Study in mice finds a trigger for devastating condition, hints at possible treatment

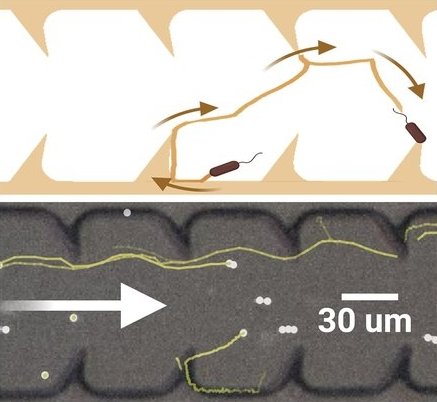
Micrograph of Escherichia coli (E. coli) bacteria.
At a glance:
- Remnant viral genes from ancestral viral infections linked to severity of bacterial infections and formation of abscesses in mice.
- Antiviral drugs used to fight HIV were shown to prevent these dangerous complications of infection in lab experiments.
- Insights into the mechanisms that lead to abscess formation open the door for new lines of thought about treating bacterial infections.
Bacterial infections inside the body can lead to abscesses — pockets of dead cells and debris surrounded by inflammation-fueling immune cells. In these pockets, bacteria multiply, causing more inflammation and further damage to surrounding tissues.
For reasons that remain poorly understood, in some cases the immune reaction can spread throughout the body, resulting in organ damage and life-threatening organ failure, a condition known as sepsis, estimated to affect 1.7 million people in the U.S. each year.
But how do the initial abscesses that set off this devastating immune cascade begin? And why do some escalate to sepsis?
Research published Jan. 16 in PNAS sheds new light on this question and also hints at a possible treatment.
Using animal models, Harvard Medical School investigators at Brigham and Women’s Hospital have identified one key mechanism that may be driving abcess formation in the liver that could culminate in sepsis.
The researchers caution that sepsis could be the result of multiple factors and that other mechanisms could be at play. However, they say their findings pinpoint a previously unknown trigger that could have important implications for treatment.
“Our work to understand the mechanisms of abscess formation and sepsis points to a new way of thinking about treatment and prevention of deleterious consequences following bloodstream infection,” said first author Karthik Hullahalli, an HMS graduate student in microbiology working in the lab of Matthew Waldor at Brigham and Women’s. Waldor is the HMS Edward H. Kass Professor of Medicine at Brigham and Women’s and an affiliated faculty member of the HMS Department of Microbiology.
The researchers say that if replicated in further studies, both in larger animals and then in humans, the work could pave the way to using existing drugs in a novel way to prevent some of the most devastating complications of bacterial infections.
The surprising role of dormant viral genes in igniting bacterial infections
The researchers examined the livers of mice infected with Escherichia coli, or E. coli, a common bacterium that infects many animals, including humans.
They found that abscess formation was linked to the presence and reactivation of dormant endogenous retroviruses (ERVs), genetic remnants of viruses that integrated into the genome of the mice following infections in previous generations.
The authors hypothesized that genetic material produced by the reawakened viruses stimulate inflammatory immune responses that in turn damage surrounding cells and thus drive abscess development. If so, the researchers surmised, suppressing the activity of the ERVs might prevent abscesses from forming.
A possible new use for antiviral drugs
To test this hypothesis, the researchers treated mice with a cocktail of reverse transcriptase inhibitors — antiretroviral drugs used to curb viral replication in people infected with HIV. They found that a single dose of the antiviral medication was enough to prevent abscess formation if delivered quickly after bacterial infection.
“Our findings show that drugs used to treat HIV can be used to prevent inflammatory complications of bacterial sepsis in animals,” Waldor said.
Further work is needed to understand whether and how antiretroviral drugs might prevent complications such as bacterial sepsis in different cases, the researchers said.
For example, Hullahalli noted that in mice, abscess susceptibility varies by sex and among tissues. In addition, the researchers noted that ERVs play a complex role in the life cycle of their host.
ERVs are switched on and off at different points in the course of an animal’s life. Most ERVs are usually deactivated and go into dormancy. In fact, if ERVs aren’t successfully silenced by the host immune system, they could lead to mutations that cause cancer or to immune dysregulation that causes autoimmune diseases later on. But these ERV genes are not always harmful. In some circumstances, ERVs could play a protective role in fighting infections by stimulating defensive immune responses.
“Whether these elements of the genome are beneficial or detrimental to an individual likely depends on context,” Hullahalli noted. “But the findings of this study suggest that there may be a role for the drugs that we currently think of as antivirals in treating inflammatory responses to bacterial infection.”