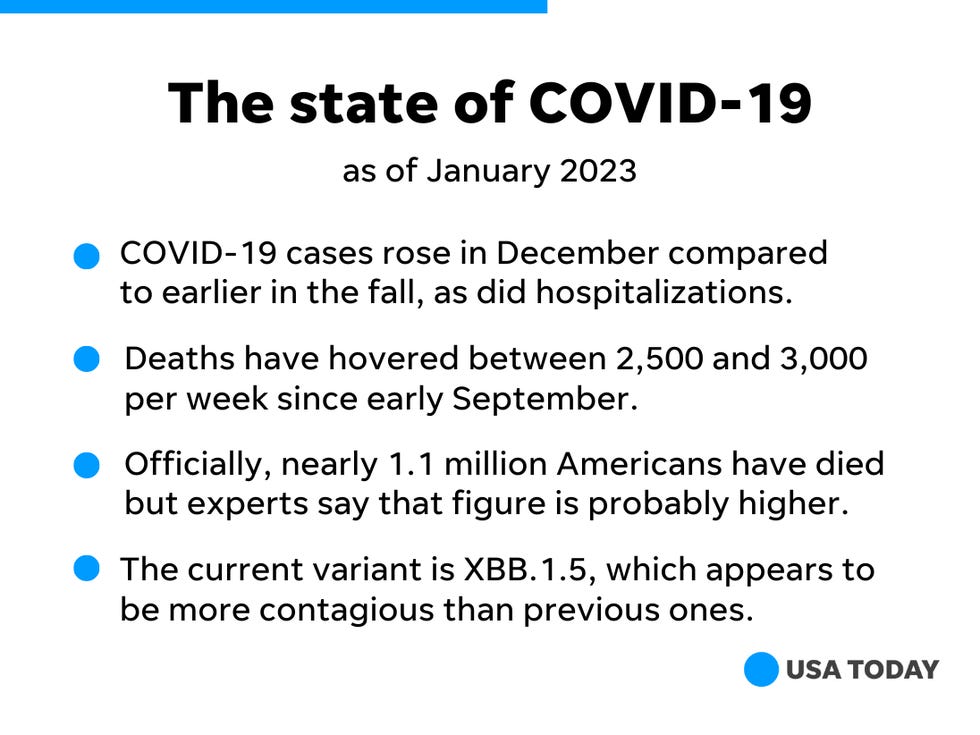
What is XBB.1.5?
XBB.1.5 is yet another omicron subvariant, and follows on from XBB and XBB.1. Scientists have nicknamed it “kraken” to distinguish it from the “variant soup” we are all navigating three years into the pandemic.1 The X signifies that these subvariants came about through a recombination of two or more sublineages—in this case BA.2.10.1 and BA.2.75.2
According to UCL Genetics Institute director Francois Balloux, a professor of computational systems biology, XBB.1.5 differs from XBB.1 through the addition of a F486P mutation in the spike protein. “This mutation makes it slightly less immune evasive than its XBB.1 ancestor but more infectious, probably because it increases binding affinity to the human cell receptor ACE-2,” he said.
Where is XBB.1.5 spreading?
The World Health Organization has reported that XBB.1.5 is present in 38 countries.3
The UK Health Security Agency (UKHSA) said it is one of two variants most likely to become dominant in the UK, despite representing less than 5% of all SARS-CoV-2 samples sequenced in the last week of 2022. The agency has described the variant as having a combination of “immune escape properties” and a higher ACE-2 binding affinity, which it said could lead to higher transmissibility. “It is plausible that XBB.1.5 will cause an increase in incidence after the current wave, however it is currently too early to confirm this trajectory,” UKHSA said.4
Meanwhile, the European Centre for Disease Prevention and Control (ECDC) has said there is a “moderate probability” that XBB.1.5 will become dominant across the European Union and European Economic Area and cause a “substantial increase in the number of covid-19 cases within the next one to two months.”
In the US the Centers for Disease Control and Prevention has said the variant is “spreading quickly” and is estimated to make up around 28% of cases in the country (week ending 7 January 2023).
“XBB.1.5 is widely anticipated to go up in frequency globally, and may cause a sizeable fraction of cases globally in the near future,” Balloux said. “That said, it remains questionable whether XBB.1.5 will cause a major wave on its own.”
Does it cause more severe illness?
This is still under review. According to WHO, however, XBB.1.5 “does not carry any mutation known to be associated with potential change in severity.” This appears to be supported by the ECDC, which said that there are no indications that XBB.1.5 will be any more severe than the other omicron sublineages that have circulated.
Do the current covid vaccines protect against XBB.1.5?
Specific vaccine effectiveness estimates are not yet available for XBB.1.5, but WHO has warned that it may have the “highest immune escape to date.” Its evidence suggests people who have had three or four doses of an mRNA covid-19 vaccine (such as Moderna or Pfizer) plus a BA.5 infection, or three doses of the Chinese Coronavac vaccine plus previous infection with BA.1, BA.5, or BF.7 “do not induce high neutralisation titers against XBB.1.5.5.”
The ECDC has also warned that its predecessors—XBB and XBB.1—showed “significant reductions in the neutralising capacity of serum from vaccinated people.” Despite this, the agency has said the available vaccines “still remain effective against severe disease because of previous and current omicron variants dominant in the EU, even though there is some evidence of waning over time.”5
It is not yet clear whether an XBB-specific booster vaccine could be needed, but experts have called on those eligible to get available booster vaccines where possible.
Is XBB.1.5 a cause for concern?
While much of the evidence surrounding XBB.1.5 is still being collected and reviewed, experts have said there is currently no need to be alarmed by this variant.
Ashall professor of infection and immunity at the University of Oxford Andrew Pollard, who led the team that developed the Oxford AstraZeneca vaccine, told The BMJ, “We should be cautious not to drive fear that each new variant heralds a new crisis in the pandemic. There is no reason to think that XBB.1.5 is of any more concern than other variants that come and go in the ever changing landscape of covid-19 mutants.”
Pollard said that, in the UK at least, the focus needs to be on ensuring the healthcare system can cope with not just covid-19, but all patients.
“In the UK today, the problem is not new infections with covid-19, which is just one of many non-pandemic viruses that make us sick, but the chronic shortage of capacity, funding, and staff in our health and social care system. We have to plan for expected winter pressures from infections and need to develop the resources to accommodate a growing elderly population over the decades ahead,” he said. “These are not easy problems to solve but, unlike pandemics, they are not easily solved by leaps in science or short term fixes but by a long term vision for our health shared across the political divide.”