
Long-COVID can lead to a variety of brain and personality-altering symptoms.
Published in 2022, a PLOS ONE research study performed longitudinal assessments of personality changes in 7,109 Americans, aged 18 to 109, during the COVID-19 pandemic.
It is reported that, compared to the pre-pandemic period, people became less extroverted, open, agreeable, or conscientious. What is more astonishing is that these changes were equivalent to about one decade of normative personality change if occurring during a non-COVID period.
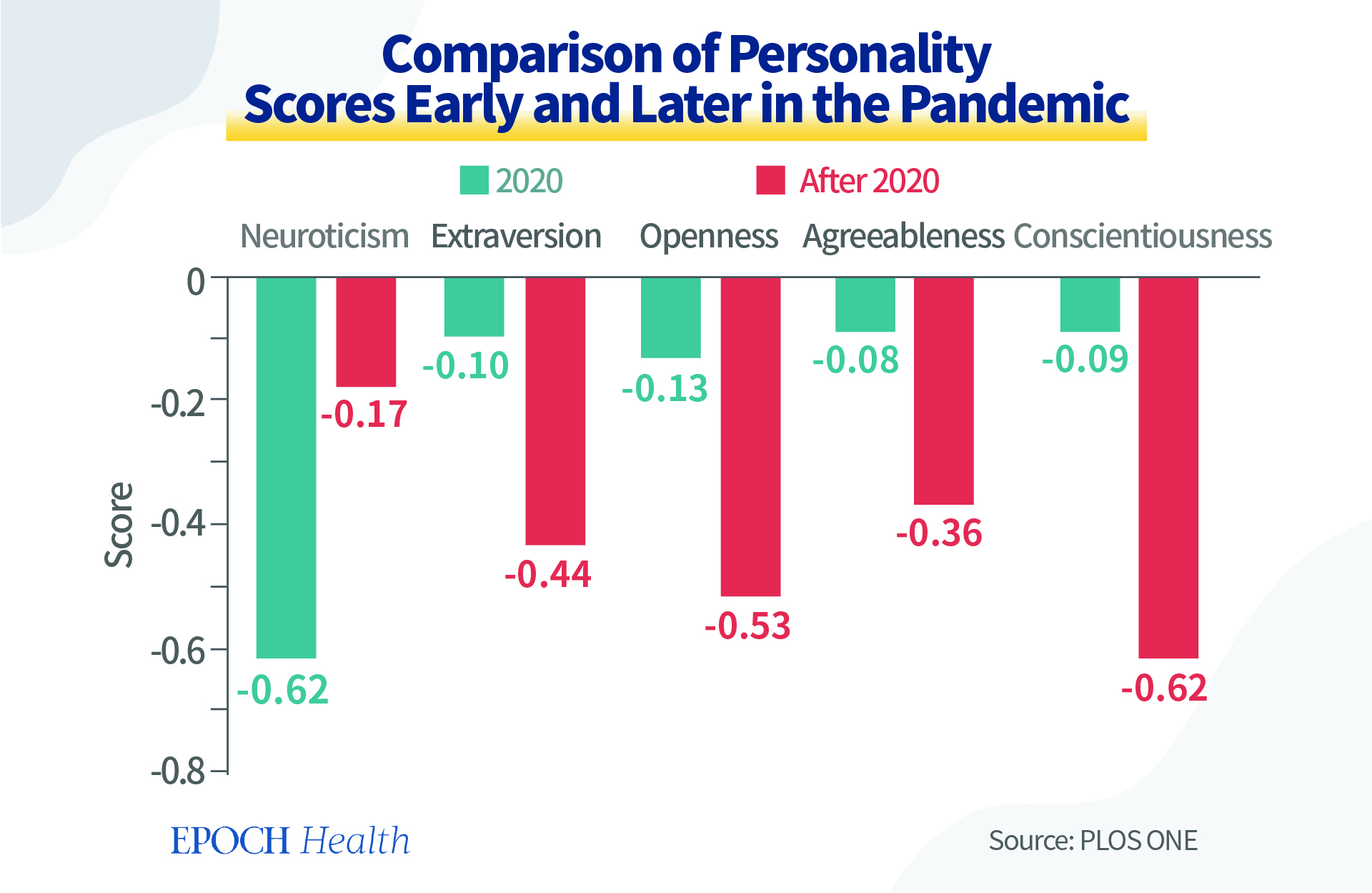
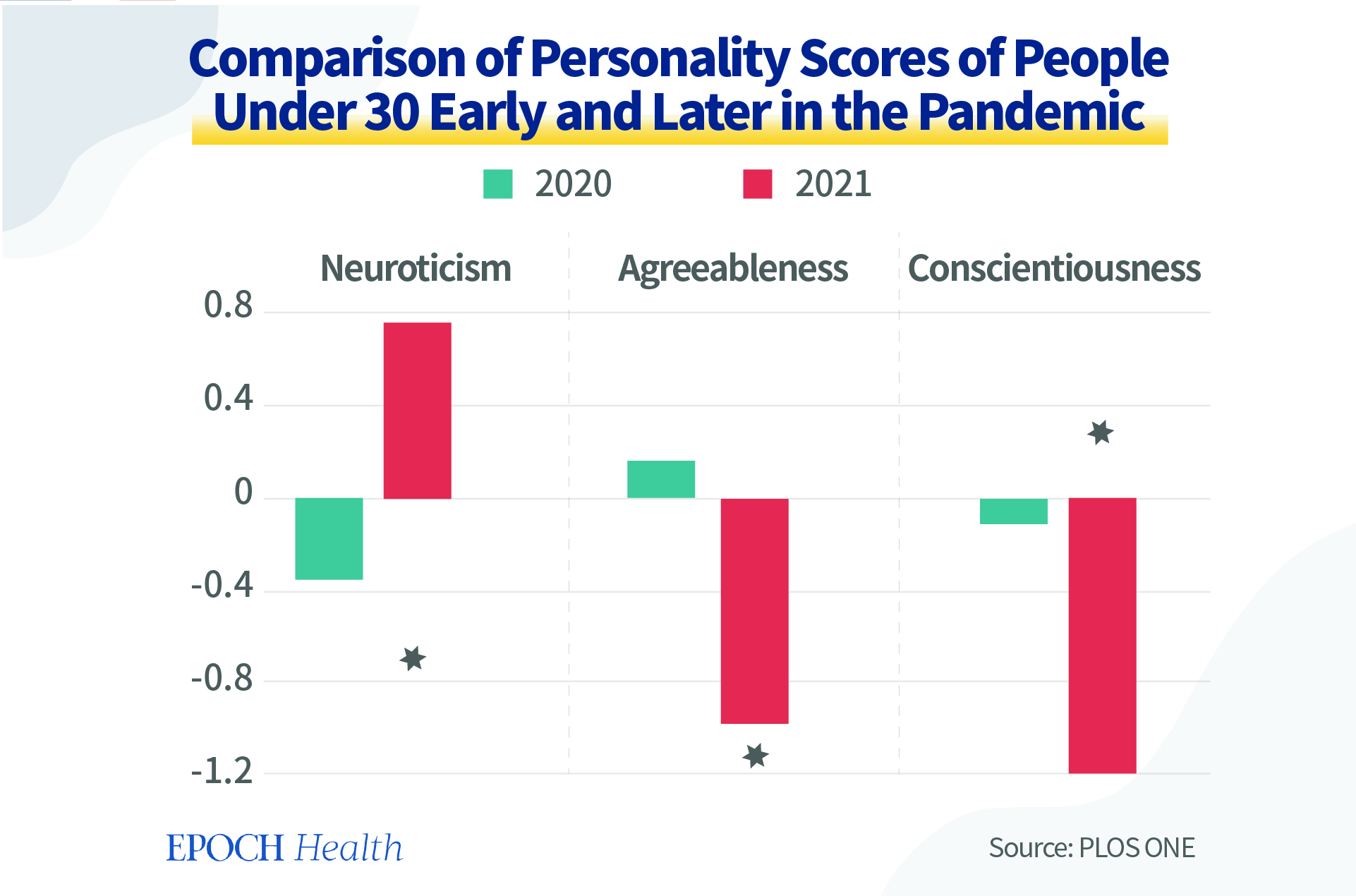
Strikingly, younger adults showed disrupted maturity by a significant increase in neuroticism and a significant decline in agreeableness and conscientiousness.
The 5 Factors of Personality Traits
Personality is the solidified reaction mode of one’s thoughts, emotions, and actions. As people mature, their personality is relatively stable regardless of the environmental simulations.
There are many classification systems for personalities. The five-trait personality system was defined by five factors: namely, Openness, Conscientiousness, Extraversion, Agreeableness, and Neuroticism (OCEAN).
Openness is the likelihood of being creative and unconventional.
Conscientiousness describes a person’s qualities of organization, discipline, and responsibility.
Extraversion is not only the level of a person’s likelihood to interact with others but also indicates the main source of one’s energy.
Agreeableness refers to whether a person is empathetic, helpful, and friendly.
Neuroticism measures if someone is inclined to experience negative emotions and is vulnerable to stress.
In summary, except for neuroticism, the higher scores indicate positivity and maturity. As a person ages, the scores should be higher. For neuroticism, a low score is more desirable.
Reasons for the Decreased Personality Scores During the Pandemic
The research did not provide data for the COVID infection and vaccination. We would like to discuss potential contributory factors causing these personality changes.
First, if people were infected by COVID-19, the SARS-CoV-2 virus itself has been proven to change one’s brain structure. This research found that those infected with SARS-CoV-2 experienced cognitive deficits equivalent to about 20 years of aging.
A study found that COVID-19 can cause neurological and psychiatric issues, such as brain fog, anxiety, and depression. People experienced higher risks of developing memory loss or inability to think coherently for as long as two years.
Long-COVID can lead to a variety of brain and personality-altering symptoms. These include traumatic brain injury and neurodegenerative conditions such as Parkinson’s and Alzheimer’s. It can change the way that people experience, interpret, and understand the world; it can make emotions unstable.
COVID-19 inflammatory cytokine storms trigger an uncontrolled immune response that may permanently destroy brain cells.
The National Geographic magazine reported a case in early 2020. Lorna Breen, a respected 49-year-old New York emergency room physician and former medical director of New York-Presbyterian Allen Hospital in Manhattan, was considered brilliant and energetic with no history of mental illness. After she was infected with the virus, Breen became confused and hesitant. She had to be hospitalized in a psychiatric ward. Shortly after discharge, Breen committed suicide.
Secondly, long-lasting emotional stress can alter one’s immune system. Even without the virus, persistent stress can affect physical health.
Similar to viruses inducing changes in our immune system, the body reacts to emotions as strongly as immune cells react to antigens. Invisible, persistent emotions can cause persistent, chronic inflammation, so as to affect people’s personalities.
Robert Ader, professor of psychiatry at the University of Rochester Medical Center and founder of psychoneuroimmunology, proposed a theory that the human mind can influence the immune system’s ability to fight disease.
Our immune system is very responsive to our emotions, thoughts, and beliefs. These factors dictate whether or not we will get sick. This is the direct manifestation of the mind-body connection.
The connection is mediated via multiple “currencies,” such as neurotransmitters, hormones, and cytokines produced by immune cells (e.g., interleukins, Tumor Necrosis Factor).
A study published in 1996 in Psychosomatic Medicine conducted a classic psychological test. One group of 79 healthy people was asked to speak publicly in front of an audience to produce a kind of social fear. Another group of 30 healthy people was asked to speak privately.
Half of the people being tested were male and half were female. The average age was 20 to 23. They were college freshmen and majored in psychology. Two tests were done after the public speech. One test had a recovery stage and the other one had no recovery stage.
The result showed that the social fear induced by public speaking caused hypertension and increased heartbeat.
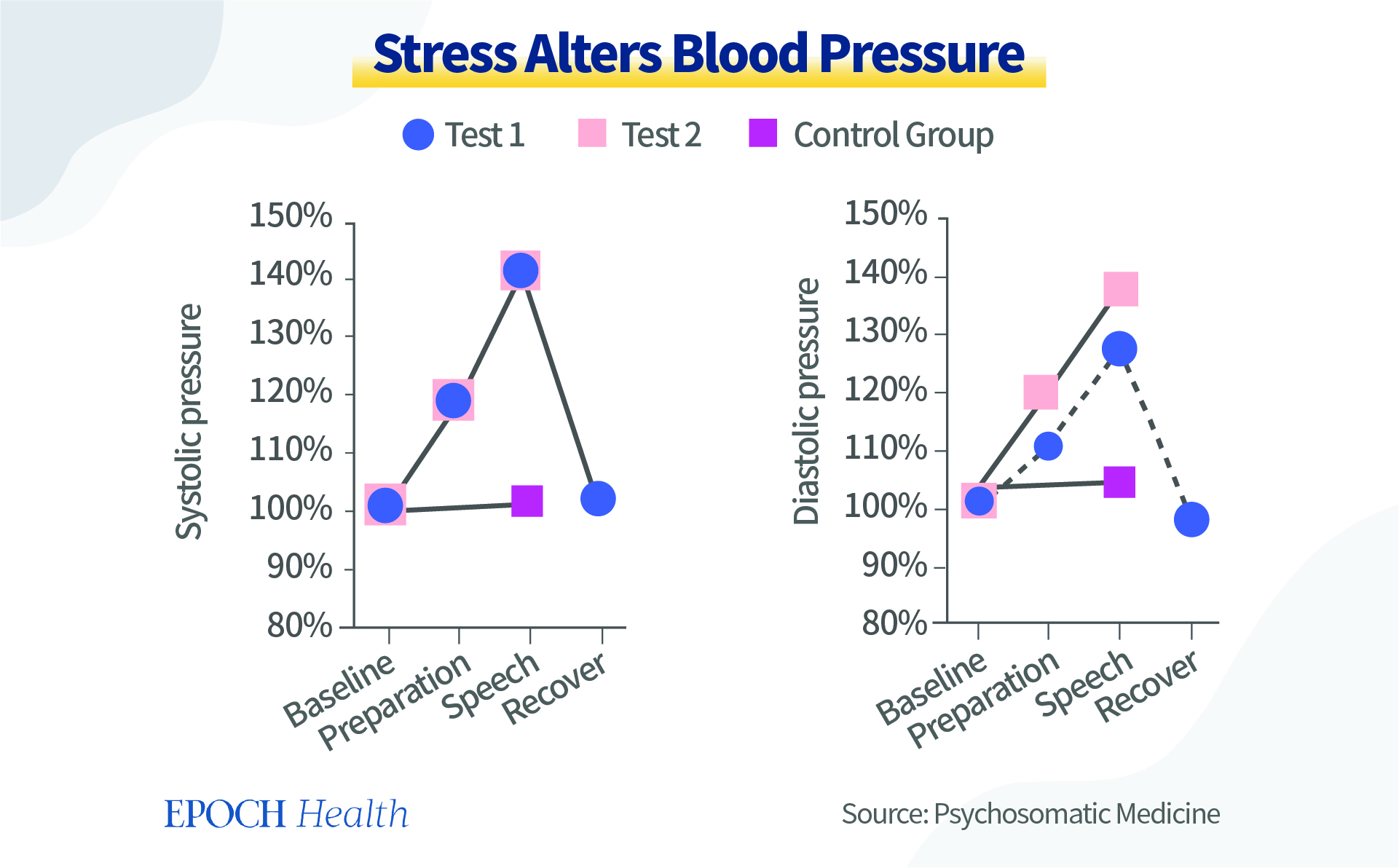
Levels of cortisol, the stress hormone, are also elevated during stress. When cortisol is elevated, immunity is affected accordingly.
During the time from 9 a.m. to noon, when the experiment was done, normally there should be a steady decline in the stress hormone level. And indeed, for the control group, it decreased by 25 percent. But in the experimental group, it did not decline but increased by five percent.
The tension brought on by short-term stress affects blood pressure and heart rate through the sympathetic-adrenal glands and affects the immune system through stress hormones. It can also affect or even change the functional state of the brain’s immune cells, the way they respond to external stimuli, and thus influence personality changes.
This study found that repeated social defeat stress caused the increase of pro-inflammatory cytokines in adult male rats.
Even though the cytokines themselves are too big to enter the brain, the signal from the cytokines can reach the brain and affect the function of immune cells in the nervous system, thus worsening the chronic inflammation of the nervous system, and resulting in a vicious cycle.
When the brain is in a persistent inflammation state, it can change a person’s mental state and eventually lead to personality changes.
When Under Stress, Rationality Is Better Than Venting
Many people are used to letting out their negative emotions when under stress.
Because stress and depression are also substances, if they accumulate inside our body too much, these negative substances make us feel uncomfortable and our body naturally wants to get rid of them.
Releasing emotions is our natural reaction, but it is not necessarily rational and does not necessarily solve the issue, either.
The difference between human beings and other forms of life is that humans have rationality. There are rational ways to remove negative emotions. When you feel angry or frustrated, try the following tips first:
- Take a break: Stop talking, and walk away from the situation that makes us angry.
- Try a few simple movements, take a deep breath, or hold a fist.
- Find a quiet place and talk to yourself by heart: “What happened? Are my negative feelings helpful to the situation? Can it really help solve the problem? What’s the source of my negative emotion? What should I do to fundamentally solve the problem?”
Forest Therapy Has Positive Effect on All Scores
Our minds and spirit are made of microscopic substances. If we want to improve the level of our mental health, we should nourish our minds or spirit with an equivalent level of substances.
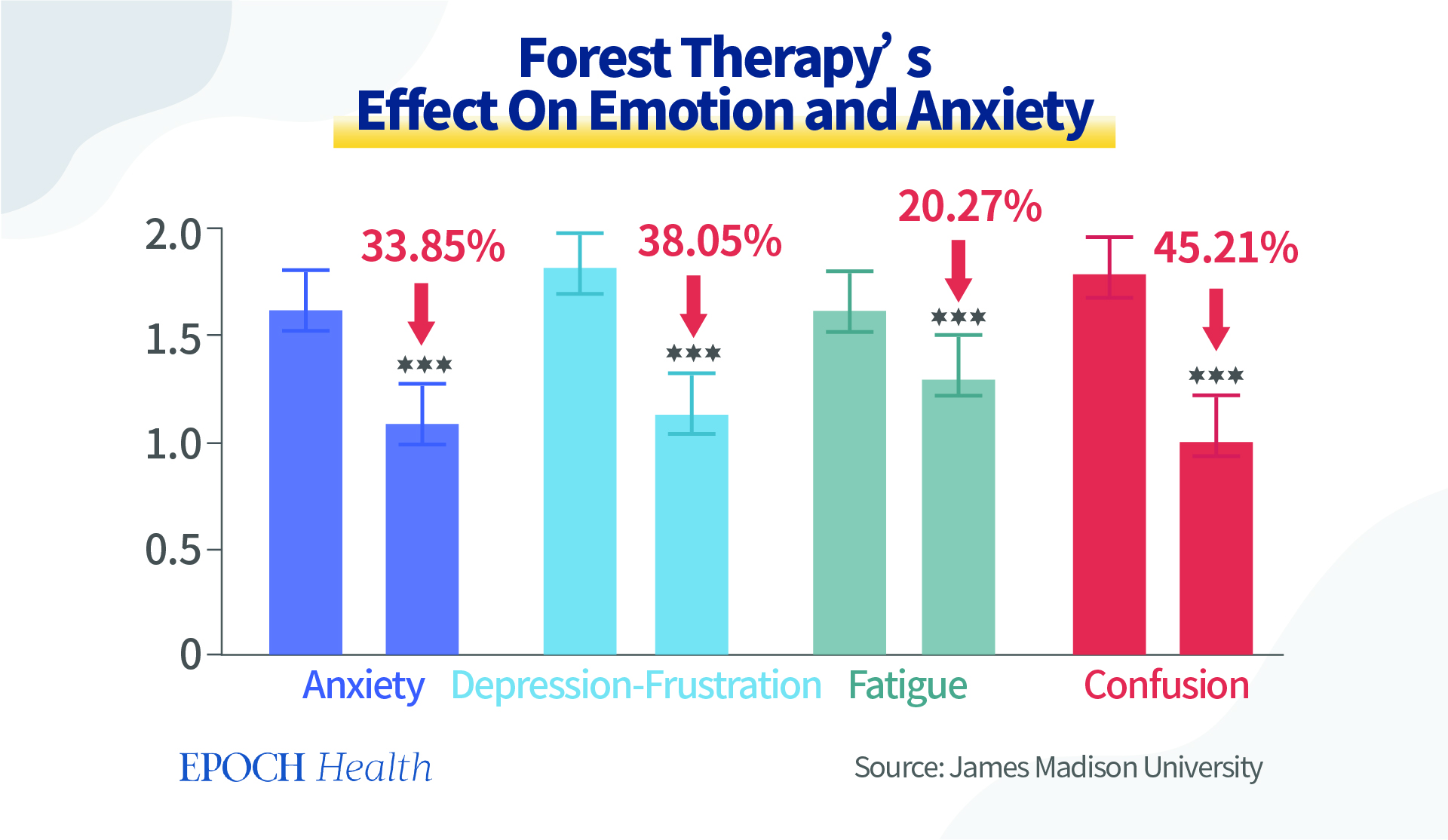
In the summer and fall of 2018, in a psychiatric hospital in northern Poland, forest therapy was practiced by walking in the forest for one hour and 45 minutes, accompanied by a therapist.
Forest therapy had a positive effect on almost all scores, with the greatest improvement in “Confusion” and “Depression-Frustration.” Anxiety or tension also decreased significantly. Vitality improved by 40 percent. No significant change was seen in the “Anger – Hostility” score.
We’ve mentioned before that horticultural therapy lowers cortisol levels, and reduces stress and negative emotions.
One of the theories to explain the effects of forest therapy and horticultural therapy is that the energy field of plants could nourish the positive energy level of our human mind and spirit.
Light Therapy and Photobiomodulation Improves SAD
For some people, mood changes come with the change of seasons, called seasonal affective disorder (SAD).
When the days become shorter in the fall and winter (called “winter blues”), one may begin to feel “down” and start to feel better in the spring. The symptoms include sleep disorders or oversleeping, overeating, weight gain, social withdrawal, anxiety, and violence.
Bright light therapy (BLT) is recognized as a first-line therapy for SAD. For this treatment, patients sit in front of a very bright light box for 30 minutes to two hours a day, usually first thing in the morning, from fall to spring.
Two meta-analyses of eight randomized blind and controlled studies (n=703 total) were consistent in demonstrating that BLT showed efficacy in the treatment of SAD when compared to a control condition.
In a placebo-controlled study, the majority of patients with SAD (61 percent of 33 patients) who received bright light therapy during the four-week study period reached symptom remission versus only 32 percent of the 31 patients receiving the placebo who achieved remission during the study, and the difference was statistically significant (p<0.05).
Thus, BLT is proven not only to be an effective treatment for SAD but also powerful enough to bring patients with depression into remission.
Since the destructive UV rays are filtered out, it is relatively safe for most people. However, people with certain eye conditions or those taking certain medications that increase sensitivity to sunlight may need to be careful.
Psychological therapy, antidepressant therapy, and vitamin D can also be used in a combined way.
Ordinarily, people can simply rely on sunlight. Sunny weather makes one feel better. Sunlight enters the hypothalamus, where our pineal gland secretes melatonin, serotonin, and dopamine, improving day and night rhythms, boosting energy, elevating mood, and improving sleep.
There is always more sunlight outdoors than indoors, even if it’s a cloudy day.
Scientific reasons for beneficial health effects associated with sunlight could perhaps be explained by photobiomodulation (PBM), by infrared and near-infrared light from sunlight.
Infrared and near-infrared (NIR) radiation has profound effects on human physiology, especially as a mitochondrial stimulant, which increases ATP—cellular energy production; enhances the activity of cytochrome c oxidase as part of the mitochondrial respiratory chain; reduces lung inflammation; improves cell survival; causing reduction of TLR-4 dependent inflammatory response pathway.
As most of these pathological patterns have been manifested in SARS-CoV-2 infection, accordingly, PBM has been suggested as a potential method for the treatment and prevention of COVID-19.
Furthermore, transcranial PBM has beneficial effects on a range of neuropsychiatric diseases, including depression and anxiety, Alzheimer’s disease, Parkinson’s disease, stroke, and traumatic brain injury.
Of all the waves in sunlight, near-infrared radiation (NIR-A), in the power range of 10 to 15 W at 810 and 980 nm, can be biologically beneficial at 3 cm depth.
Since 2020, COVID-19 has caused far-reaching negative effects on humans at physical, mental, and spiritual levels. It could even worsen our personality regardless of whether we are infected by the virus directly or not.
The shocking impact of personality decline by more than 10 years during the COVID pandemic is enough for us to reflect on the current measures that we have taken to prevent or treat COVID-19.
Humans are holistic beings of the physical body, mind, and spirit. To heal the trauma in our personality level, we must turn to the natural ways again—embrace the trees and enjoy the sunlight. Nature is a great source of enormous healing power.













