Epstein Barr disease stretches further than the infectious mononucleosis—with frequently overlooked influence on chronic diseases such as multiple sclerosis.
Tanya Francis, 45, couldn’t have predicted that a virus she encountered at 14 would drastically affect her health years later. Diagnosed with mononucleosis, a common adolescent ailment caused by the Epstein-Barr virus (EBV), Ms. Francis’s experience deviated from the norm. Rather than being a fleeting teenage illness, EBV marked the beginning of a long-term battle.
Ms. Francis’ ensuing struggle with fatigue, joint pain, vertigo, and a 2018 multiple sclerosis diagnosis reflects a wider narrative. Her experience sheds light on EBV’s complex and frequently overlooked influence on chronic diseases.
Unveiling the Epstein-Barr Virus
The Epstein-Barr virus, less familiar to many than the common cold but arguably as widespread, is stepping into the spotlight of medical research, revealing its complex role in numerous health issues.
While best known for causing infectious mononucleosis, often called the “kissing disease,” the influence of EBV stretches much further. “EBV is one of the most common human viruses,” explains Dr. Jeffrey Dunn, a neurologist at Stanford Medicine focusing on immune-mediated neurological diseases. “If you checked everybody for whether they’ve been exposed to Epstein Barr virus, 95 percent plus will have it.”
As a member of the herpesvirus family, EBV is a double-stranded DNA virus capable of remaining latent in the body. “Much like herpes simplex virus, once you’re infected with EBV, you can never eradicate it,” Paul Gisbert Auwaerter, M.D. and professor at Johns Hopkins University School of Medicine, told The Epoch Times. He emphasizes that this ability to lie dormant is central to the virus’s nature, allowing it to stay hidden for prolonged periods.
EBV is commonly passed through oral secretions, often in simple acts like sharing drinks or kissing. However, its transmission extends to blood transfusions, organ transplants, and breast milk. The presence of EBV in genital secretions further underscores its capacity to spread via multiple bodily fluids.
EBV infection typically occurs in childhood or adolescence, frequently producing mild or unnoticeable symptoms. In teens or young adults, it often manifests as infectious mononucleosis, marked by fever, sore throat, and swollen glands. But the true concern lies in what unfolds long after these initial symptoms subside.
A Spectrum of Linked Diseases
Beyond its role in causing mononucleosis, the Epstein-Barr virus is now recognized as a key player in various autoimmune and inflammatory diseases. What was once speculative is now backed by growing scientific evidence.
A pivotal study tracking over 10 million U.S. military recruits for two decades revealed a startling connection between EBV and multiple sclerosis (MS). The research found a 32-fold increase in MS risk post-EBV infection, shedding light on the virus’s possible role in autoimmune diseases.
Alberto Ascherio, M.D., Harvard epidemiologist and senior author, reflected on the study in a press release. “This is a big step because it suggests that most MS cases could be prevented by stopping EBV infection, and that targeting EBV could lead to the discovery of a cure for MS.”
While the exact mechanisms by which EBV may lead to MS are still under investigation, a 2022 Stanford study may offer a clue. The research highlighted a unique aspect of EBV’s interaction with MS. The virus contains elements mimicking brain and spinal cord proteins, leading the immune system to mistakenly attack the body’s nerve cells, a phenomenon termed “molecular mimicry.”
Beyond MS, EBV is linked to other autoimmune diseases such as lupus, Type 1 diabetes, and rheumatoid arthritis. These findings suggest that EBV’s role extends beyond dormancy, potentially triggering various autoimmune responses.
Research is also probing potential connections between EBV and gastrointestinal disorders, including irritable bowel syndrome and celiac disease.
In cancer research, EBV’s influence is notably significant. It contributes to cancers like Burkitt’s lymphoma, Hodgkin’s lymphoma, gastric cancer, and nasopharyngeal carcinoma. Dr. Dunn highlights, “It’s been estimated that there may be 200,000 cancer cases per year associated with EBV,” a number that becomes meaningful when considering public health and potential treatments, he explains.
“We’re dealing with a virus that has the capability to affect the body in multiple ways,” explains Dr. Auwaerter. He emphasizes, however, that while there’s a noticeable link between EBV and certain autoimmune diseases, the exact ways EBV influences these conditions remain to be fully understood by researchers.
The Immune System’s Role in EBV Activation
The Epstein-Barr virus is not just widespread—its true danger lies in its ability to manipulate the human immune system. Its threat often becomes pronounced when our natural defenses are weakened.
“It’s a delicate balance,“ Dr. Michael Bauerschmidt, chief medical officer at Deeper Healing Wellness Center, told The Epoch Times. ”The virus itself can remain harmless for years, but under certain conditions, it can become a formidable adversary.”
A key element is the immune response to EBV. Usually, a robust immune system keeps the virus in check. However, if the immune system is compromised due to stress, illness, or other factors, EBV may reactivate.
“The diagnosis is not the disease,” states Dr. Bauerschmidt. “Yes, EBV causes problems, but only because the individual immune system is unable to keep it contained.”
Factors weakening the immune system and possibly reactivating EBV are numerous. “It’s about everything,” Dr. Bauerschmidt explains, emphasizing lifestyle influences, particularly nutrition. A nutrient-deficient diet can weaken immune defenses, allowing EBV reactivation. Conversely, a nutrient-rich diet might strengthen the immune response against EBV.
Environmental elements also play a role. Dr. Bauerschmidt points to exposure to mold, heavy metals, pesticides, and electric and magnetic fields as factors that can weaken the immune system. “These environmental factors can create a perfect storm for EBV reactivation,” says Dr. Bauerschmidt.
Dr. Bauerschmidt asserts that the approach to understanding and managing EBV must be holistic. “Focusing solely on the virus is insufficient. We must consider the body’s entire ecosystem.” He advocates for a strong, balanced immune system as the primary defense.
Ben Galyardt, chiropractor and founder and CEO of F8 Well Centers, aligns with this view, particularly considering recent findings on Long COVID and EBV reactivation. A 2023 study showed higher EBV reactivation rates in COVID-19 patients. “A range of physical stressors can provoke EBV reactivation, initiating an inflammatory response within the body,” he notes.
Dr. Auwaerter, however, questions the effectiveness of merely boosting the immune system against EBV-linked conditions. Acknowledging the benefits of a healthy lifestyle, he cautions, “There’s no definitive proof that less immune activation or reactivation leads to less disease.”
He points out the complexity, especially with autoimmune conditions, where stimulating the immune system might be counterproductive. “The critical question is whether the issues stem directly from the virus or from the immune response,” he adds, underlining the intricacies of EBV-related health challenges.
Navigating the Challenges of Diagnosis
Diagnosing conditions associated with EBV is a complex task in medicine, largely due to the virus’s prevalence and dormant nature. A significant issue is that standard EBV tests often fail to provide clear insights into the virus’s active role in current health issues.
EBV testing typically involves checking for antibodies against specific EBV antigens to assess recent or past infections. According to the Centers for Disease Control (CDC), anti-VCA IgM appears early in an EBV infection and usually vanishes within four to six weeks, signifying a recent infection. On the other hand, anti-VCA IgG emerges in the acute phase, peaks at two to four weeks post-onset, and then remains for life, indicating past exposure. The simultaneous presence of VCA and EBNA antibodies generally suggests past infection, a common finding in adults.
However, Mr. Galyardt points out the limitations of these tests. “Since most adults have encountered EBV, standard tests like anti-VCA IgG, IgM, or EBNA offer limited information about ongoing health issues.” Although these tests can identify past exposure or acute infections, they don’t conclusively show whether EBV is currently affecting a patient’s health.
Mr. Galyardt suggests a more comprehensive diagnostic method, focusing on white blood cell counts. “A low white blood cell count coupled with a high lymphocyte percentage often indicates chronic viral infection, irrespective of EBV test results.” This approach considers the body’s overall state, not just specific EBV markers.
Interpreting EBV antibody tests requires considering the patient’s symptoms and medical history. The connection between EBV and various chronic conditions, like autoimmune diseases or cancers, isn’t widely acknowledged in general practice, potentially leading to diagnostic and treatment oversights.
While EBV testing can be instrumental in diagnosing conditions like infectious mononucleosis or chronic active Epstein-Barr Virus (CAEBV), Dr. Auwaerter recommends a cautious approach when it comes to testing for other issues, such as chronic fatigue, Long COVID, MS, lupus, or lymphoma. “In my opinion, there’s no benefit,” he remarks, highlighting that the scientific community is still working to fully understand how EBV is connected to various health conditions.
EBV Treatment: Searching for Effective Strategies
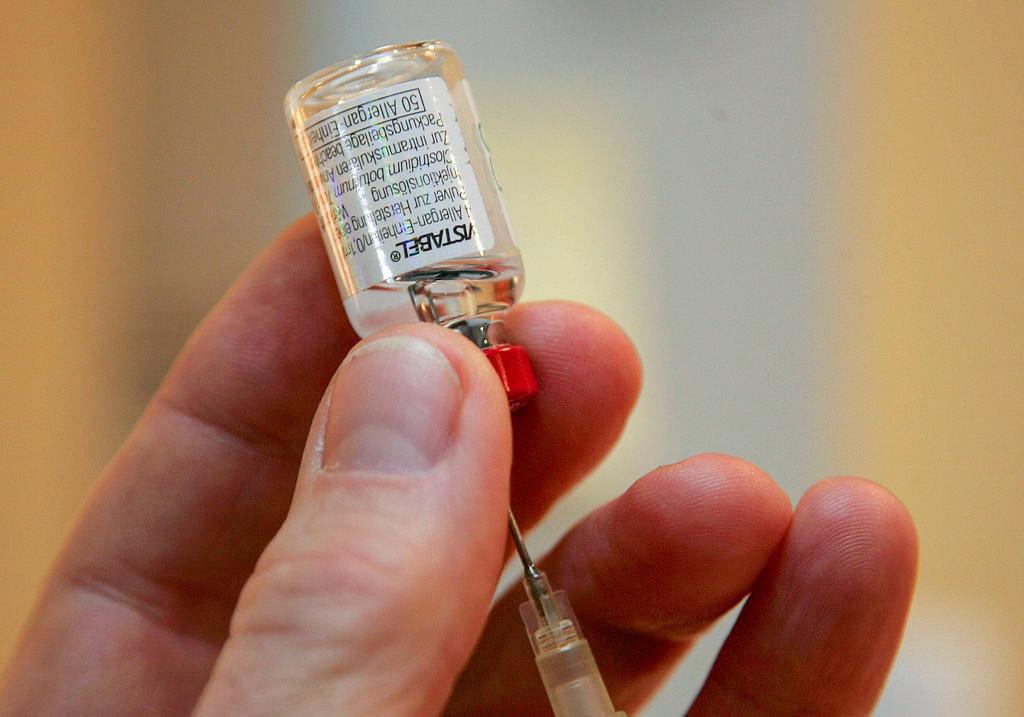
Current medical understanding acknowledges the absence of a specific treatment or cure for EBV, as per the CDC. Although no vaccine is yet available, the National Institutes of Health began a clinical trial for an EBV vaccine in 2022.
This lack of a targeted cure has led to diverse treatment approaches. Health care providers often use antiviral treatments like acyclovir, but these have shown limited effectiveness against EBV’s latent presence in cells.
Catherine Bollard, M.D., and Jeffrey Cohen, M.D., note in a paper, “Once EBV infection is established, acyclovir has no effect on virus-infected T cells in T-cell CAEBV.” Echoing this, Mr. Galyardt adds, “There’s no great antiviral. COVID proved that,” highlighting the limitations of current treatments.
Other treatments like interferons and immunoglobulin therapy have shown inconsistent results, and while immune cell therapy is promising in post-transplant EBV cases, stem cell transplants have had varied success. This underlines the ongoing challenge of finding effective EBV treatments.
Mr. Galyardt advocates a proactive health approach, emphasizing the importance of strengthening the body’s defenses against viruses like EBV. “The vast majority of people carry some form of chronic viral load, but it’s not inevitable for it to become problematic,” he says. His recommendations for keeping EBV inactive include adequate sleep, adrenal function maintenance, and blood sugar level stabilization.
“Chronic viral infections like EBV significantly impact the body,” Mr. Galyardt notes, stressing the importance of overall health. “Keeping our body systems in optimal condition will help prevent and treat chronic viral loads better than any medication out there.”
Dr. Bauerschmidt takes a similar approach, focusing on the roots of immune dysfunction. He promotes oxygen therapy: “Oxygen is essential to eliminate the body’s toxin burden.” He compares traditional treatments like antibiotics and antivirals to using premium fuel without improving the engine—more expensive but not more effective.
At Deeper Healing, Dr. Bauerschmidt uses altitude contrast oxygen therapy, hyperbaric methods, and nighttime oxygen concentrators. He finds a combination of ozone therapy and ultraviolet blood radiation especially effective. For active viral infections, he has found nebulizing with high-quality colloidal silver or 0.3 percent hydrogen peroxide beneficial for some patients.
As research into EBV and the immune system progresses, it holds the promise of new management and treatment strategies for the virus’s associated conditions.
For individuals like Ms. Francis, this research offers hope and the promise of a more proactive approach to managing their health. As the medical community gains a deeper understanding of EBV’s interactions with the immune system, the potential for more targeted and effective treatments grows, bringing hope to millions affected by this pervasive virus.