Abstract
Background
Glioblastoma multiforme (GBM) is the most aggressive primary brain tumor with poor prognosis. GMB are highly recurrent mainly because of radio- and chemoresistance. Radiotherapy with Temozolomide (TMZ) is until today the golden standard adjuvant therapy, however, the optimal treatment of recurrent glioblastoma remains controversial. Ouabain belongs to the Cardiotonic Steroids (CTS) the natural ligands of the Na/K-ATPase (NKA). It is established that the NKA represents a signal transducer with either stimulating or inhibiting cell growth, apoptosis, migration and angiogenesis. Over the last decade evidence grew that CTS have anti-tumor properties especially in GBM.
Discussion
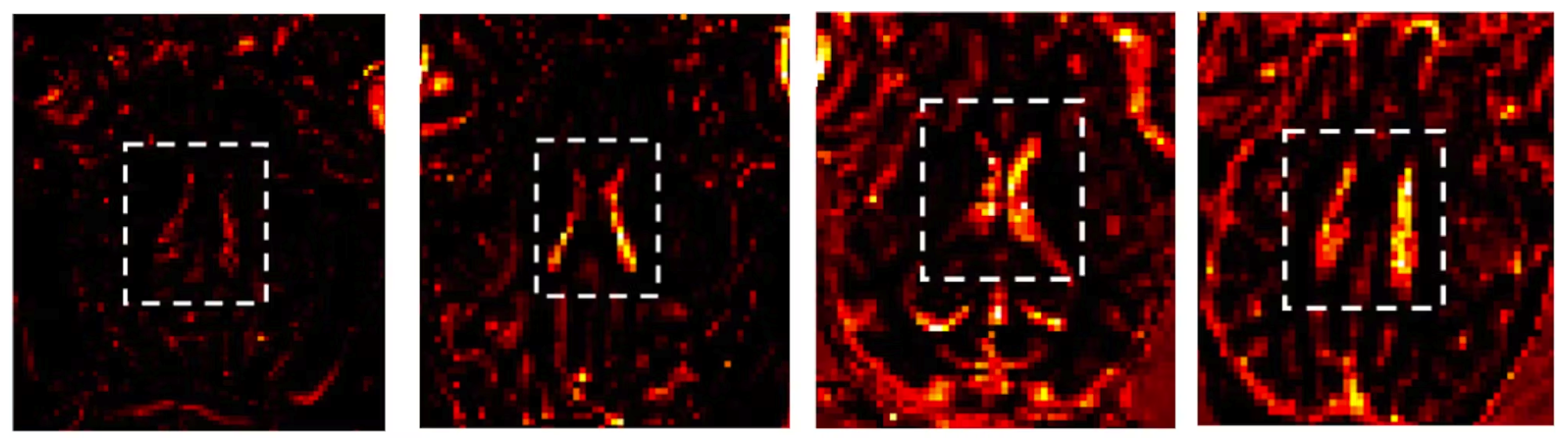
The results show that with regard to cell migration as well as plasma cell membrane depolarization Ouabain indeed has different effects on the two GBM cell lines, the TMZ-sensitive LN229 and the TMZ-resistant T98G cell line, similar to the results found by the group of Chen and coworkers with respect to apoptosis [46]. The authors showed that in T98G cells apoptosis was induced at significantly lower Ouabain concentrations (0.1 μM) as compared to LN229 cells (> 1 µM). However, in our setting, LN229 cells did not show any reaction to Ouabain neither in the migration assay nor in the cell membrane potential assay, even at higher concentrations (> 10 µM). For this discrepancy we do not have a plausible explanation and further studies are needed.
In contrast, the TMZ-resistant cell line T98G showed a marked inhibition of migration at rather low doses of Ouabain (0.01–0.1 µM), which correlated significantly with an increase in cell membrane depolarization (p = 0.002). A similar opposite reaction pattern to Ouabain was observed in the LN229 and T98G cells in the Bcl-2 analysis i.e., only in the T98G cell line we saw a down-regulation whereas LN229 did not show any reaction. The fact, that the Bcl-2 down-regulation was detected only at very low Ouabain concentrations (0.01 nM) must be interpreted with caution, we will discuss this issue further down. In summary, while the TMZ-resistant T98G cell line is sensitive to Ouabain, the TMZ-sensitive LNN29 cell line seems to be resistant to Ouabain.
Interestingly, migrating GBM cells are per se resistant to apoptosis. Joy and coworkers revealed an activation of the phosphoinositide 3-kinase (PI3-K) survival pathway by migrating glioma cells, which renders them resistant to apoptosis [68]. Applying a specific inhibitor of PI3-K (LY294002) to migrating cells the phosphorylation of Akt was inhibited and consequently, an increased rate of apoptosis was seen. Yang and coworkers could demonstrate that Ouabain is able to prevent phosphorylation of Akt and mTOR, inhibiting cell migration and enhancing apoptosis [47]. Lefranc and coworkers also stressed the importance of an inverse relationship between migration and apoptosis in GBM and the key role of the PI3-K/Akt pathway [69].
The fact that the T98G cells reacted to the cell migration assay as well as to the plasma cell membrane potential assay at similar Ouabain concentrations strongly indicates a causal relationship between migration inhibition, depolarization of the cell membrane, and consequent induction of apoptosis.
Many authors described a correlation between plasma cell membrane (PCM) depolarization and early apoptosis, but it is not fully clear whether it constitutes a causal relationship or a mere epiphenomenon. There is evidence that PCM depolarization is a prerequisite for apoptosis. Suzuki-Karasaki and coworkers described the disruption of intracellular K + and Na + concentrations as a basic important event leading to depolarization, cell shrinkage, and hence apoptosis [70]. Bortner and coworkers reported in Jurkat T-cells a PCM depolarization immediately after application of diverse apoptotic stimuli (anti-Fas antibody, thapsigargin and the calcium ionophore A23187) followed by cell shrinkage [71]. Moreover, an early increase in intracellular Na + as well as inhibition of K + uptake was observed in response to anti-Fas, indicating an inactivation of the Na + /K + -ATPase. Interestingly, Ouabain enhanced anti-Fas-induced apoptosis. Finally, applying an anti-apoptotic signal, i.e., protein kinase C, did not only inhibit apoptosis but also prevent cell membrane depolarization in response to anti-Fas. Thus, the authors concluded that cell membrane depolarization per se is a crucial early step in anti-Fas-induced apoptosis [71].
Interestingly, the PCM depolarization was not a short-lasting phenomenon, as known from electrically excitable cells, but rather was sustained. We also saw in the T98G cell line over time (up to 6 h) a sustained PCM depolarization. This sustained PCM depolarization is an indication that upon apoptotic stimulation, the cells lose their ability to repolarize.
At this point it is important to mention the role of Bcl-2, the classic anti-apoptotic protein of the Bcl-2 family [72]. Usually, they are localized at the outer mitochondrial membrane, but recent studies discovered intracellular truncated forms in the neighborhood of the plasma cell membrane [73]. The most known function of Bcl-2 is exerted by inhibiting the oligomerization of Bcl-2-associated X protein (BAX) and Bcl-2-associated agonist of cell death protein (BAD) hereby preventing their pro-apoptotic effect.
But already decades ago the importance of Bcl-2 in modulating the plasma cell membrane has been stressed. We mentioned above the works of Gilbert and coworkers who observed that overexpression of the anti-apoptotic Bcl-2 gene is associated with membrane hyperpolarization rendering cells more resistant to radiation-induced apoptosis [61]. Further studies revealed that Bcl-2 itself has pore-forming domains similar to that of bacteria toxins and that the activation of K + channels by the myeloid leukemia cell differentiation protein (Mcl-1), a member of the Bcl-2 family, results in plasma cell membrane hyperpolarization [59, 74]. Finally, Lauf and coworkers could demonstrate a direct co-localization of Bcl-2 specifically with the NKA in the cell membrane providing the missing link to the hypothesized interaction between Bcl-2 and NKA [63].
The numerous functions of Ouabain on intracellular pathways are well described; one of them is the down-regulation of Bcl-2/Mcl-1 by accelerating its proteasomal degradation via reactive oxygen species (ROS) generation [75].
So, it seems, that Ouabain can not only depolarize the plasma cell membrane directly by inhibiting the NKA but additionally by down-regulating Bcl-2. We saw only in the TMZ-resistant T98G cell line a Bcl-2 down-regulation after treatment with Ouabain for 24 h at very low concentrations (0.01 nM) which unfortunately did not correlate with the concentrations, at which we observed PCM depolarization and cell migration inhibition. Consequently, in our study we could not confirm that Bcl-2 down-regulation contributes to PCM depolarization.
But with caution, we may interpret the down-regulation of Bcl-2 as a kind of sensitizing effect to facilitate e.g., apoptosis. Only recently, a Bcl-2 effect on cell migration was discovered [76,77,78]. In Fig. 1b we see a slight inhibitory effect of Ouabain on cell migration at very low (≤ 0.01 nM) concentrations which correlates exactly with those of Bcl-2 down-regulation (Fig. 5). As we outlined above, inhibition of cell migration is a prerequisite to apoptosis. Additional studies in future are needed and may focus not only on Bcl-2 but also on Mcl-1 expression [61, 63]. Interestingly, Wang and coworkers demonstrated that Mcl-1 causes a hyperpolarization of the PCMP through activation of K + channel activity [59] hereby preventing apoptosis.
At this point it should be stressed that Ouabain is known to have significant effects at nanomolar concentrations [56], e.g., at 0.1 to 10 nM the NKA is stimulated in non-malignant (cardiac and neuronal) cells, interestingly, via the high glycoside affinity α3 isoform [79].
As outlined above the PI3-K/Akt pathway is one important modulator of cell migration. We revealed in T98G cells an increase in p-Akt after 24 h treatment with 0.1 µM Ouabain. In contrast, LN229 cells did not show any change in p-Akt. It contradicts the anti-migratory effect of Ouabain which we revealed at 0.1 µM in T98G cells. In fact, we expected a p-Akt down-regulation, at least after prolonged 24 h treatment similar to Chen and coworkers, who observed a p-Akt down-regulation at 2.5 µM Ouabain in U-87 GBM cells [46].
The significant decreased level of pan-Akt after 24 h Ouabain treatment at 1 µM hints to a different mechanism by which Ouabain exerts its antitumor effects. You and coworkers were concerned about the short-lasting effects of phosphorylation inhibitors and developed a pan-AKT degrader by conjugating the Akt-phosphorylation inhibitor GDC-0068 to Lenalidomide. He showed that this compound (INY-03–041) induced significant degradation of all Akt isoforms at 24 h and, interestingly, improved the anti-proliferative effects compared to GDC-0068 alone [80].
Ouabain is known to contribute to degradation of several compounds in the signalosome by internalization and disturbed intracellular trafficking [81, 82]. With specific respect to the epidermal growth factor receptor (EGFR) Hafner and coworkers described in lung cancer A549 cells a specific phenomenon called endosomal arrest. After treatment with Ouabain, Digoxin, or Acovenoside they revealed persistent granules with internalized EGF-receptor without further degradation [83].
This endosomal arrest may be considered as a crucial checkpoint in cell biology [84] by diverting growth factors either to the recycling or the degradation pathway. In case of prolonged endosomal arrest, however, they are simply “stuck there”, losing any biological function.
We assume that pan-Akt like other compounds of the signalosome is endocytosed upon prolonged Ouabain stimulation and undergoes an endosomal arrest together with NKA α-subunits and EGFR. Indeed, it was shown that endosomal Akt is associated with the intracellular trafficking of growth factor receptor complexes and thus modifying their activity in a time and location dependent manner [85].
The peak in Akt activation (p-Akt Ser473) at prolonged lower doses of Ouabain might serve as a stimulus for inducing its degradation. Kometiani and coworkers stressed the time factor in intracellular activation processes i.e., while short term activation of ERK1/2 induced cell proliferation, sustained ERK1/2 activation resulted in increased expression of the cyclin-dependent kinase inhibitor 1 (p21Cip1) resulting in growth arrest [86]. Hence, this could be the main mechanism by which e.g., pan-Akt is down-regulated resulting in inhibition of migration and induction of apoptosis. Further studies certainly are here needed.
The reciprocal response of LN229 and T98G cells to Ouabain resp. Temozolomide is striking and may have significant clinical consequences. The underlying mechanisms are not yet known. There is evidence that Ouabain induces different endocytotic trafficking and signaling pathways according to the EGFR mutation status, the NKA isoforms [56, 87] and other not yet fully analyzed factors. Many authors described the interaction between NKA and EGFR e.g., Liu and Shapiro analyzed in the renal cell line LLC-PK1 the role of the signalosome in the process of endocytosis and demonstrated that Ouabain-stimulated endocytosis of the NKA is dependent on Caveolin-1 and Clathrin as well as the activation of c-Src, transactivation of EGFR and activation of phosphoinositide 3-kinase (PI3K). They showed that c-Src, EGFR, and the extracellular signal-regulated kinases 1 and 2 (ERK1/2) all were endocytosed along with the plasmalemmal NKA [81].
We did not analyze the NKA isoforms in our GBM cell lines but as shown by Chen and coworkers the T98G cell line is characterized by a high NKA α3/ α1 isoform ratio. He stressed that the high expression of the α3 isoform in the T98G cell line was correlating with a higher sensitivity to the apoptosis inducing effect of Ouabain [46]. Xiao and coworkers proved that the knockdown of the α3 isoform with siRNA impaired the anti-proliferative effect of Ouabain, indicating that Ouabain preferentially binds to the NKA α3 isoform [88]. Future studies are warranted to analyze the exact role of EGFR- and NKA isoform expression at the cell surface in directing ouabain-induced signaling either towards enhanced or reduced cell proliferation and migration.
Last, but not least, we could demonstrate for the first time an anti-angiogenic effect of Ouabain at low concentrations (0.01 µM) which correlated significantly with the inhibitory effect on cell migration (Fig. 7). Angiogenesis is considered as prerequisite for migration and invasion of tumor cells [89,90,91] and as such it constitutes an important target for cancer therapy, especially the hypervascularized gliomas. Bevacizumab a humanized monoclonal antibody against VEGF was approved in the treatment of recurrent GBM but, at least as monotherapy, it prolonged only the progression-free survival, but not the overall survival [92, 93]. The effect of Ouabain on angiogenesis resp. endothelial cells is rarely investigated [94, 95]. Trenti and coworkers revealed that Digitoxin in therapeutic range (1–25 nM) inhibited effectively angiogenesis via focal adhesion kinase (FAK) inhibition (51). At the same time Digitoxin as well as Ouabain protected HUVEC cells from apoptosis induced by growth factor deprivation (51). Dual actions of all CTS—dependent on cell types and dose regimen—remain a scientific and therapeutic challenge we have to accept and address in future studies.