







Merry Christmas to all my Blog subscribers and followers.
Happy Reading. Hope you all are enjoying my posts.
Season greetings and Merry Xmas to all of you. Happy Holiday !!😍🎉🥳
Dr Chandan Aryan
New Delhi,India
Email: aryan.chandan@dr.com








Merry Christmas to all my Blog subscribers and followers.
Happy Reading. Hope you all are enjoying my posts.
Season greetings and Merry Xmas to all of you. Happy Holiday !!😍🎉🥳
Dr Chandan Aryan
New Delhi,India
Email: aryan.chandan@dr.com
Intercept Pharmaceuticals, Inc. (Nasdaq: ICPT), a biopharmaceutical company focused on the development and commercialization of novel therapeutics to treat progressive non-viral liver diseases, today announced a key publication in Gastroenterology showing that people receiving OCA for primary biliary cholangitis (PBC) in a clinical trial setting had greater transplant-free survival compared to patients with PBC selected from “real-world” patient registries who did not receive OCA.
Key findings include:
“This important study is the first to demonstrate that initiating treatment with OCA in appropriate patients with PBC appears to have a meaningful impact on clinical outcomes,” said Professor Gideon Hirschfield, FRCP, Ph.D., Lily and Terry Horner Chair in Autoimmune Liver Disease at the University of Toronto. “I am proud of this innovative analysis, and further, the continued value we are deriving from large, academic-led, prospective databases like the Global PBC and UK-PBC study groups. Leveraging these registries helps advance our collective understanding of this disease to ultimately influence clinical decision-making and benefit people living with PBC.”
“Given the known challenges associated with conducting blinded, placebo-controlled trials when the treatment has been approved and is available, this study provides evidence that a well-matched external comparator group can be a credible, alternate approach to evaluating clinical efficacy,” said M. Michelle Berrey, M.D., M.P.H., President of Research & Development and Chief Medical Officer of Intercept. “We look forward to further leveraging real-world databases to continue generating insights on the clinical benefit of Ocaliva in PBC.”
This study compared patients with PBC who received up to six years of OCA in the Phase 3 POISE study and its open-label extension (n=209) to external controls who were extracted from two large, academic-led patient registries. External controls met POISE entry criteria but were not treated with OCA. Treatment with ursodeoxycholic acid (UDCA) was permitted.
The primary endpoint of this study was time to first occurrence of liver transplant or death. Over the six-year follow-up, there were five deaths/liver transplants in 209 subjects in the POISE study, 135 in 1,381 patients in the Global PBC control, and 281 in 2,135 patients in the UK-PBC control. Preliminary results from this analysis were first presented at the 2021 Annual Meeting of the American Association for the Study of Liver Diseases (AASLD).
Data Sources for this Study:
The Global PBC registry included 6,484 patients with PBC from eight countries in Europe and North America during the study period who were not treated with OCA. Of these, 1,381 met the entry criteria for this study.
The UK-PBC registry included over 6,900 patients with PBC from the UK during the study period who were not treated with OCA. Of these, 2,135 met the entry criteria for this study.
The POISE trial studied the safety and efficacy of once-daily treatment with Ocaliva in PBC patients with an inadequate therapeutic response to, or who were unable to tolerate, ursodeoxycholic acid (UDCA). There were 217 patients randomized to one of three groups in the trial: placebo, OCA 10 mg, or OCA 5 mg for six months titrated to 10 mg based on clinical response. Seven subjects did not participate in the open-label extension and were not included in the current study. Patients completing the double-blind phase had the option to continue in an open-label extension (OLE) phase for a maximum of five additional years, during which all patients received treatment with OCA 5-10 mg once daily. Of the 198 patients who completed the double-blind phase, more than 95 percent continued in the long-term safety extension phase of the trial. Additional information regarding the POISE trial can be found on the NIH clinical study listing website: http://clinicaltrials.gov/ct2/show/NCT01473524.
About Primary Biliary Cholangitis
Primary biliary cholangitis (PBC) is a rare, progressive and chronic autoimmune disease that affects the bile ducts in the liver and is most prevalent (approximately 1 in 10,000) in women over the age of 40. PBC causes bile acids to build up in the liver, resulting in inflammation and scarring (fibrosis), which, if left untreated, can lead to cirrhosis, liver transplant, or death.
About Intercept
Intercept is a biopharmaceutical company focused on the development and commercialization of novel therapeutics to treat progressive non-viral liver diseases, including primary biliary cholangitis (PBC) and nonalcoholic steatohepatitis (NASH). For more information, please visit www.interceptpharma.com or connect with the company on Twitter and LinkedIn.
About Ocaliva® (obeticholic acid)
OCALIVA, a farnesoid X receptor (FXR) agonist, is indicated for the treatment of adult patients with primary biliary cholangitis (PBC).
This indication is approved under accelerated approval based on a reduction in alkaline phosphatase (ALP). An improvement in survival or disease-related symptoms has not been established. Continued approval for this indication may be contingent upon verification and description of clinical benefit in confirmatory trials.
IMPORTANT SAFETY INFORMATION
WARNING: HEPATIC DECOMPENSATION AND FAILURE IN PRIMARY BILIARY CHOLANGITIS PATIENTS WITH CIRRHOSIS
Contraindications
OCALIVA is contraindicated in patients with:
Warnings and Precautions
Hepatic Decompensation and Failure in PBC Patients with Cirrhosis
Hepatic decompensation and failure, sometimes fatal or resulting in liver transplant, have been reported with OCALIVA treatment in PBC patients with cirrhosis, either compensated or decompensated. Among post-marketing cases reporting it, median time to hepatic decompensation (e.g., new onset ascites) was 4 months for patients with compensated cirrhosis; median time to a new decompensation event (e.g., hepatic encephalopathy) was 2.5 months for patients with decompensated cirrhosis.
Some of these cases occurred in patients with decompensated cirrhosis when they were treated with higher than the recommended dosage for that patient population; however, cases of hepatic decompensation and failure have continued to be reported in patients with decompensated cirrhosis even when they received the recommended dosage.
Hepatotoxicity was observed in the OCALIVA clinical trials. A dose-response relationship was observed for the occurrence of hepatic adverse reactions including jaundice, worsening ascites, and primary biliary cholangitis flare with dosages of OCALIVA of 10 mg once daily to 50 mg once daily (up to 5-times the highest recommended dosage), as early as one month after starting treatment with OCALIVA in two 3-month, placebo-controlled clinical trials in patients with primarily early stage PBC.
Routinely monitor patients for progression of PBC, including hepatic adverse reactions, with laboratory and clinical assessments to determine whether drug discontinuation is needed. Closely monitor patients with compensated cirrhosis, concomitant hepatic disease (e.g., autoimmune hepatitis, alcoholic liver disease), and/or with severe intercurrent illness for new evidence of portal hypertension (e.g., ascites, gastroesophageal varices, persistent thrombocytopenia), or increases above the upper limit of normal in total bilirubin, direct bilirubin, or prothrombin time to determine whether drug discontinuation is needed. Permanently discontinue OCALIVA in patients who develop laboratory or clinical evidence of hepatic decompensation (e.g., ascites, jaundice, variceal bleeding, hepatic encephalopathy), have compensated cirrhosis and develop evidence of portal hypertension (e.g., ascites, gastroesophageal varices, persistent thrombocytopenia), experience clinically significant hepatic adverse reactions, or develop complete biliary obstruction. If severe intercurrent illness occurs, interrupt treatment with OCALIVA and monitor the patient’s liver function. After resolution of the intercurrent illness, consider the potential risks and benefits of restarting OCALIVA treatment.
Severe Pruritus
Severe pruritus was reported in 23% of patients in the OCALIVA 10 mg arm, 19% of patients in the OCALIVA titration arm, and 7% of patients in the placebo arm in a 12-month double-blind randomized controlled clinical trial of 216 patients. Severe pruritus was defined as intense or widespread itching, interfering with activities of daily living, or causing severe sleep disturbance, or intolerable discomfort, and typically requiring medical interventions. Consider clinical evaluation of patients with new onset or worsening severe pruritus. Management strategies include the addition of bile acid binding resins or antihistamines, OCALIVA dosage reduction, and/or temporary interruption of OCALIVA dosing.
Reduction in HDL-C
Patients with PBC generally exhibit hyperlipidemia characterized by a significant elevation in total cholesterol primarily due to increased levels of high-density lipoprotein-cholesterol (HDL-C). Dose-dependent reductions from baseline in mean HDL-C levels were observed at 2 weeks in OCALIVA-treated patients, 20% and 9% in the 10 mg and titration arms, respectively, compared to 2% in the placebo arm. Monitor patients for changes in serum lipid levels during treatment. For patients who do not respond to OCALIVA after 1 year at the highest recommended dosage that can be tolerated (maximum of 10 mg once daily), and who experience a reduction in HDL-C, weigh the potential risks against the benefits of continuing treatment.
Adverse Reactions
The most common adverse reactions (≥5%) are: pruritus, fatigue, abdominal pain and discomfort, rash, oropharyngeal pain, dizziness, constipation, arthralgia, thyroid function abnormality, and eczema.
Drug Interactions
Patients who received obeticholic acid for primary biliary cholangitis experienced greater transplant-free survival compared with external control patients, according to research published in Gastroenterology.
“This important study is the first to demonstrate that initiating treatment with obeticholic acid (OCA) in appropriate patients with primary biliary cholangitis (PBC) appears to have a meaningful impact on clinical outcomes,” Gideon Hirschfield, FRCP, PhD, Lily and Terry Horner Chair in autoimmune liver disease at the University of Toronto, said in a press release.

Although first-line therapy with ursodeoxycholic acid has been shown to improve transplant-free survival in PBC, nearly 40% of patients treated with ursodeoxycholic acid experience an inadequate response, with increased risk for hepatic complications and poor outcomes. Obeticholic acid had been given accelerated FDA approval for inadequate responders in 2016, with full approval contingent on establishing benefit for clinical outcomes, including hepatic decompensation, liver transplant and mortality.
Using data from the POISE trial, Hirschfield and colleagues compared results of patients treated with OCA from the double-blind and open label extension periods (n = 209) with those generated by “real-world controls” not treated with OCA from the Global PBC (n = 1,381) and UK PBC (n = 2,135) registry studies.
Baseline characteristics reflected a predominantly female epidemiology of PBC with most diagnosed between 50 and 60 years of age and receiving ursodeoxycholic acid therapy between 900 mg/day and 1,000 mg/day for 3.5 to 4 years at index. The primary outcome was time to first occurrence of liver transplant or death.
Over 6 years of follow-up, researchers observed liver transplantation or death among 2.4% of patients from the POISE cohort, 10% of patients from the Global PBC cohort and 13.2% of patients from the UK PBC cohort.
Pre-specified propensity scoring yielded hazard ratios of 0.29 (95% CI, 0.1-0.83) for POISE vs. Global PBC and 0.3 (95% CI, 0.12-0.75) for POISE vs. UK PBC; researchers noted these results indicated patients treated with OCA in a trial setting had a “significantly greater transplant-free survival than patients in either external control group.”
Further analysis revealed 16 incidences of death, liver transplant or hepatic decompensation among 209 patients in the POISE cohort vs. 212 incidences among 1,381 patients in the Global PBC cohort (HR = 0.42; 95% CI, 0.21-0.85).
“Given the known challenges associated with conducting blinded, placebo-controlled trials when the treatment has been approved and is available, this study provides evidence that a well-matched external comparator group can be a credible, alternate approach to evaluating clinical efficacy,” Michelle Berrey, MD, MPH, president of research and development and chief medical officer at Intercept Pharmaceuticals, said in the release. “We look forward to further leveraging real-world databases to continue generating insights on the clinical benefit of Ocaliva (OCA, Intercept) in PBC.”
“Pruritus is commonly associated with primary biliary cholangitis, present in nearly 75% of patients over the disease course,” Cynthia Levy, MD, FAASLD, AGAF, of the University of Miami Miller School of Medicine, and colleagues wrote. “Pruritus substantially impairs health-related quality of life, affecting sleep and contributing to fatigue.”

According to researchers, linerixibat — a minimally absorbed oral small molecule ileal bile acid transporter inhibitor — reduced cholestatic pruritus without serious adverse events in a phase 2a study. In addition, treatment with linerixibat reduced bile acid levels and improved sleep interference and fatigue compared with placebo.
To expand on these findings, Levy and colleagues conducted the multicenter, randomized phase 2b GLIMMER study to investigate the safety, efficacy and dose-response of linerixibat among 147 patients (mean age, 55.8 years, 94% women) with moderate to severe pruritus-associated primary biliary cholangitis (PBC), defined as an itch score of at least 4 on the numerical rating scale (NRS).
After 4 weeks of single-blind placebo, patients received linerixibat once (20 mg, n = 16; 90 mg, n = 23; 180 mg, n = 27) or twice daily (40 mg, n = 23; 90 mg, n = 22) or placebo (n = 36) for 12 weeks. Patients measured their itch score (0-10 NRS) twice daily, and researchers determined daily, weekly and monthly itch scores. The primary endpoint was change in mean worst daily itch (MWDI) score compared with baseline.
According to study results, there was a reduction from baseline in MWDI scores (mean 2 points) among patients dosed with linerixibat at week 16. Although these differences were not significant compared with placebo, post-hoc analysis of change in monthly itch score yielded “significant differences” between placebo and linerixibat 180 mg once daily (least squares mean change = –0.9; 95% CI, –1.76 to –0.03), 40 mg twice daily (–1.16; 95% CI, –2.05 to –0.28) and 90 mg twice daily (–0.95; 95% CI, –1.85 to –0.06).
Further, a linear model of total daily dose of linerixibat in the per protocol population yielded a “statistically significant” reduction vs. placebo in MWDI score at the 10% level, indicating a dose-response relationship.
According to researchers, commonly reported adverse events included diarrhea and abdominal pain, which occurred more often at higher linerixibat doses.
“Targeting bile acid reuptake with linerixibat may provide relief for patients with PBC and cholestatic pruritus, along with improvements in health-related quality of life relating to itch,” Levy and colleagues concluded. “Twice-daily dosing was associated with greater itch improvement.”
They added, “This study identified a linerixibat dose for further investigation, and a confirmatory study is ongoing in PBC patients with moderate to severe itch which includes a longer double-blind dosing period and analysis of itch intensity throughout the study period rather than at a single timepoint.”
Obesity was not a universal phenotype among children with type 2 diabetes, despite being an important risk factor, according to a systematic review and meta-analysis published in JAMA Network Open.
“While the complex weave of factors driving the pathogenesis of pediatric type 2 diabetes are not yet fully defined, the biopsychosocial determinants of health with health inequities and social and economic vulnerabilities in this population play an important role in disease risk and outcomes,” M. Constantine Samaan, MD, MSc, associate professor in the department of pediatrics at McMaster University and a staff physician in the division of pediatric endocrinology at McMaster Children’s Hospital in Hamilton, Ontario, Canada, and colleagues wrote. “Obesity is a major trigger for screening for type 2 diabetes in clinical practice, yet the prevalence of obesity in the pediatric type 2 diabetes population is unknown.”

In this systematic review and meta-analysis, researchers searched through MEDLINE, Embase, CINAHL, Cochrane Library and Web of Science from inception to June 2022 and identified observational studies with at least 10 participants with reports on the prevalence of obesity in individuals with pediatric type 2 diabetes. Overall, researchers included 57 studies in the systematic review and 53 studies in the meta-analysis.
The primary outcome included pooled prevalence rates of obesity among children with type 2 diabetes. Secondary outcomes included pooled prevalence rates of obesity among children with type 2 diabetes by sex and race as well as associations between obesity and glycemic control and dyslipidemia.
Among individuals with pediatric type 2 diabetes, researchers observed an overall obesity prevalence of 75.27% with a prevalence of 77.24% at diabetes diagnosis among 4,688 children. Boys had higher odds of obesity compared with girls (78.65% vs. 59.2%; OR = 2.1; 95% CI, 1.33-3.31; P = .03) and, compared with other racial groups, Asian children had the lowest obesity prevalence (64.5%) and white children had the highest (89.86%; P < .001 for both).
In addition, when assessing obesity prevalence by region, North America had the highest prevalence among children with type 2 diabetes compared with Europe (81.14% vs. 68.3%; P < .001 for both).
There were no significant associations between obesity prevalence and dyslipidemia or HbA1c levels in children with type 2 diabetes.
“Further research is needed to evaluate the causes of sex- and race and ethnicity-based associations of diabetes with obesity and explore additional factors that may affect the risk of developing type 2 diabetes apart from obesity in children,” the researchers wrote.
The use of wearable digital health monitors that measure itch and scratch during sleep appeared useful for patients with atopic dermatitis, according to study results.
“If a person knows how much itching they’re having at night, then they can also share that with their physician or other health care practitioner, informing them of the status of their atopic dermatitis,” Donna D. (De De) Gardner, DrPH, RRT, FCCP, FAARC, director of research and evaluation at Allergy & Asthma Network, told Healio.

For the study, presented at the American College of Allergy, Asthma & Immunology Annual Scientific Meeting, researchers recruited respondents from a dermatology office and the Allergy & Asthma Network community via email between December 2020 and April 2021. Most of the participants were white women aged 35 to 50 years, Gardner said.
Participants needed to have an Apple iPhone and Apple Watch; those without the watch received one to use during the study.
Next, participants downloaded the DermaTrack (Embleema) application onto their iPhone to measure vibrations and movement in the skin and record when users scratch themselves.
The participants also completed the Dermatology Life Quality Index (DLQI) and a demographic survey, in addition to daily surveys and a final satisfaction survey.
Of the 81 participants who completed the DLQI, 53 said that their AD determined what clothes they were going to wear each day, 41 said their social activities depended on their AD status, 28 said they were hesitant to have sex with their partner because of their AD and 61 said they were embarrassed or overly conscious of their AD.
“And then 73, almost all of the participants, said that their skin was itchy, sore and painful,” said Gardner. “So atopic dermatitis does, as we know, impact quality of life.”
Overall, 79% of the participants agreed that AD had a moderate to large effect on their life.
For 7 nights, the participants wore the Apple Watch while they slept.
Data from the app showed patients experienced a maximum of 32 minutes of itching a night, indicating scratch from AD impacts sleep as well, Gardner said.
“If you could imagine itching constantly for 32 minutes, that’s painful and is going to interrupt your sleep,” Gardner said. “These people are not sleeping at night, and their quality of life is poor.”
The app’s dashboard then let participants review these data and share it with their physicians. Although 89% of the participants agreed that the information was useful, only 53% said it would enable them to better discuss their AD with their physician, and even fewer said they would do so.
“The sad thing is that even though people were informed, only a third of them said they would actually have the conversation,” Gardner said. “That tells you that they are hesitant to have the conversation with their health care provider about the status of their atopic dermatitis.”
Engaging the brain’s plasticity by stimulating the locus coeruleus, a region in the brainstem, could be a clinically relevant approach to optimize the efficacy of cochlear implants in restoring hearing in the deaf, claims a study published in the journal Nature on December 21, 2022. The study “Locus coeruleus activity improves cochlear implant performance,” uses rat models fitted with multichannel cochlear implants to examine neuromodulation and plasticity in learning and performance following cochlear implantation.

Lead author of the study, Erin Glennon, PhD, a medical student at NYU Grossman School of Medicine said, “Our findings suggest that differences in neuroplasticity, particularly in parts of the brain such as the locus coeruleus, may help explain why some cochlear implant users improve faster than others.”
Co-senior author Robert Froemke, PhD, a professor of genetics at NYU Langone, said, “improving neuroplasticity in the locus coeruleus may speed up and bolster the effectiveness of cochlear implants.”
Cochlear implants are the first neuroprosthetic electronic devices to restore a human sense. Despite their success in enabling some recipients to understand speech within a few hours, it can take months or years before implantation results in an optimal perception of speech in others.
Experts believe that differences in neuroplasticity in the central auditory system may be responsible for this variable effectiveness. However, technical challenges in monitoring and manipulating neural activity in humans and animal models have left unanswered questions regarding neural mechanisms that control the brain’s ability to adapt to the implant.
Lina Reiss, PhD, associate professor of otolaryngology and biomedical engineering at Oregon Health & Science University said, “Clinically, this [study] might pave the way for novel treatments or even behavioral training strategies to better engage the locus coeruleus to speed up re-learning auditory processing through a cochlear implant. Stimulation of the locus coeruleus may also help poorly performing patients improve further even if they have plateaued.” (Reise studies pitch and speech perception in children and adults with cochlear implants and mechanisms of hearing loss after cochlear implantation. She was not involved in the current study.)
Cochlear implants consist of an externally worn microphone, sound processor and transmitter, and an implanted electrode system that receives signals from the external system and stimulates nerves in the inner ear.
Noradrenaline produced by the locus coeruleus is a key factor in inducing neuroplasticity. Earlier studies by the same group had shown electric stimulation of the locus coeruleus in normal rats increases neuroplasticity, accelerates learning new reward associations, and influences how the brain represents sound. The current study builds on their earlier work to demonstrate stimulation of the locus coeruleus hastens hearing in cochlear implant recipients. The investigators analyzed behavioral responses and neural activity in the locus coeruleus and the auditory cortex of deafened rats with multi-channel cochlear implants.
First, they trained normal rats on an auditory task that rewarded the animals on successful performance. The rats were trained to press a button when they heard a specific sound and to ignore the button if they heard a different tone. The rats showed substantial differences in learning rates and peak performance. Using photometry of the locus coeruleus, the researchers could predict when rats began responding to sounds and exhibited long-term accuracy in hearing.
As expected, deafened rats could not complete the task. The deafened rats were then given cochlear implants and retrained to perform the same task. Next, the researchers separated deafened rat models with the implanted neuroprosthetic into two sets, stimulating one group in the locus coeruleus with optogenetic stimulation while the other set of rats received no stimulation.
They found rats that were stimulated learned faster with higher long-term accuracy. In the reward-based auditory task, the stimulated rats showed enhanced performance and corresponding responses in the auditory cortex. Rats that received an optogenetic boost in the locus coeruleus could successfully complete the auditory task within three days while those that did not receive the boost took up to 16 days.
Activity in the locus coeruleus changed as the rats learned to use their implants. At initial stages, the locus coeruleus showed peak activity only when the animals received the reward, but later, activity peaked immediately following the tone. The speed of this change of activity in the locus coeruleus mirrored the animals’ ability to consistently succeed at the task.
“Previous studies have focused on the peripheral factors that govern variability—this study is innovative in finding a way to investigate central processing factors in an animal model, by focusing on the locus coeruleus,” said Reiss. “The findings have implications for our understanding of individual differences in how fast people can re-learn to hear through a cochlear implant, from the central auditory processing aspect.”
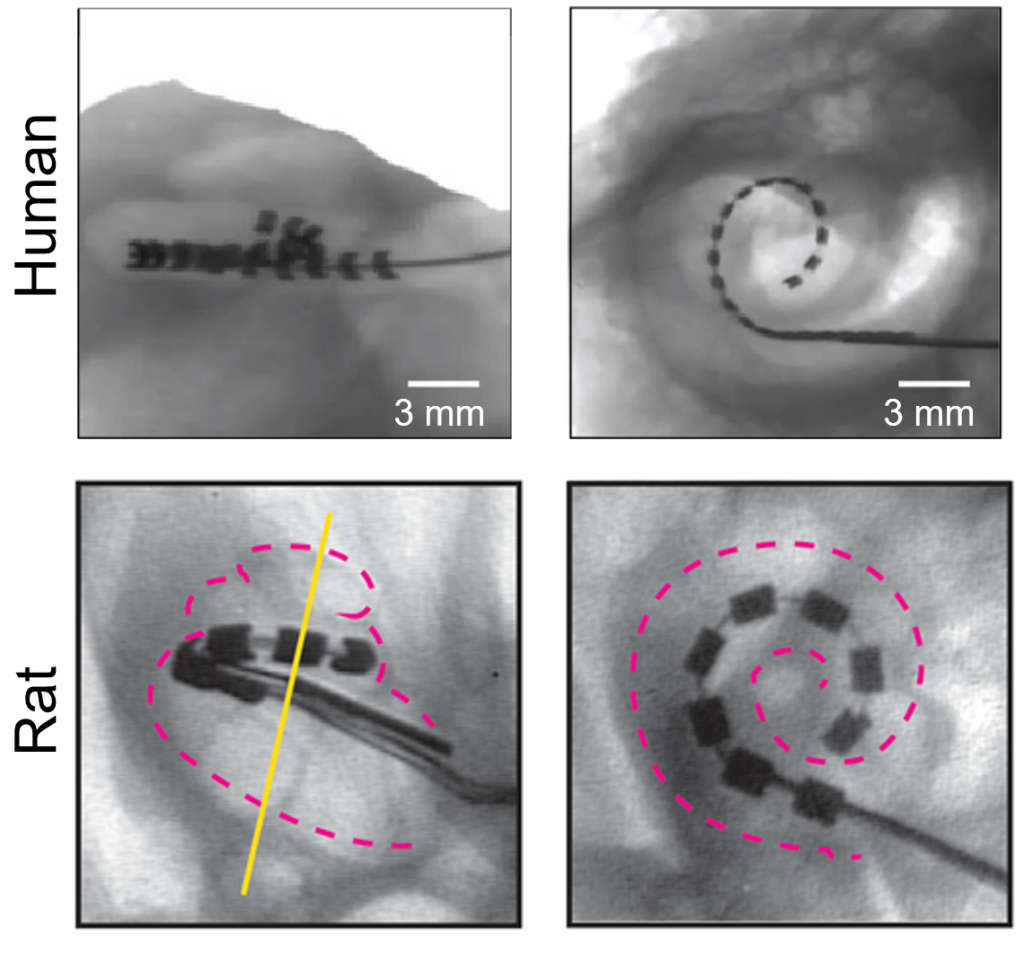
In future projects, the team intends to explore ways of stimulating the locus coeruleus in humans. “We need to determine what noninvasive mechanisms may be used to trigger the brain region,” said Mario Svirsky, PhD, professor of otolaryngology at NYU Langone and co-senior author of the study. Svirsky cautions that the current study tested hearing in rats using simple sounds in a straightforward task, while humans need to respond to nuanced speech patterns in noisy environments. Translating the insights from the current study to humans will require further research.

Scientists at the Institute for the Advanced Study of Human Biology (ASHBi) at Kyoto University say they used a petri dish and induced pluripotent stem cells (iPSCs) to learn how the early stages of the human body plan are established.
In their study “Reconstituting human somitogenesis in vitro,” published in Nature, Cantas Alev, MD, PhD, and his team created a cocktail consisting of human iPSC-derived cells and Matrigel, a viscous gel compound enriched with extracellular matrix components, to generate a 3D model that reportedly can recapitulate the development of our early body plan in a dish, which they coined “axioloids.”
“Our (bottom-up) approach of generating axioloids has not only allowed us to uncouple fundamental biological processes, such as cell morphology and cell states, but it allowed us to determine how mutationscontribute to spine disease,” explains Alev. “We also anticipate similar strategies will become increasingly necessary in order to understand better the etiology and pathology of other diseases.”
The segmented body plan of vertebrates is set up during somitogenesis, a well-studied process in model organisms, but remains elusive in humans due to ethical and technical limitations, note the investigators. “Despite recent advances with pluripotent stem cell (PSC)-based approaches, models that robustly recapitulate human somitogenesis in both space and time are still largely missing,” they write.
“Here, we introduce a PSC-derived mesoderm-based 3D model of human segmentation and somitogenesis, which we termed ‘axioloid’, that captures accurately the oscillatory dynamics of the segmentation clock and the morphological and molecular characteristics of sequential somite formation in vitro. Axioloids show proper rostrocaudal patterning of forming segments and robust anterior-posterior FGF/WNT signaling gradients and retinoic acid (RA) signaling components.
“We identify an unexpected critical role of RA signaling in the stabilization of forming segments, indicating distinct, but also synergistic effects of RA and extracellular matrix (ECM) on the formation and epithelialization of somites. Importantly, comparative analysis demonstrates striking similarities of axioloids to the human embryo, further validated by the presence of a HOX code in axioloids.
“Lastly, we demonstrate the utility of axioloids to study the pathogenesis of human congenital spine diseases, by using patient-like iPSCs with mutations in HES7 and MESP2. These results suggest that axioloids represent a promising novel platform to study axial development and disease in humans.”
“(Our) axioloids capture, not only the oscillatory nature of the segmentation clock, but also the molecular as well as the 3-D morphological and structural characteristics observed during the process of segmentation and somitogenesis” notes Alev, whose team identified a previously unappreciated functional role for retinoids during somite formation.
“Our [study] was critical to unraveling the role of retinoids during somitogenesis. It is likely that many researchers missed this essential role because vitamin A is a common supplement that usually gets included into culture media.”
When the axioloids were compared to actual human embryos, they revealed “remarkable similarities to Carnegie Stage 9-12 human embryos, which is known to be a critical stage during human development where organs such as the brain and heart start forming,” he remarks.

In this 2012 image provided by Lawrence Livermore National Laboratory, a technician reviews an optic inside the preamplifier support structure at the Lawrence Livermore National Laboratory in Livermore, Calif. The major advance in fusion research announced in Washington on Tuesday, Dec. 13, 2022, was decades in coming, with scientists for the first time able to engineer a reaction that produced more power than was used to ignite it. (Damien Jemison/Lawrence Livermore National Laboratory via AP)
The major advance in fusion research announced in Washington on Tuesday was decades in coming, with scientists for the first time able to engineer a reaction that produced more power than was used to ignite it.
Using powerful lasers to focus enormous energy on a miniature capsule half the size of a BB, scientists at the Lawrence Livermore National Laboratory in California started a reaction that produced about 1.5 times more energy than was contained in the light used to produce it.
There are decades more to wait before fusion could one day — maybe — be used to produce electricity in the real world. But the promise of fusion is enticing. If harnessed, it could produce nearly limitless, carbon-free energy to supply humanity’s electricity needs without raising global temperatures and worsening climate change.
At the press conference in Washington, the scientists celebrated.
“So, this is pretty cool,” said Marvin “Marv” Adams, the National Nuclear Security Administration deputy administrator for defense programs.
“Fusion fuel in the capsule got squeezed, fusion reactions started. This had all happened before – 100 times before – but last week for the first time they designed this experiment so that the fusion fuel stayed hot enough, dense enough and round enough for long enough that it ignited,” said Adams. “And it produced more energy than the lasers had deposited.”
Here’s a look at exactly what nuclear fusion is, and some of the difficulties in turning it into the cheap and carbon-free energy source that scientists hope it can be.
Look up, and it’s happening right above you — nuclear fusion reactions power the sun and other stars.
The reaction happens when two light nuclei merge to form a single heavier nucleus. Because the total mass of that single nucleus is less than the mass of the two original nuclei, the leftover mass is energy that is released in the process, according to the Department of Energy.
In the case of the sun, its intense heat — millions of degrees Celsius — and the pressure exerted by its gravity allow atoms that would otherwise repel each other to fuse.
Scientists have long understood how nuclear fusion has worked and have been trying to duplicate the process on Earth as far back as the 1930s. Current efforts focus on fusing a pair of hydrogen isotopes — deuterium and tritium — according to the Department of Energy, which says that particular combination releases “much more energy than most fusion reactions” and requires less heat to do so.
Daniel Kammen, a professor of energy and society at the University of California at Berkeley, said nuclear fusion offers the possibility of “basically unlimited” fuel if the technology can be made commercially viable. The elements needed are available in seawater.
It’s also a process that doesn’t produce the radioactive waste of nuclear fission, Kammen said.
Crossing the line of net energy gain marks a major achievement, said Carolyn Kuranz, a University of Michigan professor and experimental plasma physicist.
“Of course, now people are thinking, well, how do we go to 10 times more or 100 times more? There’s always some next step,” Kuranz said. “But I think that’s a clear line of, yes, we have achieved ignition in the laboratory.”
One way scientists have tried to recreate nuclear fusion involves what’s called a tokamak — a doughnut-shaped vacuum chamber that uses powerful magnets to turn fuel into a superheated plasma (between 150 million and 300 million degrees Celsius) where fusion may occur.
The Livermore lab uses a different technique, with researchers firing a 192-beam laser at a small capsule filled with deuterium-tritium fuel. The lab reported that an August 2021 test produced 1.35 megajoules of fusion energy — about 70% of the energy fired at the target. The lab said several subsequent experiments showed declining results, but researchers believed they had identified ways to improve the quality of the fuel capsule and the lasers’ symmetry.
It takes more than extreme heat and pressure. It also takes precision. The energy from the lasers must be applied precisely to counteract the outward force of the fusion fuel, according to Stephanie Diem, an engineering physics professor at the University of Wisconsin–Madison.
And that’s just to prove net energy gain is possible. It’s even harder to produce electricity in a power plant.
For example, the lab’s lasers can only fire a few times a day. To viably produce energy, they would need to fire rapidly and capsules would need to be inserted multiple times a minute, or even faster, Kuranz said.
Another challenge is to increase efficiency, said Jeremy Chittenden, a professor at Imperial College in London specializing in plasma physics. The lasers used at Livermore require a lot of electrical energy, and researchers need to figure out a way to reproduce their results in a much more cost-effective way, he said.

This handout picture made available by the World Health Organization (WHO) shows WHO Director-General Tedros Adhanom Ghebreyesus delivering remarks following the speech of US President’s chief medical adviser during a World Health Organization (WHO) executive board meeting on January 21, 2021 in Geneva. – In a dramatic about-turn, the new US administration on January 21, 2021 thanked the World Health Organization for leading the global pandemic response and vowed to remain a member. “The United States also intends to fulfil its financial obligations to the organisation,” top US scientist Anthony Fauci, who has been named President Joe Biden’s chief medical adviser, told a meeting of the WHO’s executive board. (Photo by Christopher Black / World Health Organization / AFP) / RESTRICTED TO EDITORIAL USE – MANDATORY CREDIT “AFP PHOTO/ CHRIS BLACK/ WORLD HEALTH ORGANIZATION” – NO MARKETING – NO ADVERTISING CAMPAIGNS – DISTRIBUTED AS A SERVICE TO CLIENTS
Geneva: At a time when fear looms over China for a bigger COVID-19 outbreak during the January Lunar New Year travel rush, the World Health Organization (WHO) head Tedros Adhanom Ghebreyesus on Wednesday called on the Asian nation to share the requested data concerning Covid-19 in a bid to understand the origins of the deadly coronavirus.
Addressing a media briefing, the WHO chief said, “We continue to call on China to share the data and conduct the studies that we have requested, to better understand the origins of this virus. As I have said many times, all hypotheses remain on the table.”
Three years after its emergence in China’s Wuhan, exactly how SARS-CoV-2 first emerged as a respiratory pathogen capable of sustained human-to-human transmission remains the subject of active debate.
Experts have put forward two dominant theories on the origins of the virus. The first theory is that SARS-CoV-2 is the result of a natural zoonotic spillover. The second theory is that the virus infected humans as a consequence of a research-related incident.
According to Reuters, a WHO body meets every few months to decide whether the new coronavirus has killed over 6.6 million people, still presents a “public health emergency of international concern” (PHEIC).
The WHO chief said that he is “hopeful” that the COVID-19 pandemic will no longer be considered a global health emergency next year. “We’re hopeful that at some point next year, we will be able to say that COVID-19 is no longer a global health emergency,” the WHO chief told a media briefing, as quoted in a statement on the organization’s website.
He recalled that one year ago, the Omicron variant “had just been identified and was starting to take off.”
“At that time, COVID-19 was killing 50,000 people each week. Last week, less than 10,000 people lost their lives globally. That’s still 10,000 too many – and there is still a lot that all countries can do to save lives – but we have come a long way,” he added.
The WHO head said the criteria for declaring an end to the emergency will be discussed during the next meeting of the Emergency Committee in January. He added that the virus “will not go away,” but all countries “will need to learn to manage it alongside other respiratory illnesses including influenza and RSV, both of which are now circulating intensely in many countries.”