A boundary-pushing global collaboration is betting on the power of science

This home visit in Peru was part of an international clinical trial that brought new combinations of the latest drugs to participants with drug-resistant tuberculosis. Image: Joanna Arcos/Partners In Health
This is a story about how science can fuel hope to drive away despair.
It’s about an ambitious project that, over the past decade, has brought new, patient-friendly treatments to some of the places hardest hit by the deadly global epidemic of drug-resistant tuberculosis.
It’s about how the project, called endTB, has improved tuberculosis care through a series of scientific studies while pushing the boundaries of what’s thought possible: in clinical trials, in epidemiology, and in the thinking about where you can do the science required to deliver world-class health care where it’s needed most.
Patients who have participated in these studies told doctors and researchers that when they received their TB diagnosis, they were afraid.
They spoke of having recently lost family members to the disease, of the terrible prospect of being isolated from their children for a two-year treatment plan that might not work, of being unable to care for their families, earn a living, or pursue their studies because of the rigors of the disease and of the readily available treatments.
And they spoke of how those fears turned to hope when they learned that there were new, alternative treatments available thanks to endTB, with fewer pills to take and no painful injections.
Even with a cure for TB available, the crisis continues
“TB is one of our oldest and deadliest infectious foes,” said Carole Mitnick, professor of global health and social medicine in the Blavatnik Institute at Harvard Medical School, research director of endTB, and co-principal investigator of its two clinical trials.
Each year approximately 500,000 new cases occur worldwide of multidrug-resistant tuberculosis (MDR-TB) — a form of TB that is resistant to rifampicin (also known as rifampin), one of the most important frontline drugs for curing TB.
Although effective treatments for MDR-TB do exist, over the past five years, fewer than 31 percent of people diagnosed with the disease received any treatment. Fewer than 15 percent of those who fell sick were cured.
Carole Mitnick on the power of science to help vulnerable populations beat TB.
Even among the few who do get treatment, most do not have access to regimens developed in the past decade that shorten the overall length of treatment, avoid injections, and have fewer side effects than earlier regimens. Instead, they go through a grueling course of treatment over 18 to 24 months, with thousands of pills and painful daily shots with severe side effects.
Some of the medications in these shortened regimens aren’t appropriate for all patient populations, such as children and people who are pregnant or have certain other diseases. Some of the drugs in existing regimens are in short supply. Some just don’t work in some people with TB. As a result, many patients are left without a viable treatment option.
The team at endTB is working to change this.
The project represents a partnership of Médecins Sans Frontières, Partners In Health, and Interactive Research and Development, with help from researchers and clinicians at HMS and other academic medical centers and research hubs around the world.
As part of their work with endTB, Mitnick and other HMS researchers and clinicians have played crucial roles in creating and testing new treatment regimens, developing implementation plans, building local know-how to deliver the therapies in challenging settings, and collecting and analyzing data from their studies and clinical trials.
“Our work at endTB is part of a huge transformational moment, helping us fulfill the promise of the therapeutic breakthroughs of the 21st century,” said Mitnick. “Science is one of the most powerful tools we have to end human suffering.”
Picking up where pharma leaves off
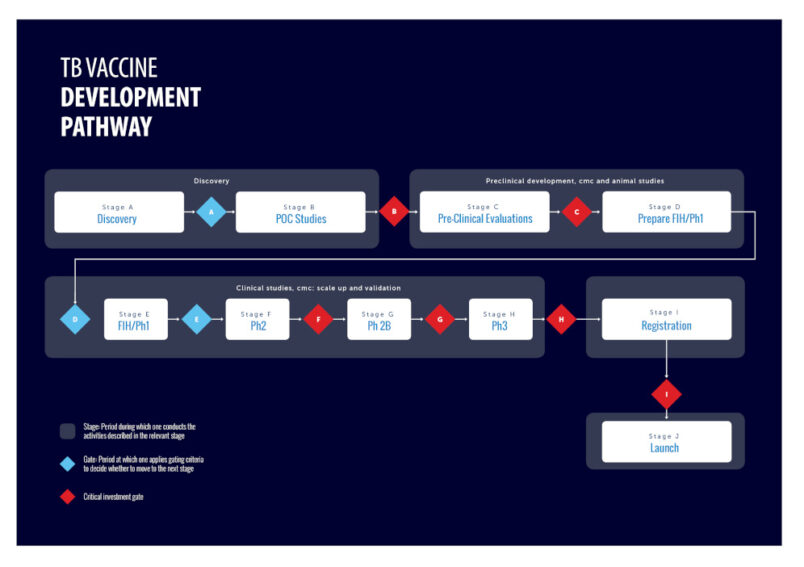
Key to endTB’s program are two phase 3 randomized clinical trials — studies conducted in many populations in different countries, often the last step before a new treatment is approved. The first tests five new MDR-TB regimens.
The treatments under study take nine months to complete instead of two years. They are all administered orally with pills, no injections needed. And they use one or two of the three new drugs developed to treat TB in the past 60 years: bedaquiline, which, in 2012, became the first U.S. Food and Drug Administration-approved drug for TB since rifampicin was approved in 1971, and delamanid, approved by the European Union in 2014.
The third drug, pretomanid, received emergency authorization from the FDA for specific use within a regimen against highly drug-resistant TB in 2019, after the endTB clinical trial was underway, and is not included in the regimens used in these trials.
The trial launched in 2017, eventually enrolling 754 patients across seven countries: Georgia, India, Kazakhstan, Lesotho, Pakistan, Peru, and South Africa.
The endTB trial fills a crucial research gap. New drugs are usually tested by the pharmaceutical companies that developed them in an effort to receive approvals so the drugs can be brought to market. Once a drug is approved, there is little incentive to conduct complex treatment programs that use combinations of new drugs developed by different companies or repurposed drugs that may be available as generic versions and can be produced by many different companies.
There is also a common misconception that it’s not possible to deliver complex care in the kinds of settings and populations where MDR-TB is most common. The endTB program was designed to address these additional challenges, including how to:
- Maximize treatment success and access while minimizing side effects and cost.
- Implement complicated research in health systems struggling to meet the clinical needs of the people they serve.
- Generate enough data about the kinds of people who are sick with the disease to understand the nuances of how the treatment works in real-world situations.
Promising progress
After completing data collection in late 2023, the endTB team reported at the Union World Conference on Lung Health that three of the five new regimens were found to be safe and effective across a population that included important subgroups: children, pregnant women, and people who were also infected with other illnesses, such as HIV and hepatitis C, common in populations with high rates of TB.

Clinical trial offers multiple new shortened drug regimens to treat adults and children with multidrug-resistant tuberculosis. Video: endTB
The team also reported that a fourth regimen, which did not perform as well as the current standard of care, might still be a valuable alternative for those patients who can’t take two key drugs found in the World Health Organization-recommended regimens for MDR-TB and in the other endTB regimens. The endTB team recommends further research on this regimen in a population that cannot take these drugs to see if it might be the first all-oral, shorter regimen treatment alternative for people with serious side effects or drug interactions that prevent them from taking the standard regimens.
The researchers noted that the regimens tested in the endTB trial could provide a much-needed complement to the shortened regimens that the WHO currently recommends. All of the individual drugs used in the endTB trial are already approved and widely available, meaning they could quickly translate into new alternatives for care in countless people with MDR-TB if the WHO recommends the regimens.
The trial data haven’t been peer-reviewed or published, so some of the details of the recommendations may change before they are finalized. The researchers said that while they are looking forward to completing the review, they felt it was important to share their initial data analysis as quickly as possible because of the potential to save lives and reduce suffering.
The best evidence possible
Over the past decade, endTB has been an important part of a new wave of scientific collaborations transforming TB treatment and research, said Molly Franke, HMS associate professor of global health and social medicine.
Investing in research in the communities that have the highest burden of TB has great potential to improve health systems and train new researchers, Franke said. Many of endTB’s research sites had never hosted any kind of study before. The endTB researchers and colleagues at other groups are running more studies that maximize the amount that can be learned from observational studies, which are often more feasible — and sometimes more ethical — to conduct than trials.
Franke was a leader of one such study: a large-scale prospective observational study with endTB that laid the groundwork for the regimens tested in the endTB clinical trial.
The study, conducted from 2015 to 2019, enrolled 2,804 participants in 17 countries on four continents, making it the largest closely followed cohort of patients receiving bedaquiline or delamanid in the world.
One of the goals of endTB is to show that it’s possible to do high-quality research in places that are struggling to control TB, Franke said.
“If you want to beat TB, you need to take the fight — and the best scientific tools in our arsenal — to where the disease is strongest,” Franke said. “Where the science leads, the cure can follow.”
Franke and colleagues continue to mine the data collected in the observational study to find evidence that can be used to improve treatment and research methods. Recently, they have optimized the length of treatment regimens that use bedaquiline and improved the methods used to estimate relapse after TB treatment. By including rigorous protocols to examine and analyze the combined side effects of all the drugs in the various regimens employed in the endTB observational study, endTB was able to demonstrate definitively that regimens containing bedaquiline, delamanid, or both are safe and well-tolerated and that the older drugs in the regimens pose greater concerns for toxicity than the new drugs.
Not the end of the story
There are no eureka moments in this story, no solitary geniuses at work alone in the lab. Instead, there are generations of researchers, clinicians, students, patients, and families working tirelessly across years to tackle a tenacious, ever-evolving microbe.
The endTB community includes veterans of many campaigns against TB.
Among them is Michael Rich, HMS assistant professor of medicine at Brigham and Women’s Hospital, who serves as senior medical officer of PIVOT, an NGO that works to strengthen health systems in rural Madagascar, and is primary author of multiple WHO guidelines on managing MDR-TB.
Another is K.J. Seung, HMS assistant professor of medicine the Division of Global Health Equity at Brigham and Women’s. Seung has worked closely with government ministries, the WHO, and community health organizations to develop programs in communities around the world, including in North Korea, that are often fighting dual epidemics of HIV and TB.
The endTB team has also welcomed newcomers to TB research, including Harvard trainees and local health officials and caregivers, among them physicians and community health workers, post-doctoral fellows, master’s students, and other early-career researchers.
This new generation of researchers and care providers will help write the story of TB’s next chapter.
Already, endTB leaders and others are working toward making key TB drugs and diagnostics more affordable.
Work is also well underway on a new trial, endTB-Q, which seeks to improve treatment for a strain of tuberculosis known as pre-extensively resistant (pre-XDR) TB that is resistant to the most important standard medications.
“The work we’ve done at endTB is an important reminder that TB is curable, even when it’s drug-resistant, and that it is possible to deliver person-centered care all around the world,” Mitnick said. “Science, service, and compassion are powerful allies.”