Last year alone, more than 600,000 people in the United States died from cancer, according to the American Cancer Society. The relentless pursuit of understanding this complex disease has shaped medical progress in developing treatment procedures that are less invasive while still highly effective.
Immunotherapy is on the rise as a possible solution. Immunotherapy involves harnessing the power of the body’s immune system to fight against cancer cells. Researchers in the College of Engineering have found a way to revamp a treatment procedure into a groundbreaking practice.
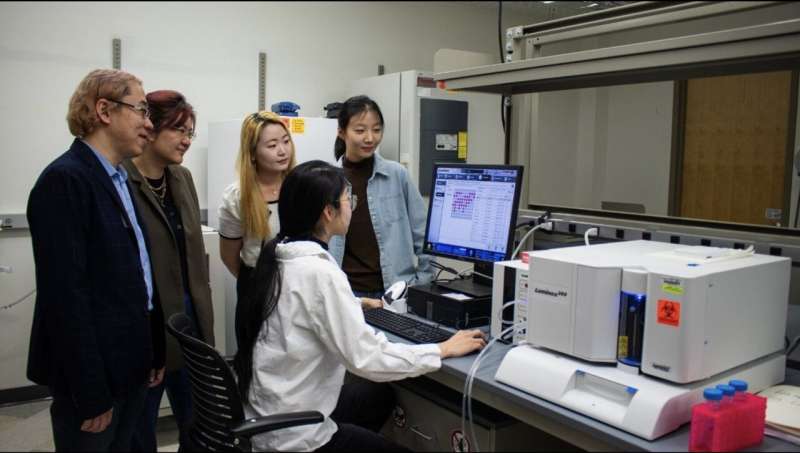
Rong Tong, associate professor in chemical engineering, has teamed up with Wenjun “Rebecca” Cai, associate professor in materials science and engineering, to explore a cancer immunotherapy treatment that has long been of interest to researchers.
In their newly published article in the journal Science Advances, Tong and Cai detailed their approach, which involves activating the immune cells in the body and reprogramming them to attack and destroy the cancer cells. This therapeutic method is frequently implemented with the protein cytokine. Cytokines are small protein molecules that act as intercellular biochemical messengers and are released by the body’s immune cells to coordinate their response.
“Cytokines are potent and highly effective at stimulating the immune cells to eliminate cancer cells,” Tong said. “The problem is they’re so potent that if they roam freely throughout the body, they’ll activate every immune cell they encounter, which can cause an overactive immune response and potentially fatal side effects.”
Tong and Cai, in collaboration with chemical engineering and materials science and engineering graduate students, have developed an innovative approach to employ cytokine proteins as a potential immunotherapy treatment. Unlike previous methods, their technique ensures that the immune cell stimulating cytokines effectively localize within the tumors for weeks while preserving the cytokine’s structure and reactivity levels.
Combining forces to take down cancer cells
Current cancer treatments, such as chemotherapy, cannot distinguish between healthy cells and cancer cells. When someone with cancer is treated with chemotherapy, the treatment attacks all of the cells in their body, which can lead to side effects such as hair loss and fatigue.
Stimulating the body’s immune system to attack tumors is a promising alternative to treat cancer. The delivery of cytokines can jump-start immune cells in the tumor, but overstimulating healthy cells can cause severe side effects.
“Scientists determined a while ago that cytokines can be used to activate and fight against tumors, but they didn’t know how to localize them inside the tumor while not exposing toxicity to the rest of the body,” said Tong. “Chemical engineers can look at this from an engineering approach and use their knowledge to help refine and elevate the effectiveness of the cytokines so they can work inside the body effectively.”
The research team’s goal is to find a balance between killing cancer cells in the body while sparing healthy cells.
To accomplish this goal, Tong and his students used their expertise to create specialized particles with distinctive sizes that help determine where the drug is going. These microparticles are designed to stay within the tumor environment after being injected into the body. Cai and her students worked on measuring these particles’ surface properties.
“In the field of materials science and engineering, we study the surface chemistry and mechanical behavior of materials, such as the specialized particle created for this project,” Cai said. “Surface engineering and characterization, along with particle size, play important roles in controlled drug delivery, ensuring prolonged drug presence and sustained therapeutic effectiveness.”
To ensure successful drug delivery, Tong and his chemical engineering students designed a novel strategy that:
- Anchors cytokines to these new microparticles, limiting the harm of cytokines to healthy cells
- Allows the newly particle-anchored cytokines to jump-start immune systems and recruit immune cells to attack cancer cells
“Our strategy not only minimizes cytokine-induced harm to healthy cells, but also prolongs cytokine retention within the tumor,” Tong said. “This helps facilitate the recruitment of immune cells for targeted tumor attack.”
The next step in the process involves combining the new, localized cytokine therapy method with commercially available, Food and Drug Administration (FDA)-approved checkpoint blockade antibodies, which reactivate the tumor immune cells that have been silenced so they can fight back the cancer cells.
“When there is a tumor inside the body, the body’s immune cells are being deactivated by the cancer cells,” Tong explained. “The FDA-approved checkpoint blocking antibody helps ‘take off the brakes’ that tumors put on immune cells, while the cytokine molecules ‘step on the gas’ to jump-start the immune system and get an immune cell army to fight cancer cells. These two approaches work together to activate immune cells.”
Combining the checkpoint antibodies with the particle-anchored cytokine proved to successfully eliminate many tumors in their study.
Engineering an impact on cancer treatment
Team members hope their impact on immunotherapy treatment is part of a greater movement toward cancer treatment approaches that are harmless to healthy cells. The new approach of attaching cytokines to particles also could be used in the future to deliver other types of immunostimulatory drugs, according to the team.
“Researchers are still looking for safer and more effective cancer treatments,” said Tong. “This motivation is what drives us to develop new technologies in the field. The whole class of drugs that are employed to jump-start the immune system to fight cancer cells has largely not yet succeeded.
“Our goal is to create novel solutions that allow researchers to test these drugs with existing FDA-approved therapeutics, ensuring both safety and enhanced efficacy.”
Cai said the nature of cancer treatment research requires expertise across engineering disciplines.
“I view this project as a perfect marriage between chemical engineering and materials science,” Cai said. “The former focuses on the synthesis and drug delivery part, the latter on applying advanced materials characterization. This collaboration not only accelerates immunotherapy research, but also has the ability to transform cancer treatment.”