammography. Given the probably shorter duration of the detectable preclinical phase, or sojourn time, in women with BRCA mutations, MRI has demonstrated superiority to mammography in this regard. Therefore, to the best of our knowledge, MRI should be performed annually. However, in view of data suggesting that tumor doubling time in women with an inherited risk decreases with age,78 it is conceivable that older women can safely be screened less frequently than younger women. The available evidence is limited, and additional research regarding optimal screening interval by age and risk status is needed.
Some experts recommend staggering MRI screening and mammography screening every 6 months. The potential advantage of this approach is that it may reduce the rate of interval cancers. Other experts recommend MRI and mammography at the same time or within a short time period. This approach allows for the results of both screening tests to be interpreted together and reported to the patient at the same time. All of the clinical trials screened participants with both MRI and mammography at the same time. There is no evidence to support one approach over the other. For the majority of women at high risk, it is critical that MRI screening be provided in addition to, not instead of, mammography, as the sensitivity and cancer yield of MRI and mammography combined is greater than for MRI alone. However, where there is a concern about raised radiation sensitivity, it may be advisable to employ MRI alone despite the overall lower sensitivity.
In order to pursue answers to some of the unresolved questions related to the use of MRI and mammography to screen women at increased risk, it is important to develop creative strategies related to data gathering and study design. Multicenter studies can result in greater efficiency in accumulating sufficiently large enough data sets in this subgroup of women. Conventional study designs with randomization may prove difficult given the potential advantage of adding MRI to mammography in higher-risk groups, and thus, design strategies that utilize surrogate markers and historic controls may prove both more practical and feasible. To move forward, we encourage the development of a simple, common data collection protocol to capture information from the growing number of centers that offer MRI and formal systems to collect outcome data. Because many insurers presently cover MRI screening for high-risk women, it may be economical to do prospective surveillance studies since screening costs are covered by third parties. A common surveillance protocol could permit pooling of data, much like presently is done within the framework of the National Cancer Institute’s Breast Cancer Surveillance Consortium, a collaborative network of seven mammography registries in the United States with linkages to tumor and/or pathology registries that was organized to study the delivery and quality of breast cancer screening and related patient outcomes in the United States.79 We also encourage seeking opportunities for broad international research collaboration on study questions of common interest.
Several further clinical trials of screening women at increased risk of breast cancer are underway, including an international study of MRI and ultrasound in conjunction with the International Breast MRI Consortium and Cancer Genetics Network, and the American College of Radiology Imaging Network (ACRIN) 666 screening trial of mammography compared with ultrasound. An amendment to the ACRIN trial, 6666, will screen patients with one round of MRI.
CONCLUSION
Often no available screening modality is uniquely ideal. For breast MRI, there is an increasing body of observational data showing that screening can identify cancer in patients of specific risk groups, ie, high-risk patients facing a lifetime risk of ∼20–25% or greater related to family history as estimated by one or more of the different risk models. We have specified a range of risk because estimates from the risk models vary and because each of the risk models is imperfect. Furthermore, these models likely will continue to be refined over time; therefore, these risk estimates for different family history profiles are likely to change. Thus, when estimating patient risk it is important to always be certain that the most current model is being used. In addition to family history, clinical factors as described earlier may be a relevant factor in individualized decisions about MRI screening when family history alone does not predict a risk of approximately 20–25%.
Several studies have demonstrated the ability of MRI screening to detect cancer with early-stage tumors that are associated with better outcomes. While survival or mortality data are not available, MRI has higher sensitivity and finds smaller tumors, compared with mammography, and the types of cancers found with MRI are the types that contribute to reduced mortality. It is reasonable to extrapolate that detection of noninvasive (DCIS) and small invasive cancers will lead to mortality benefit.
The guideline recommendations for MRI screening as an adjunct to mammography for women at increased risk of breast cancer take into account the available evidence on efficacy and effectiveness of MRI screening, estimates of level of risk for women in various categories based on both family history and clinical factors, and expert consensus opinion where evidence for certain risk groups is lacking. All of these groups of women should be offered clinical trials of MRI screening, if available. Women should be informed about the benefits, limitations, and potential harms of MRI screening, including the likelihood of false-positive findings. Recommendations are conditional on an acceptable level of quality of MRI screening, which should be performed by experienced providers in facilities that provide MRI-guided biopsy for the follow up of any suspicious results.