Day: 01/02/2023
Even Leaner People with Type 2 Diabetes Can Achieve Remission

A new study has demonstrated that weight loss can lead to remission from type 2 diabetes even for people that are not overweight.
We already know that some people with type 2 diabetes can achieve remission, but most research suggests that it generally requires dramatic weight loss. So where does that leave patients with type 2 diabetes that have less weight to lose?
Contrary to the stereotypes, sometimes even lean adults develop type 2 diabetes. According to the CDC’s National Diabetes Statistics Report (PDF), about 11% of the United States’ estimated 34 million adults with diabetes have a BMI under 25 kg/m2, indicating “normal” weight. (An additional 27.6% are classed as “overweight,” but not obese.)
The ReTUNE trial, out of the UK’s Newcastle University, suggests that even comparatively lean patients with diabetes can put their conditions into remission. And the method is the just same: cutting calories and losing weight.
The trial enrolled adults with type 2 diabetes that had a BMI near 25 kg/m2, the official border between “normal” and “overweight.” Participants were asked to follow a strict 800-calorie per day diet consisting of “formula meal replacements and non-starchy vegetables.” They would alternate between 2-4 weeks of the crash diet and 4-6 weeks of a weight-loss maintenance diet, repeating the cycle up to three times.
In results shared at the recent 2022 Diabetes UK Professional Conference , an incredible 70% of ReTUNE participants were said to achieve remission. These lucky patients lost an average of 8% of their bodyweight, and enjoyed significant improvements to their A1C despite ceasing the use of glucose-lowering medications.
The results are impressive, but a few warnings are in order:
- The study was extremely small (only 20 participants).
- All participants had been diagnosed with type 2 in the previous five years. There’s reason to doubt that intervention would be as effective for people with long-standing diabetes.
- We don’t know what will happen to these participants in the future. Most experts believe that losing weight in the first place is actually the easy part. Maintaining weight loss is the real struggle. Does a crash diet set patients up for sustainable success?
This isn’t the first time the same research team has shown that very low-calorie diets can make a big difference. Dr. Roy Taylor also led the DIRECT trial, which placed adults with type 2 diabetes on a very low-calorie diet for 3-5 months and then offered significant weight management training and support for up to two years. An impressive 36% of those participants achieved diabetes remission by the end of the second year. Among those that lost at least 10kg (about 22 lbs.), a majority (64%) achieved remission.
Dr. Taylor’s unifying theory of diabetes is the personal fat threshold, which argues that every individual has a unique level of excess fat accumulation that they can handle. Some people may develop type 2 diabetes after gaining only a little weight, while others can sustain extreme obesity without ever becoming diabetic. As Dr. Taylor told the Guardian, “The bottom line is, a person will develop type 2 diabetes when they’ve become too heavy for their own body. It doesn’t matter if their BMI is within the ‘normal’ range. They’ve crossed their personal threshold and become unhealthy.”
Although leaner people with diabetes have less weight to lose, the theory goes, they have just as much to gain from losing it.
Dr. Taylor is eager to spread the word. On his university webpage, you can find links to his books and Youtube talks, and even a list of approved meal-replacement shakes. Last year the Guardian published a profile of Dr. Taylor and his methods, another resource for curious readers.
Other trials unrelated to Dr. Taylor’s research have similarly shown that very low-calorie diets can be effective in reversing the progression of type 2 diabetes. But those should perhaps be weighed against the fact that most dieting authorities caution against crash diets, believing that they do not prepare dieters for the type of sustainable healthy adjustments that they’ll need to maintain weight loss for years into the future.
It should go without saying that anyone contemplating an extreme diet should speak to their doctor first.
SGLT-2 Inhibitors

SGLT-2 inhibitors are a class of diabetes drugs used to treat type 2 diabetes and, often off-label, type 1 diabetes. These drugs work by preventing your body from re-absorbing sugar into your bloodstream and instead flush it out when you urinate. SGLT-2 medications are taken orally, typically daily.
This drug has an interesting history. The compound was first discovered in the 1800s when someone noticed that if dogs urinate at the bark of a certain tree, ants would be attracted to that dog’s urine. The dog’s urine was sweet. One and a half centuries later, we have a new diabetes treatment!
Sodium-glucose co-transporter 2 (SGLT2) inhibitors are a relatively new class of prescription drugs which are FDA approved for type 2 diabetes to use in combination with diet and exercise to help lower blood sugar levels.
Medications in this class include:
- canagliflozin (Invokana)
- dapagliflozin (Farxiga)
- empagliflozin (Jardiance)
These are available as single-ingredient drugs or in combination with other diabetes medications. The combinations currently available are:
- canagliflozin and metformin (Invokamet)
- dapagliflozin and metformin extended-release (Xigduo XR)
- empagliflozin and linagliptin (Glyxambi)
How do SGLT2 Inhibitors Work?
SGLT2 is a protein humans have which helps glucose reabsorb in the kidneys. The SGLT2 protein is responsible for 90% of the glucose reabsorption in the proximal renal tube.
An SGLT2 inhibitor stops the reabsorption of glucose in the kidneys and the extra sugar is excreted into the urine. This helps to lower blood sugar levels. Below is a graphic that shows an SGLT2 inhibitor does this:

Side Effects of SGLT2 Inhibitors
The FDA states that “The safety and efficacy of SGLT2 inhibitors have not been established in patients with type 1 diabetes, and FDA has not approved them for use in these patients.” Studies have been indicating patients with type 1 diabetes may be able to use SGLT2 inhibitors safely, however.
Side effects of SGLT2 inhibitors, as reported by the FDA include:
- acidosis
- dehydration
- kidney problems
- low blood sugar when combined with other diabetes medications
- elevated blood cholesterol
- yeast infections in men and women
Warnings from the FDA
The FDA has issued a strengthened warning for canagliflozin (Invokana, Invokamet) and dapagliflozin (Farxiga, Xigduo XR). The warning is for acute kidney injury and they add the following recommendations to help lower this risk:
“Patients should seek medical attention immediately if they experience signs and symptoms of acute kidney injury. This is a serious condition in which the kidneys suddenly stop working, causing dangerous levels of wastes to build up in the body. Signs and symptoms of acute kidney injury may include decreased urine or swelling in the legs or feet. Patients should not stop taking their medicine without first talking to their health care professionals. Doing so can lead to uncontrolled blood sugar levels that can be harmful.”
The FDA has also issued a warning for any SGTL2 inhibitor stating it may lead to diabetic ketoacidosis (DKA).
It is especially helpful when taking a medication to keep a journal of when you take something and how much you took. Include your symptoms and blood sugar readings in order to be able to help you and your healthcare provider decide whether or not a medication is working safely for you.
If you live in the USA and have experienced a serious side effect, you or your doctor may send a report to the FDA’s MedWatch Adverse Event Reporting program online (http://www.fda.gov/Safety/MedWatch) or by phone (1-800-332-1088).
SLGT-2 Inhibitors for Type 1 Diabetes
diaTribe shares the following advice from Dr. Anne Peters, who helped author the study that led to the warning on SGLT-2 inhibitors.
In individuals with type 1 diabetes who are using the drug off-label, it is best to work out a plan for safe use of the medication with a health care provider. Dr. Peters has patients temporarily hold the drug if unusual activity will be occurring during the day (e.g., travel, increased exercise, or a person feels unwell). Her patients with type 1 diabetes test ketones a week or two before starting the SGLT-2 inhibitor to obtain a baseline ketone level, then test urine ketones every morning while on the drug. If ketone levels are moderate to large, Dr. Peters recommends stopping use of the drug that day until the ketones clear. Finally, her patients with type 1 or type 2 diabetes stop the drug for three days before any elective surgery.
glycemic diabetic ketoacidosis.”
The Effect of Oral Antidiabetic Agents on A1C Levels: A systematic review and meta-analysis
OBJECTIVE
Previous reviews of the effect of oral antidiabetic (OAD) agents on A1C levels summarized studies with varying designs and methodological approaches. Using predetermined methodological criteria, we evaluated the effect of OAD agents on A1C levels.
RESEARCH DESIGN AND METHODS
The Excerpta Medica (EMBASE), the Medical Literature Analysis and Retrieval System Online (MEDLINE), and the Cochrane Central Register of Controlled Trials databases were searched from 1980 through May 2008. Reference lists from systematic reviews, meta-analyses, and clinical practice guidelines were also reviewed. Two evaluators independently selected and reviewed eligible studies.
RESULTS
A total of 61 trials reporting 103 comparisons met the selection criteria, which included 26,367 study participants, 15,760 randomized to an intervention drug(s), and 10,607 randomized to placebo. Most OAD agents lowered A1C levels by 0.5−1.25%, whereas thiazolidinediones and sulfonylureas lowered A1C levels by ∼1.0–1.25%. By meta-regression, a 1% higher baseline A1C level predicted a 0.5 (95% CI 0.1–0.9) greater reduction in A1C levels after 6 months of OAD agent therapy. No clear effect of diabetes duration on the change in A1C with therapy was noted.
CONCLUSIONS
The benefit of initiating an OAD agent is most apparent within the first 4 to 6 months, with A1C levels unlikely to fall more than 1.5% on average. Pretreated A1C levels have a modest effect on the fall of A1C levels in response to treatment.
CONCLUSIONS
This systematic review and meta-analysis of double-blind, randomized controlled trials that met predefined methodological criteria summarized treatment effects on A1C levels across OAD drug class, dose, and duration of therapy (Fig. 2). The greatest pooled treatment effect noted was with maximum doses of sulfonylureas after 12 weeks of therapy, followed by TZDs after 13–18 weeks of therapy. Across all OAD classes, an increase in dose yielded a further decrease in A1C initially with a maximum effect achieved by 3–6 months.
The meta-regression analysis also provided a numerical estimate of an effect that has been commented on by previous authors: higher baseline A1C levels are associated with greater declines in A1C with therapy (9). However, this effect was modest in most studies that were reviewed, such that after controlling for OAD drug class and dose, every 1% higher pretreatment A1C levels predicted a 0.5% greater fall of A1C levels after 6 months of therapy.
This review has several strengths. First, it was restricted to randomized controlled trials that met predetermined methodological criteria to minimize the potential for bias. Of note, the application of these criteria led to the exclusion of 150 out of 211 (71%) manuscripts that may otherwise have been included. Second, it entailed a comprehensive search for all currently used OAD classes for type 2 diabetes treatment. Third, the effect of OADs on A1C level was assessed at different time intervals, ranging from 12 weeks to 2 years. Finally, it focused on the effect of OAD class versus individual drugs and therefore may be relevant to new drugs from the same class.
This review has several limitations. First, most of the studies included participants with relatively newly diagnosed diabetes (median duration of diabetes of 5.2 years). As such, the review’s findings may not be relevant to patients with a longer duration of diabetes or with diabetes-related complications. Second, relatively few studies were available for sulfonylureas (n = 6), meglitinides (n = 10), and biguanides (n = 12) thereby affecting the reliability of their respective quantitative estimates. Third, less than 30% of the reviewed papers reported the effect of therapy for periods greater than 24 weeks. Fourth, there is some statistical heterogeneity (ranging up to 90%) in the meta-analyzed results of the included studies, regardless of OAD class, drug, or dose. This heterogeneity may have been due to study differences in design, patient demographics and characteristics, duration of diabetes, and background drug therapy or confounding. Regardless of the cause, heterogeneity was managed by using a random-effects model for meta-analyses. Fifth, some of the summarized trials added oral agents to background therapy that included insulin. If investigators adjusted the dose of insulin during the trial, this may have affected the estimate of the effect of the OAD on the change in A1C. This could not be taken into consideration as insulin doses were not provided in the reports. Finally, it is possible that this review was influenced by publication bias given that studies with positive results are generally more likely to get published, resulting in an overestimate of the benefit of an OAD on A1C reduction.
In summary, the results of this systematic review and meta-analysis suggest that the initiation of an OAD in addition to current therapy yields an additional decrease in A1C level of ∼1–1.25% with most of the treatment effect evident by 3–6 months of initiating OAD therapy. This effect was fairly consistent between OAD classes with sulfonylureas and TZDs having the greatest reduction in AIC. The meta-regression analysis numerically demonstrated a small effect of baseline A1C on the fall of A1C with OAD treatment. Further carefully conducted OAD trials are needed to account for 1) combinations of OAD drug use and its impact on A1C levels; 2) the effectiveness of long-term OAD use on A1C levels; and 3) adverse and hypoglycemic events.
Source: https://diabetesjournals.org
Human brain cells implanted in rats prompt excitement — and concern
Rat–human hybrid brains offer new ways to study human neurological disorders, but also raise ethical questions
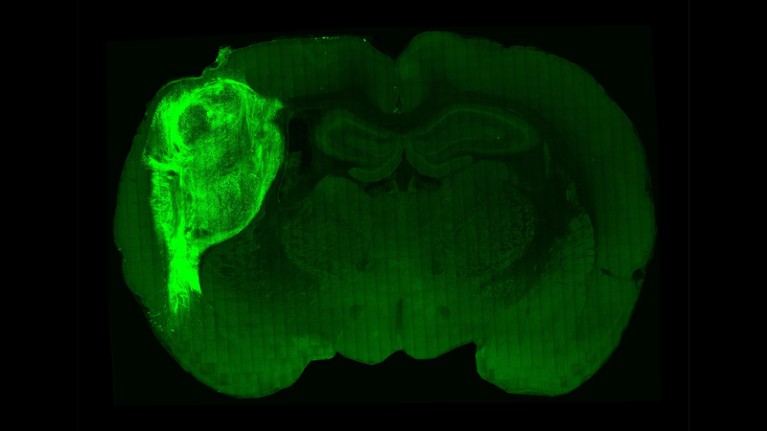
Miniature human-brain-like structures transplanted into rats can send signals and respond to environmental cues picked up by the rats’ whiskers, according to a study1. This demonstration that neurons grown from human stem cells can interface with nerve cells in live rodents could lead to a way to test therapies for human brain disorders.Hybrid brains: the ethics of transplanting human neurons into animals
Scientists would like to use brain organoids — tiny brain-like structures grown from human stem cells — to study neurodegenerative and neuropsychiatric disorders that humans develop. But the organoids mimic human brains only so far. They don’t develop blood vessels and so can’t receive nutrients, meaning that they don’t thrive for long. And they don’t get the stimulation they need to grow fully: in a human infant’s brain, neurons’ growth and how they develop connections with other neurons are based in part on input from the senses.
To give brain organoids this stimulation and support, neuroscientist Sergiu Pasca at Stanford University in California and his colleagues grew the structures from human stem cells and then injected them into the brains of newborn rat pups, with the expectation that the human cells would grow along with the rats’ own cells. The team placed the organoids in a brain region called the somatosensory cortex, which receives signals from the rats’ whiskers and other sensory organs and then passes them along to other brain regions that interpret the signals.Can lab-grown brains become conscious?
Human brain cells mature much more slowly than rat cells, so the researchers had to wait for more than six months for the organoids to become fully integrated into the rat brains. But when they examined the animals’ brains at the end of that time, they saw that the integration had been so successful that it was almost like adding “another transistor to a circuit”, Pasca said at a 10 October press conference.
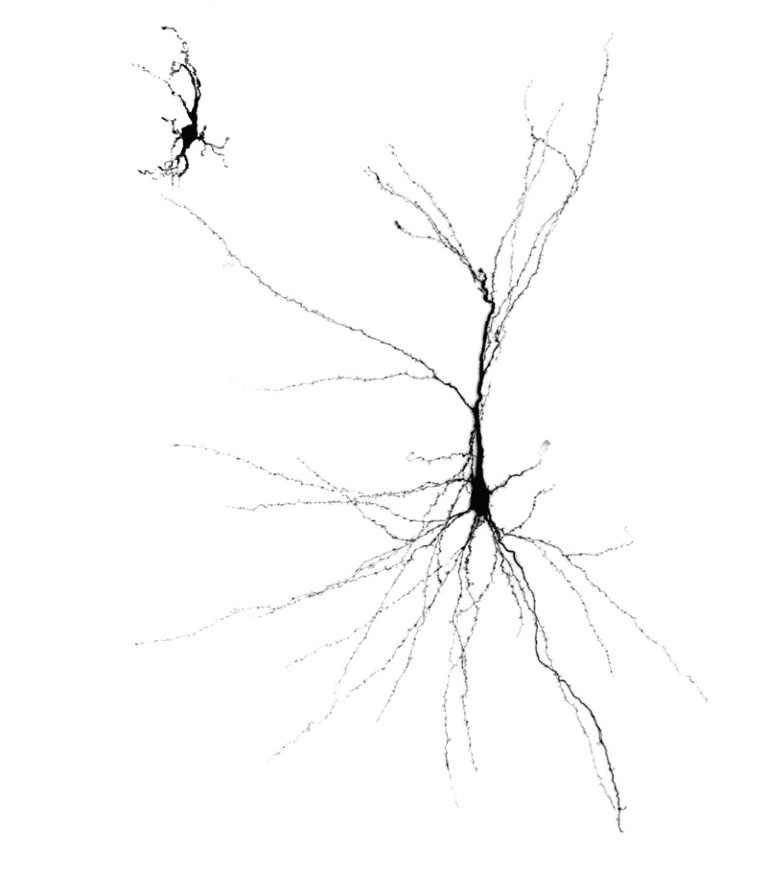
Paola Arlotta, a molecular biologist at Harvard University in Cambridge, Massachusetts, is excited about the results. “It’s an important step in allowing organoids to tell us more complex properties of the brain,” she says, although she thinks that the transplantation procedure is probably still too expensive and complex to become a standard research tool. The next step, Arlotta adds, will be to work out how individual human neurons — not just fully developed organoids — are integrated into the rat brain.
Behaviour trigger
In their report, published in Nature on 12 October1, the researchers describe how they genetically engineered the neurons in the organoids to fire when stimulated with light from a fibre-optic cable embedded in the rats’ brains. The team trained the rats to lick a spout to receive water while the light was switched on. Afterwards, when the researchers shone the light on the hybrid brains, the rats were prompted to lick the spout, meaning that the human cells had become integrated well enough to help drive the animals’ behaviour. Furthermore, when the researchers prodded the rats’ whiskers, they found that the human cells in the sensory cortex fired in response, suggesting that the cells were able to pick up sensory information.
To demonstrate the promise of their work for studying brain disorders, Pasca and his colleagues also created brain organoids from the stem cells of three people with a genetic condition called Timothy syndrome, which can cause symptoms similar to some seen in autism. The tiny structures looked the same as any other brain organoids grown in a dish, but when the researchers transplanted them into rats, they did not grow as large as others and their neurons didn’t fire in the same way.
Rusty Gage, a neuroscientist at the Salk Institute for Biological Studies in La Jolla, California, is glad to see these results. In 2018, he and a team of researchers found that transplanted human brain organoids could be integrated into the brains of adult mice2. Mice don’t live as long as rats, and Pasca and his colleagues hoped that because newborn rat pups’ brains are more plastic than those of adult animals, they would be better able to receive the new cells.
“We’ve got challenges out there for us,” Gage says. “But I do believe the transplantation procedure will be a valuable tool.”First monkey–human embryos reignite debate over hybrid animals
Some of the challenges are ethical. People are concerned that creating rodent–human hybrids could harm the animals, or create animals with human-like brains. Last year, a panel organized by the US National Academies of Sciences, Engineering, and Medicine released a report concluding that human brain organoids are still too primitive to become conscious, attain human-like intelligence or acquire other abilities that might require legal regulation. Pasca says that his team’s organoid transplants didn’t cause problems such as seizures or memory deficits in the rats, and didn’t seem to change the animals’ behaviour significantly.
But Arlotta, a member of the National Academies panel, says that problems could arise as science advances. “We can’t just discuss it once and let it be,” she says. She adds that concerns about human organoids need to be weighed against the needs of people with neurological and psychiatric disorders. Brain organoids and human–animal hybrid brains could reveal the mechanisms underlying these illnesses, and allow researchers to test therapies for conditions such as schizophrenia and bipolar disorder. “I think we have a responsibility as a society to do everything we can,” Arlotta says.
Source: Nature
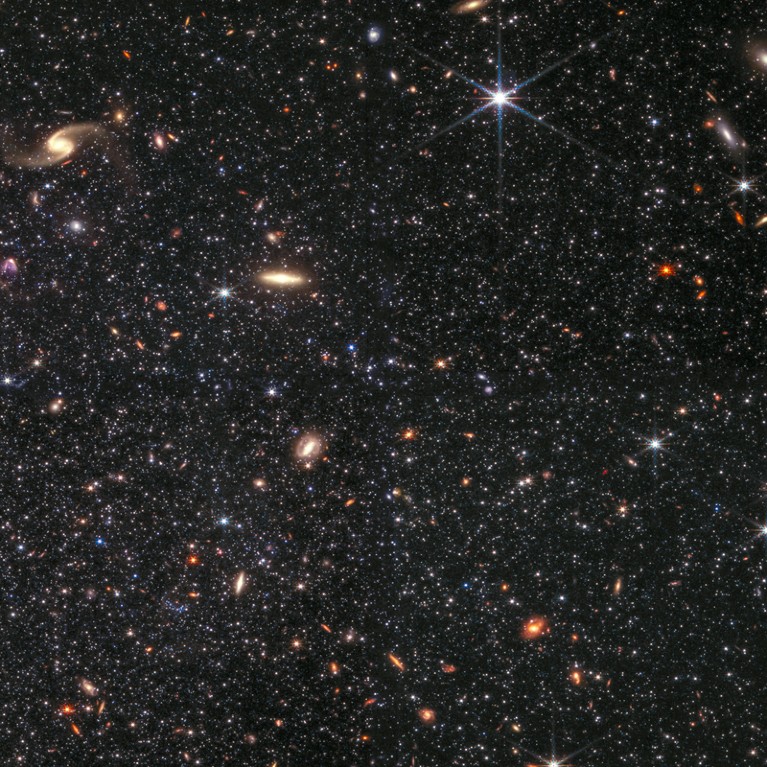
How JWST revolutionized astronomy in 2022
The far-seeing observatory has served up revelations from the most distant reaches of the Universe to a moon orbiting Saturn.
The crowd in the auditorium began murmuring, then gasping, as Emma Curtis-Lake put her slides up on the screen. “Amazing!” someone blurted out.
Curtis-Lake, an astronomer at the University of Hertfordshire in Hatfield, UK, was showing off some of the first results on distant galaxies from NASA’s James Webb Space Telescope (JWST). It was not the last time astronomers started chattering in excitement this week as they gazed at the telescope’s initial discoveries, at a symposium held at the Space Telescope Science Institute (STScI) in Baltimore, Maryland.
In just its first few months of science operations, JWST has delivered stunning insights on heavenly bodies ranging from planets in the Solar System to stars elsewhere in the cosmos. These discoveries have sharpened researchers’ eagerness to take more advantage of the observatory’s capabilities. Scientists are now crafting new proposals for what the telescope should do in its second year, even as they scramble for funding and debate whether the telescope’s data should be fully open-access.
White-knuckle launch
JWST launched on 25 December 2021 as the most expensive, most delayed and most complicated space observatory ever built. Astronomers held their breath as the US$10-billion machine went through a complex six-month engineering deployment in deep space, during which hundreds of potential failures could have seriously damaged it.
But it works — and spectacularly so. “I feel really lucky to be alive as a scientist to work with this amazing telescope,” says Laura Kreidberg, an astronomer at the Max Planck Institute for Astronomy in Heidelberg, Germany.JWST spots some of the most distant galaxies ever seen
First out of the floodgate, in July, came a rush of preprints on the early evolution of galaxies. The expansion of the Universe has stretched distant galaxies’ light to infrared, the wavelengths that JWST captures. That allows the telescope to observe faraway galaxies — including several so distant that they appear as they did just 350 million to 400 million years after the Big Bang, which happened 13.8 billion years ago.
Many early galaxies spotted by JWST are brighter, more diverse and better formed than astronomers had anticipated. “It seems like the early Universe was a very profound galaxy-maker,” says Steven Finkelstein, an astronomer at the University of Texas at Austin.
Some of these initial findings are being revised as data calibrations improve, and many of the early claims about distant galaxies await confirmation by spectroscopic studies of the galaxies’ light. But astronomers including Curtis-Lake announced on 9 December that they have already nailed spectroscopic confirmation of two galaxies that are farther away than any ever previously confirmed.
’Mindblowing’ detail
In closer regions of the cosmos, JWST is yielding results on star formation and evolution, thanks to its sharp resolution and infrared vision. “Compared to what we can see with Hubble, the amount of details that you see in the Universe, it’s completely mind-blowing,” says Lamiya Mowla, an astronomer at the University of Toronto in Canada. She and her colleagues were able to spot bright ‘sparkles’ around a galaxy that they dubbed the Sparkler; these turned out to be some of the oldest star clusters ever discovered. Other studies have unveiled details such as the hearts of galaxies where monster black holes lurk.
Another burst of JWST discoveries comes from studies of exoplanet atmospheres, which the telescope can scrutinize in unprecedented detail.JWST reveals first evidence of an exoplanet’s surprising chemistry
For instance, when scientists saw the first JWST data from the exoplanet WASP-39b, signals from a range of compounds, such as water, leapt right out. “Just looking at it was like, all the answers were in front of us,” says Mercedes López-Morales, an astronomer at the Center for Astrophysics | Harvard & Smithsonian in Cambridge, Massachusetts. Now scientists are keenly anticipating data about other planets, including the seven Earth-sized worlds that orbit the star TRAPPIST-1. Early results on two of the TRAPPIST-1 planets, reported at the symposium, suggest that JWST is more than capable of finding atmospheres there, although the observations will take more time to analyse.
JWST has even made its first planet discovery: a rocky Earth-sized planet that orbits a nearby cool star, Kevin Stevenson at the Johns Hopkins University Applied Physics Laboratory in Laurel, Maryland, told the meeting.
The telescope has also proved its worth for studying objects in Earth’s celestial neighbourhood. At the symposium, astronomer Geronimo Villanueva at NASA’s Goddard Space Flight Center in Greenbelt, Maryland, showed new images of Saturn’s moon Enceladus. Scientists knew that Enceladus has a buried ocean whose water sometimes squirts out of fractures in its icy crust, but JWST revealed that the water plume envelops the entire moon and spreads well beyond. Separately, engineers have also figured out a way to get JWST to track rapidly moving objects, such as Solar System planets, much better than expected. That led to new studies such as observations of the DART spacecraft’s deliberate crash into an asteroid in September, says Naomi Rowe-Gurney, an astronomer also at Goddard.Fresh images reveal fireworks when NASA spacecraft ploughed into asteroid
Yet all these discoveries are but a taste of what JWST could ultimately do to change astronomy. “It’s premature to really have a full picture of its ultimate impact,” says Klaus Pontoppidan, JWST project scientist at STScI. Researchers have just begun to recognize JWST’s powers, such as its ability to probe details in the spectra of light from astronomical objects.
Applications are now open for astronomers to pitch their ideas for observations during JWST’s second year of operations, which starts in July. The next round could result in more ambitious or creative proposals to use the telescope now that astronomers know what it is capable of, Pontoppidan says.
Amid all the good news, there are still glitches. Primary among them is a lack of funding to support scientists working on JWST data, says López-Morales. “We can do the science, we have the skills, we are developing the tools, we are going to make groundbreaking discoveries but on a very thin budget,” she says. “Which is not ideal right now.”
Available to all?
López-Morales chairs a committee that represents astronomers who use JWST, and their to-do list is long. It includes surveying scientists about whether all of the telescope’s data should be freely available as soon as it is collected — a move that many say would disadvantage early-career scientists and those at smaller institutions who do not have the resources to pounce on and analyse JWST data right away. Telescope operators are also working on a way to get its data to flow more efficiently to Earth through communication dishes, and to fly it in a physical orientation that reduces the risk of micro-meteoroids smashing into and damaging its primary mirror.
But overall, the telescope is opening up completely new realms of astronomy, says Rowe-Gurney: “It’s the thing that’s going to answer all the questions that my PhD was trying to find.”
Source: Nature
Defining the Optimal Duration of Lenalidomide Maintenance after Autologous Stem Cell Transplant – Data from the Myeloma XI Trial
Abstract
Introduction Lenalidomide maintenance after autologous stem cell transplant (ASCT) is standard of care for myeloma (MM) patients, based on trials in which lenalidomide was planned to continue until disease progression. As outcomes for myeloma patients continue to improve, understanding whether time limited maintenance is as effective as treatment to progression is a critical question. Optimal duration may differ in subgroups of patients e.g. those with standard vs high-risk genetics or those who have achieved minimal residual disease negativity (MRD-ve). Data from the UK NCRI Myeloma XI trial were analysed to explore these questions.
Methods Myeloma XI is a phase III randomised controlled trial which recruited newly diagnosed patients with pathways for both transplant eligible (TE) and ineligible patients. In the TE pathway there was a maintenance randomisation at 3 months after ASCT with patients allocated to either lenalidomide maintenance (10mg D1-21/28, planned to continue until disease progression) or observation.
Progression-free survival (PFS) data were analysed landmarked from multiple time points (2, 3, 4, and 5 years) after the time of maintenance randomisation, including all patients who had not had an event or were censored prior to that time point. Data were analysed for all patients, within genetic risk sub-groups and by MRD status. MRD was assessed at the time of maintenance randomisation using flow cytometry with a median sensitivity of 0.004%. Molecular high-risk (HiR) was defined as the presence of del(17p), gain(1q), t(4,14), t(14;16) or t(14;20). The percentage of patients experiencing key side effects over time was also explored including all patients taking lenalidomide in each 6-month time interval.
Results In the TE pathway 1248 patients entered the maintenance randomisation and were allocated to observation (n=518) or lenalidomide (n=730). Median follow up was 44.7 months (IQR 32.4-62.7). As previously reported, lenalidomide maintenance was associated with a significant PFS benefit, median PFS from randomisation was 64 months for those receiving lenalidomide vs 32 months for those observed (HR 0.52, [95%CI 0.45, 0.61], p<0.001). This was consistent for both SR (HR 0.40, [95%CI 0.28, 0.58], p<0.0001) and HiR (HR 0.50, [95%CI 0.35, 0.70], p<0.0001) patients and for those MRD-ve (HR 0.72, [95%CI 0.55, 0.95], p=0.022) and MRD+ve (HR 0.37, [95%CI 0.27, 0.50], p<0.0001) at the start of maintenance therapy.
The magnitude of the PFS benefit was consistent when landmarked from 2y after randomisation (HR 0.51 [95%CI 0.40, 0.66], p<0.001), 3y (HR 0.47, [95%CI 0.33, 0.67], p<0.0001) and 4y (HR 0.56 [95%CI 0.33, 0.95], p=0.031), but the benefit appeared to diminish at subsequent time points.
There was more evidence for the benefit of longer duration of lenalidomide maintenance in patients MRD+ve at the start of maintenance therapy than those MRD-ve. In MRD +ve patients landmarked from 2y the HR was 0.34 [95%CI 0.19, 0.59], p<0.0001, 3y HR 0.26 [95%CI 0.11, 0.58], p=0.001 and 4y HR 0.14 [95%CI 0.04, 0.48], p=0.002. In MRD -ve patients landmarked from 2y the HR was 0.63 [95%CI 0.43, 0.94], p=0.025 but from 3y was no longer statistically significant (3y HR 0.65 [95%CI 0.36, 1.15], 4y HR 0.68 [95%CI 0.27, 1.69]). In patients with both standard and high-risk disease there was evidence of ongoing benefit of lenalidomide maintenance beyond 2-3 years.
Patients continuing lenalidomide maintenance long term did not experience worsening bone marrow suppression. In the first 6 months neutropenia was seen in 57% of patients, grade 1 (G1) 21%, G2 19%, G3 15% and G4 2.5%. This gradually reduced the longer patients were on maintenance therapy, e.g. during months 54-60 neutropenia was seen in only 40% of patients G1 20%, G2 17%, G3 3%, G4 0%.
Discussion In this analysis there is clear evidence that continuing lenalidomide maintenance beyond 3 years is associated with improved PFS, supporting recent findings from the DETERMINATION and STAMINA studies. There does, however, appear to be a time after ASCT at which continuing maintenance may no longer have ongoing benefit over observation. The current analysis suggests that between 4 and 5 years the impact diminished in all patients, earlier in the subgroup of patients MRD-ve after ASCT. Ongoing long term follow up of this and other studies is needed to define the optimal time point at which a randomised trial of stopping or continuing maintenance should be implemented.
source: https://ashpublications.org
These Medications Might Make Diabetic Retinopathy Worse

Ksenia Chernaya/Pexels
By Ross Wollen
December 19th, 2022
Diabetic retinopathy is a common complication of diabetes that affects the blood vessels in the retina, the light-sensitive tissue at the back of the eye. If left untreated, diabetic retinopathy can cause severe vision loss or even complete blindness.
The good news is that diabetic retinopathy (DR) can be diagnosed long before it actually begins to impact your vision. The condition is very treatable, and potentially even reversible, especially when caught early.
Doctors have a good understanding of what causes DR: high blood sugar, high blood pressure, and, to a lesser extent, high cholesterol. Diabetic retinopathy is very sensitive to metabolic health, and many of the medications that people with diabetes commonly take can affect its progression and development — for better or for worse.
This article will review the drugs that we know (or suspect) might worsen diabetic retinopathy.
Warning
A quick word of warning: This article shouldn’t be taken as medical advice, and no patient is qualified to decide for themselves whether to avoid any drug listed here. Many of these medications are important for the health of millions of adults, and their benefits may easily outweigh whatever effect they might have on DR.
If you’re concerned that you may be taking a medication that could make your diabetic retinopathy worse, please talk to your doctor. Only a medical professional is qualified to assess the unique totality of your health conditions to recommend medication adjustments.
The Two Diabetes Drugs That (Might) Make DR Worse
Most diabetes drugs have beneficial effects for diabetic retinopathy, slowing its progression and potentially even helping to reverse the damage. Taking your glucose-lowering medications as prescribed by your doctor is absolutely one of the best ways to protect yourself from DR.
There are, however, one and possibly two exceptions to that rule, as described by a recent survey of the topic in the medical journal Eye.
Thiazolidinediones (TZDs)
TZDs have been called “the forgotten diabetes medication.” These pills directly improve insulin resistance, a root cause of type 2 diabetes, but have been deemphasized by authorities due to concerns over harmful side effects, including cardiovascular disease.
Although these drugs are increasingly out of fashion, they are still commonly prescribed. As of 2019, about 8 percent of people with type 2 diabetes used a TZD.
TZDs carry a known risk of diabetic macular edema (DME), an especially damaging form of diabetic retinopathy that affects our keenest vision in the center of our eyesight. TZDs can cause fluid retention, which appears to exacerbate the swelling of blood vessels that characterizes DME. It only happens in a small number of cases — fewer than 3 percent of those that use the drug.
There are now two types of TZDs on the market:
- Rosiglitazone (Avandia)
- Pioglitazone (Actos)
Luckily, cessation is associated with rapid eye improvement.
Ozempic
There is some evidence that semaglutide (Ozempic), a GLP-1RA, may increase the incidence of diabetic retinopathy. One of several pivotal studies of semaglutide found an increased risk of DR, and the FDA has reported that a significantly higher percentage of Ozempic users have DR in comparison with users of similar drugs like dulaglutide (Trulicity) and liraglutide (Victoza). The connection is disputed, however, as another large study of semaglutide found no such risk.
Even if the association is real, it’s very possible that your own doctor would conclude that semaglutide is worth the risk. Ozempic is a very effective drug for people with diabetes, typically conferring both rapid glycemic improvements and weight loss.
It seems possible that Ozempic’s effectiveness, in fact, explains its negative effect on the eyes. Contrary to all expectations, rapid improvement in glucose control can actually worsen diabetic retinopathy. This is called “early worsening,” because the eyes will get worse before the major long-term benefits of better blood sugar control become evident.
Experts don’t believe that this is necessarily a reason to avoid Ozempic. A recent discussion of the issue by experts from the American Academy of Ophthalmology suggested that “early worsening” from Ozempic is both “temporary and manageable,” although it does call for increased scrutiny from eye doctors.
Other Drugs With Negative Metabolic Effects
Drugs That Increase Blood Sugar
Some medications are known to cause blood sugar spikes:
- Steroids, including hydrocortisone and prednisone, can have a dramatic effect on blood sugar. (Steroid creams and inhalers do not have the same effect).
- Hormonal birth control, including the pill, the shot, the patch, and the IUD
- Beta-blockers, which are used to treat hypertension, irregular heartbeat, and anxiety
- Anti-psychotic drugs, which are used to treat schizophrenia and related mental illnesses
If you take any of the above drugs, it might be wise to make sure your main diabetes healthcare provider is aware of it. They may or may not suggest an adjustment.
- Statins are also associated with rising blood sugar levels — but even taking that factor into account, experts still recommend statins for most adults with diabetes because they reduce the risk of cardiovascular disease.
Finally, if you have advanced diabetic retinopathy that requires treatment, you may be given steroid injections. These drugs can have a powerful anti-inflammatory effect within the eyeball that directly improves DR symptoms, even if they exert a negative effect on insulin sensitivity.
Drugs That Increase Blood Pressure
Hypertension (high blood pressure) is the other big factor that speeds the development and progression of diabetic retinopathy. Accordingly, medications that are known to raise your blood pressure can be considered risk factors for DR.
An incomplete list of some common drugs that can increase blood pressure includes:
- Pain relievers, including acetaminophen (Tylenol) and nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen (Motrin, Advil) and naproxen (Aleve)
- Antidepressants, including fluoxetine (Prozac), monoamine oxidase inhibitors, and tricyclic antidepressants
- Decongestants, including pseudoephedrine (Sudafed, Contac) and phenylephrine (Sudafed PE)
- Hormonal birth control, including the pill, the shot, the patch, and the IUD
- Stimulants, such as methylphenidate (Ritalin)
Some supplements, including caffeine and ginseng, can have a similar effect. The Mayo Clinic has a full article on the topic.
Drugs That Increase (Bad) Cholesterol
Experts are very confident that high blood sugar and high blood pressure both lead to diabetic retinopathy. The evidence linking high cholesterol with DR is not quite as strong, although we do know that some cholesterol-lowering drugs (especially fibrates) significantly reduce the incidence of DR.
These are some of the most common drugs that are believed to elevate “bad” cholesterol (LDL and/or triglycerides), which may or may not be risk factors for DR:
- Steroids
- Hormonal birth control, including the pill, the shot, the patch, and the IUD
- Retinoids (used to treat acne)
- Beta-blockers, which are used to treat hypertension, irregular heartbeat, and anxiety
- Diuretics
Drugs That Increase Weight
It should be no surprise that weight gain, which is so highly related to the development and progression of type 2 diabetes, is associated with an increased risk of diabetic retinopathy. A 2021 study in Korea found that patients with recent diagnoses of type 2 diabetes that lost 10 percent of their body weight cut their risk of DR in half, whereas those that had 10 percent weight gain tripled their risk.
It’s therefore probably fair to consider any drugs that cause weight gain as potential risk factors for DR.
Some of the most common drugs associated with weight gain include:
- Tricyclic antidepressants, including amitriptyline (Elavil), doxepin (Silenor), and nortriptyline (Pamelor)
- Selective serotonin reuptake inhibitors (SSRIs), another type of antidepressant, including escitalopram (Lexapro), paroxetine (Paxil), sertraline (Zoloft)
- Anti-psychotics, particularly olanzapine (Zyprexa)
- Anti-seizure medications, including gabapentin (Gralise), pregabalin (Lyrica), and vigabatrin (Sabril).
- Steroids
- Beta-blockers
- Antihistamines
The diabetes medications insulin and sulfonylureas are also associated with weight gain, which is why diabetes authorities have recently begun to prefer other options for glucose control.
Takeaways
Diabetic retinopathy is largely caused by poor metabolic health: high blood sugar, high blood pressure, and possibly high cholesterol. Many prescription medications have undesirable metabolic side effects and can therefore be considered potential contributors to DR.
Furthermore, two types of diabetes drugs in particular are associated with worsening diabetic retinopathy: the family of thiazolidinediones (TZDs), which includes rosiglitazone (Avandia) and pioglitazone (Actos), and semaglutide (Ozempic). Your ophthalmologist should be aware that you are taking one of these drugs, but will not necessarily advise a change, even if you are at high risk of vision loss from DR.
Many of the drugs discussed in this article are vital to the health of millions; therefore, it’s impossible to say whether or not readers should avoid them. As always, the guiding hand of a doctor that understands your unique health status is critical. It’s sometimes up to you to make sure that your various specialists are all on the same page. We encourage you to ensure that your main diabetes care provider and ophthalmologist are aware of every medicine you take.
This article has concentrated on the effects that various medications have on diabetic retinopathy. Medicine, of course, is only one factor of many — diet, exercise, glycemic control, and many other decisions play an immense role in the development and progression of diabetes complications.
Why Diabetes Experts Just Started Taking Sleep Health Very Seriously

Karolina Grabowska/Pexels
By Ross Wollen
December 23rd, 2022
The experts have selected a brand-new focus for doctors and caregivers who treat diabetes: sleep health.
The directive comes from the American Diabetes Association (ADA), which issues a new version of its Standards of Medical Care in Diabetes annually. This is the single most influential document in diabetes treatment, at least for Americans. The recommendations in this guidance govern the way that diabetes is treated in the country.
The 2023 edition, which was released on December 12, has an entirely new section on sleep health and explains in detail why diabetes experts now believe that sleep health can be such an important part of diabetes health.
Here’s the most important takeaway: Diabetes healthcare providers are now recommended to “consider screening for sleep health in people with diabetes” and to “refer to sleep medicine and/or a qualified behavioral health professional as indicated.”
In other words, if you’re having any problems getting healthy sleep, your sleep problems are now officially diabetes problems, and your doctor, nurse, or diabetes educator should help advocate for you to get the sleep help that you need.
Making the Case
We’ve discussed the many connections between sleep and diabetes in detail: The Importance of Sleep Health for Diabetes. Here, we’ll go over the evidence that led the ADA to make the change.
- Sleep disorders are a risk factor for developing type 2 diabetes.
Many elements of suboptimal sleep — including short sleep duration, obstructive sleep apnea, shift work, and insomnia — have been found to correlate with type 2 diabetes development and progression, enough for poor sleep to be named a significant risk factor for the disease.
- Sleep disorders may be a risk factor for developing gestational diabetes.
One large review, which evaluated 16 studies with data on millions of pregnant women, showed that women who got either too little sleep or too much sleep were more likely to develop gestational diabetes. Poor sleep quality, snoring, and obstructive sleep apnea only increased the risk.
- Sleep disturbances make diabetes self-management much more difficult.
If you live with diabetes, you know how true this is. When we’re exhausted, we are not in the right frame of mind to make the kind of methodical decisions that optimal diabetes care so often demands of us.
- Sleep disorders are extremely common in diabetes.
The ADA reports that more than half of people with type 1 diabetes have obstructive sleep apnea. In type 2, it could be as much as 86 percent! Insomnia, sleep disturbances, and restless leg syndrome are all common as well.
That so many people with diabetes deal with sleep disorders is further proof that there’s a significant link between sleep health and metabolic health — and all the more reason for diabetes doctors to make sleep health a priority.
- Diabetes can interfere with sleep (especially type 1).
Intensive insulin management leads to all sorts of sleep disturbances. Insulin pumps and continuous glucose monitors sound alarms in the middle of the night (sometimes these alarms are important, and sometimes they’re erroneous). Extreme blood sugars cause us to wake up drenched in sweat, disoriented, famished, or all of the above.
And then there’s the way that diabetes distress can impact sleep: It’s not easy to sleep well if your head isn’t in the right place, and diabetes is unfortunately associated with very high rates of stress, anxiety, and similar mental health challenges. The ADA cites a qualitative study that identified diabetes-related “emotional distress” as a major cause of sleep difficulties. Putting it all together, some people with diabetes almost never enjoy an uninterrupted good night’s sleep, which puts them at risk of the many health problems associated with poor sleep.
- Sleep therapy can reduce A1C and insulin resistance.
We know from a 2022 study that cognitive behavioral therapy can help patients improve both their metabolism (A1C, fasting blood sugar, and blood pressure) and their sleep quality. Pharmacological intervention may help too; a 2021 study found that both behavioral medication and sleeping pills can improve insulin resistance and may also improve A1C.
Additional Factors
We actually think that the ADA is only scratching the surface here in connecting sleep health to diabetes health:
- Sleep quality is intertwined with diet quality. A poor night’s sleep makes you more likely to binge on unhealthy foods, and unhealthy foods probably lower sleep quality, a vicious cycle.
- Good sleep is essential for a properly functioning immune system — a special concern for people with diabetes, who are generally more susceptible to infections and illnesses.
- Good sleep is also essential for good mental health, another huge issue for many people with diabetes.
- Sleep quality and quantity can moderate your risk for cardiovascular disease.
We’ve got links and details on all of the above in our article on the importance of sleep health for diabetes.
For ideas on how to create healthier sleep habits, check out this link from our partners at Everyday Health: Sleep 101: The Ultimate Guide to a Better Night’s Sleep.
The Bottom Line
Sleep is a surprisingly important factor in diabetes management, in so many ways. Getting the right amount of sleep isn’t a cure-all, but it can help get your health back on the right track, putting you in the best possible position to manage your diabetes optimally.
If you have sleep issues, it may be time to take them seriously as a health problem that you need to solve. Consider this news an encouragement to discuss any sleep issues with the healthcare provider you see for your diabetes. There’s a growing recognition that sleep health and metabolic health are intimately related, and it may soon become easier for you to get the help you need.
10 Ways to Achieve Your Healthiest Weight Yet

Jonathan Borba/Pexels
December 26th, 2022
It’s the new year, and as usual, there will be a spike in interest in dieting and weight loss. Unfortunately, these resolutions are often made in ways that definitely do not set up dieters for success. We are better at shifting habits when we can find truly meaningful motivation.
If your goals for healthy living include any aspect of managing your weight, keep the following thoughts in mind for a sustainable approach to achieving your healthiest weight yet.
Don’t Wait to Begin — Do It Now
Looking for benchmarks to start a new way of eating, quit an old habit, or begin an exercise routine is natural, but unnecessary. You can change direction at any time. If you missed the opportunity to start your new routines on January 1st, you don’t have to wait until next year or even next month to make a change. You can do it now!
If you fall off the wagon, you don’t have to wait until next week or even tomorrow to try again. Look at the next possible opportunity you have to make a healthy choice that leads you closer to your goals and make the choice, right then and there.
Make as Many Ideal Food Choices as Possible

Engin Akyurt/Pexels
It’s easy to get caught up in strict rules around eating when weight is in mind. The odds are good that if you make more ideal food choices than not, you will feel better and the weight goals will follow.
If you have the opportunity to choose your food six times throughout a day (let’s say breakfast, morning snack, lunch, afternoon snack, dinner, and after-dinner treat/snack), and you make healthy choices that meet the criteria that you have set for yourself at least three times throughout a day, you will be meeting your goal 50% of the time. If you can work up to five out of six, that’s 83%. It’s not a zero-sum game where each day becomes an automatic failure if you don’t meet 100%. Each opportunity to choose is a fresh slate and doesn’t require waiting for the next day to try again.
Choose One Change at a Time
As you set out to make a series of new choices on your journey, you will find that some choices achieve the desired results while others don’t seem to be working for you.
If you’re trying to make a million changes, think about slowing down. Give each change the attention it deserves, one at a time. You don’t want to overwhelm yourself with too many changes at once and feel discouraged if you aren’t able to keep up with a whole slew of modifications. Making more than one change at once may mean not being able to determine what results correlate with each change. Isolating the adjustments helps you to determine which steps are working, and which are not.
Put Your Carb Counting in Context
As people living with diabetes, we are always aware of our carbohydrate consumption. We count carbs, we know the difference between high-quality and low-quality carbs, and we study how different amounts and types of carb consumption affect our diabetes management and overall well-being. And it’s easy to forget that there are other pieces to the puzzle, like fat and protein.
Here are some questions to ask yourself about carb counting that may help you to dig deeper into the relationship between your diabetes management and weight loss goals:
- How does my fat and protein intake affect the absorption of the carbohydrates I am eating?
- What foods can I use as building blocks for my meals that will have a minimal impact on my blood glucose levels?
- When does the timing of my insulin/medications and food work best for achieving my diabetes goals?
- Where do I have the opportunity to make dietary changes that work for my vision of weight management, diabetes management, and quality of life?
Eat When You Are Hungry
This one seems like it could be a no-brainer, but like many of the behaviors associated with weight management, it isn’t always easy. If you are hungry, eat. Make the healthiest choice possible for your meal or snack, enjoy it slowly, and give yourself the time to sit and feel full before thinking about whether you need to go back for more. If you are not hungry, don’t eat (unless your blood sugar is low, of course!). Try to eliminate situations where you are eating for other reasons, like emotions, boredom, or habit.
While it is important to be flexible for occasions that demand it, creating a daily routine for eating is helpful for both weight and diabetes management.
Listen to Your Body
Our body gives us feedback that can guide us in healthy decision-making. For example, if your body is sluggish and reliant on caffeine to make it through the day, perhaps it is telling you it needs more “clean fuel,” like sleep and whole foods. Every individual is different, so the cues for one person may not be the same for another.

Kelvin Valerio/Pexels
Think about how sensitive you are to blood glucose fluctuations in either direction, and try to apply that kind of responsiveness to your hunger levels. If you can get more in tune with the messages your body is sending, it’ll pay off.
Mentally Prepare Yourself for Success
If you have struggled with managing your weight in the past, you might be dealing with internal messages of self-doubt. That is normal. However, embracing a positive mindset and the spirit of willing experimentation will get you far.
Look in the mirror and repeat the affirmation “I have the tools and knowledge to reach success. I am strong enough to make this journey.” You can come up with your own affirmation that speaks to you. Write it down. Say it aloud. Most importantly, believe that it is true.
Celebrate Your Journey
The road to weight loss is generally not linear. It takes a while to figure out the combination of modifications to see progress. Sometimes circumstances throw us for a loop. Results may come easily, then stagnate or reverse. In the moment, these are frustrating roadblocks. In the big picture, these are small inconveniences.
Celebrate when you make a healthy choice and follow it up with another one, make it one step closer to your goal, and see how the changes you are making are positively affecting your diabetes management. Success is not simply a destination; it can be found throughout the journey. Find joy in each of these moments as you move forward.
Monitor How Your New Habits Are Affecting Your Diabetes
As we know, eating differently or adding physical activity are just two of many factors that can affect our blood glucose levels. Lifestyle modifications may require you or your doctor to consider changes to your insulin or medication, or otherwise alter how you self-manage your diabetes. It helps to make notes of these changes so you can keep track, both for yourself and for your doctor.
Cardio exercise and lower-carbohydrate diets are two popular weightloss strategies that can quickly shift the amount of insulin or other glucose-lowering medication that you need. Be prepared to counteract hypoglycemia with fast-acting carbohydrates, like juice or glucose tabs. Losing weight increases insulin sensitivity and may affect your basal insulin or mealtime doses, making adjustments accordingly.
Remember: Your Weight Management Journey May Vary
You are unique. Your weight management journey is going to be different than that of your neighbor or the person posting about it in your diabetes Facebook group. You can try strategies that are suggested by others, but don’t be discouraged if that advice doesn’t necessarily reap rewards for you. Keep your eye on the prize (your goals!), do what is best for your body, and the rest will follow.