Summary: A newly developed blood test can detect brain-derived tau (BD-tau), a biomarker of Alzheimer’s disease neurodegeneration.
A group of neuroscientists led by a University of Pittsburgh School of Medicine researcher developed a test to detect a novel marker of Alzheimer’s disease neurodegeneration in a blood sample.
A study on their results was published today in Brain.
The biomarker, called “brain-derived tau,” or BD-tau, outperforms current blood diagnostic tests used to detect Alzheimer’s-related neurodegeneration clinically. It is specific to Alzheimer’s disease and correlates well with Alzheimer’s neurodegeneration biomarkers in the cerebrospinal fluid (CSF).
“At present, diagnosing Alzheimer’s disease requires neuroimaging,” said senior author Thomas Karikari, Ph.D., assistant professor of psychiatry at Pitt. “Those tests are expensive and take a long time to schedule, and a lot of patients, even in the U.S., don’t have access to MRI and PET scanners. Accessibility is a major issue.”
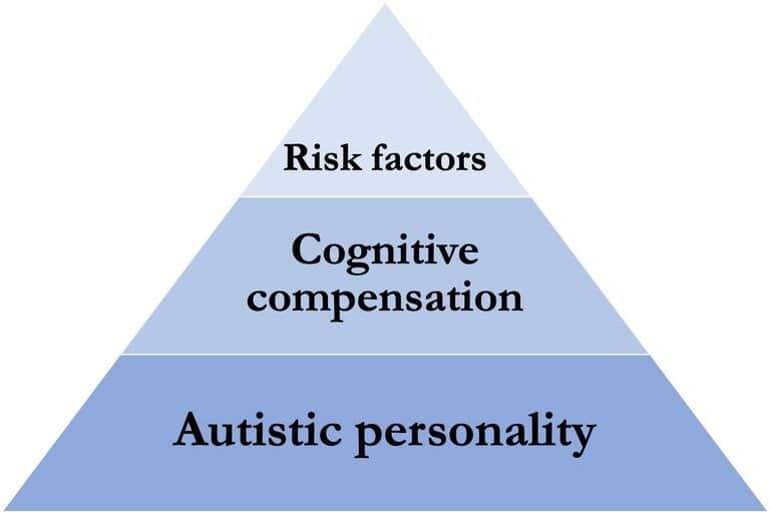
Currently, to diagnose Alzheimer’s disease, clinicians use guidelines set in 2011 by the National Institute on Aging and the Alzheimer’s Association. The guidelines, called the AT(N) Framework, require detection of three distinct components of Alzheimer’s pathology—the presence of amyloid plaques, tau tangles and neurodegeneration in the brain—either by imaging or by analyzing CSF samples.
Unfortunately, both approaches suffer from economical and practical limitations, dictating the need for development of convenient and reliable AT(N) biomarkers in blood samples, collection of which is minimally invasive and requires fewer resources.
The development of simple tools detecting signs of Alzheimer’s in the blood without compromising on quality is an important step toward improved accessibility, said Karikari.
“The most important utility of blood biomarkers is to make people’s lives better and to improve clinical confidence and risk prediction in Alzheimer’s disease diagnosis,” Karikari said.
Current blood diagnostic methods can accurately detect abnormalities in plasma amyloid beta and the phosphorylated form of tau, hitting two of the three necessary checkmarks to confidently diagnose Alzheimer’s.
But the biggest hurdle in applying the AT(N) Framework to blood samples lies in the difficulty of detecting markers of neurodegeneration that are specific to the brain and aren’t influenced by potentially misleading contaminants produced elsewhere in the body.
For example, blood levels of neurofilament light, a protein marker of nerve cell damage, become elevated in Alzheimer’s disease, Parkinson’s and other dementias, rendering it less useful when trying to differentiate Alzheimer’s disease from other neurodegenerative conditions. On the other hand, detecting total tau in the blood proved to be less informative than monitoring its levels in CSF.
By applying their knowledge of molecular biology and biochemistry of tau proteins in different tissues, such as the brain, Karikari and his team, including scientists at the University of Gothenburg, Sweden, developed a technique to selectively detect BD-tau while avoiding free-floating “big tau” proteins produced by cells outside the brain.
To do that, they designed a special antibody that selectively binds to BD-tau, making it easily detectible in the blood. They validated their assay across over 600 patient samples from five independent cohorts, including those from patients whose Alzheimer’s disease diagnosis was confirmed after their deaths, as well as from patients with memory deficiencies indicative of early-stage Alzheimer’s.
The tests showed that levels of BD-tau detected in blood samples of Alzheimer’s disease patients using the new assay matched with levels of tau in the CSF and reliably distinguished Alzheimer’s from other neurodegenerative diseases. Levels of BD-tau also correlated with the severity of amyloid plaques and tau tangles in the brain tissue confirmed via brain autopsy analyses.
Scientists hope that monitoring blood levels of BD-tau could improve clinical trial design and facilitate screening and enrollment of patients from populations that historically haven’t been included in research cohorts.

“There is a huge need for diversity in clinical research, not just by skin color but also by socioeconomic background,” said Karikari.
“To develop better drugs, trials need to enroll people from varied backgrounds and not just those who live close to academic medical centers. A blood test is cheaper, safer and easier to administer, and it can improve clinical confidence in diagnosing Alzheimer’s and selecting participants for clinical trial and disease monitoring.”
Karikari and his team are planning to conduct large-scale clinical validation of blood BD-tau in a wide range of research groups, including those that recruit participants from diverse racial and ethnic backgrounds, from memory clinics, and from the community. Additionally, these studies will include older adults with no biological evidence of Alzheimer’s disease as well as those at different stages of the disease.
These projects are crucial to ensure that the biomarker results are generalizable to people from all backgrounds, and will pave the way to making BD-tau commercially available for widespread clinical and prognostic use.