ABSTRACT
Trastuzumab deruxtecan (T-DXd) is a human epidermal growth factor 2 (HER2)–directed antibody-drug conjugate approved in HER2-expressing breast and gastric cancers and HER2-mutant non–small-cell lung cancer. Treatments are limited for other HER2-expressing solid tumors.
METHODS
This open-label phase II study evaluated T-DXd (5.4 mg/kg once every 3 weeks) for HER2-expressing (immunohistochemistry [IHC] 3+/2+ by local or central testing) locally advanced or metastatic disease after ≥1 systemic treatment or without alternative treatments. The primary end point was investigator-assessed confirmed objective response rate (ORR). Secondary end points included safety, duration of response, progression-free survival (PFS), and overall survival (OS).
RESULTS
At primary analysis, 267 patients received treatment across seven tumor cohorts: endometrial, cervical, ovarian, bladder, biliary tract, pancreatic, and other. The median follow-up was 12.75 months. In all patients, the ORR was 37.1% (n = 99; [95% CI, 31.3 to 43.2]), with responses in all cohorts; the median DOR was 11.3 months (95% CI, 9.6 to 17.8); the median PFS was 6.9 months (95% CI, 5.6 to 8.0); and the median OS was 13.4 months (95% CI, 11.9 to 15.5). In patients with central HER2 IHC 3+ expression (n = 75), the ORR was 61.3% (95% CI, 49.4 to 72.4), the median DOR was 22.1 months (95% CI, 9.6 to not reached), the median PFS was 11.9 months (95% CI, 8.2 to 13.0), and the median OS was 21.1 months (95% CI, 15.3 to 29.6). Grade ≥3 drug-related adverse events were observed in 40.8% of patients; 10.5% experienced adjudicated drug-related interstitial lung disease (ILD), with three deaths.
CONCLUSION
Our study demonstrates durable clinical benefit, meaningful survival outcomes, and safety consistent with the known profile (including ILD) in pretreated patients with HER2-expressing tumors receiving T-DXd. Greatest benefit was observed for the IHC 3+ population. These data support the potential role of T-DXd as a tumor-agnostic therapy for patients with HER2-expressing solid tumors.
INTRODUCTIONChooseTop of pageAbstractINTRODUCTION <<METHODSRESULTSDISCUSSIONREFERENCES
Human epidermal growth factor receptor 2 (HER2) is a transmembrane tyrosine kinase receptor involved in the stimulation of cell proliferation, differentiation, and survival.1 HER2 overexpression can occur in a range of solid tumors, including breast, gastric, biliary tract, bladder, pancreatic, and gynecological tumors.2 HER2 overexpression is associated with a biologically aggressive tumor phenotype, poor prognosis, increased risk of disease recurrence, and limited benefit from chemotherapy.1,3–5 HER2-directed therapy is standard of care for HER2-expressing unresectable or metastatic breast cancer, HER2-positive locally advanced or metastatic gastric cancers, colorectal and gastroesophageal junction adenocarcinomas, and HER2-mutant non–small-cell lung cancer.6–9 However, many patients with other HER2-expressing solid tumors will progress on standard therapy, with poor prognosis and limited alternatives.5,10–13 This represents an opportunity to improve outcomes for such patients with novel HER2-targeted therapeutics.
CONTEXT
- Key Objective
- What is the efficacy and safety of trastuzumab deruxtecan (T-DXd; 5.4 mg/kg once every 3 weeks) in previously treated patients with locally advanced or metastatic human epidermal growth factor 2 (HER2)–expressing (immunohistochemistry [IHC] 3+/2+) solid tumors?
- Knowledge Generated
- DESTINY-PanTumor02 demonstrated that treatment with T-DXd resulted in durable responses across multiple tumor types, alongside clinically meaningful rates of progression-free survival and overall survival, with the greatest benefit observed in the HER2 IHC 3+ population. The safety profile was consistent with the known profile for T-DXd, including the incidence of interstitial lung disease (ILD).
- Relevance (G.F. Fleming)
- T-DXd provides meaningful benefit for patients with multiple types of solid tumors that express HER2, particularly for those whose tumors express HER2 at the 3+ level on central review.**Relevance section written by JCO Associate Editor Gini F. Fleming, MD.
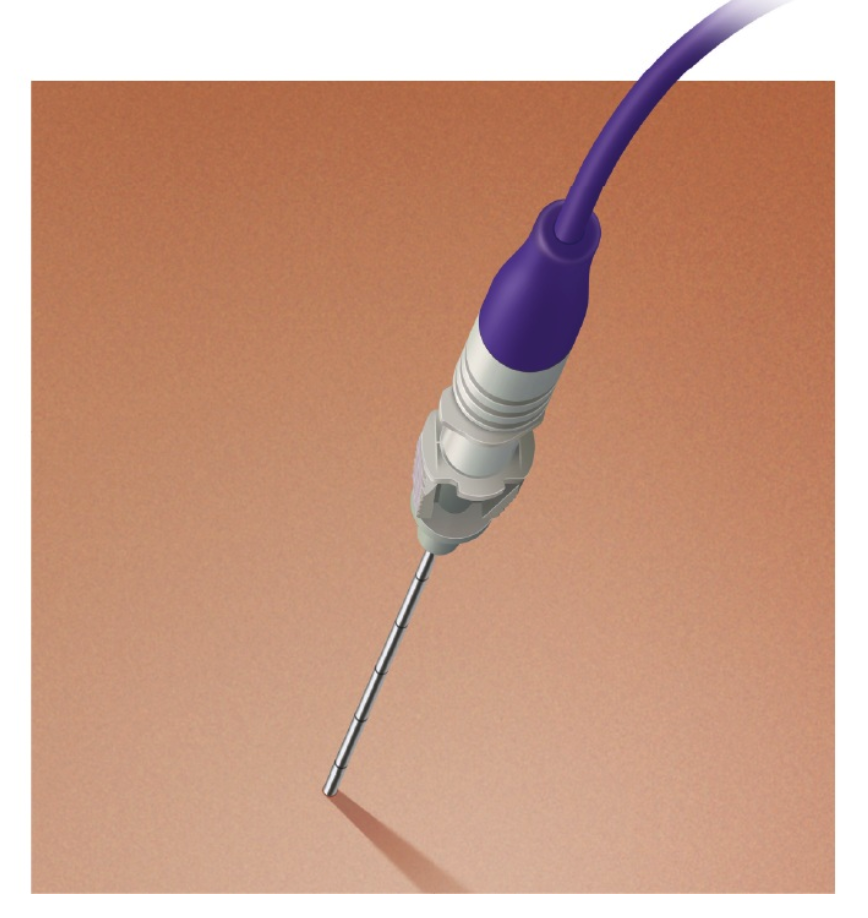
Trastuzumab deruxtecan (T-DXd) is a HER2-directed antibody-drug conjugate composed of a humanized immunoglobulin G1 anti-HER2 monoclonal antibody, a tetrapeptide-based cleavable linker, and a potent topoisomerase I inhibitor payload.14 T-DXd is currently approved in the United States and European Union for treatment of HER2-expressing breast cancer and HER2-positive gastric or gastroesophageal junction adenocarcinoma and in the United States and Japan for HER2-mutant non–small cell lung cancer.15–17 In early-phase studies, T-DXd demonstrated antitumor activity in a range of HER2–expressing malignancies, including colorectal, salivary gland, biliary tract, and endometrial cancer.18 In August 2023, T-DXd was granted breakthrough therapy designations in the United States for adult patients with unresectable or metastatic HER2-positive (immunohistochemistry [IHC] 3+) solid tumors that have progressed after prior treatment and have no satisfactory alternatives and for patients with HER2-positive (IHC 3+) metastatic colorectal cancer who have received ≥2 prior treatment regimens.19 The aim of this study (ClinicalTrials.gov identifier: NCT04482309) was to assess the efficacy and safety of T-DXd in patients with selected, locally advanced, metastatic, or unresectable HER2-expressing solid tumors.
METHODSChooseTop of pageAbstractINTRODUCTIONMETHODS <<RESULTSDISCUSSIONREFERENCES
Study Design and Participants
This open-label, multicenter, phase II study (ClinicalTrials.gov identifier: NCT04482309) evaluated the efficacy and safety of T-DXd 5.4 mg/kg once every 3 weeks in patients with previously treated HER2-expressing solid tumors in seven cohorts.
Eligible patients were age 18 years or older; had histologically confirmed locally advanced, unresectable, or metastatic biliary tract, bladder, cervical, endometrial, ovarian, pancreatic, or other solid cancers (excluding breast, colorectal, gastric, and non–small-cell lung cancers); who progressed after ≥1 systemic treatment or had no satisfactory alternative treatment options; Eastern Cooperative Oncology Group performance status of 0-120; HER2-overexpressing tumors with IHC 3+/2+ (local or central testing) scored using current ASCO/College of American Pathology guidelines for scoring HER2 in gastric cancer21; and had ≥1 investigator-assessed measurable lesion on the basis of RECIST 1.1.22 Patients with noninfectious interstitial lung disease (ILD)/pneumonitis requiring steroids, or if suspected ILD/pneumonitis could not be ruled out by imaging at screening, were excluded. HER2 expression for eligibility was based on local assessment, where available. Otherwise, eligibility was determined by central testing. HER2 IHC status was assessed centrally using HER2 HercepTest (DAKO) and scored according to gastric-specific criteria. Prior HER2-targeted therapy was permitted. Eligibility criteria are provided in Appendix 2, online only.
The study Protocol (online only) was approved by the institutional review board at each site and was conducted in accordance with the International Conference on Harmonisation Good Clinical Practice, the Declaration of Helsinki, and local regulations on the conduct of clinical research. All patients provided written informed consent before study participation.
Procedures
T-DXd was administered intravenously once every 3 weeks at 5.4 mg/kg of body weight. RECIST scans were performed at screening and every 6 weeks until documented disease progression (RECIST 1.1) or withdrawal of consent. Treatment continued until documented disease progression (RECIST 1.1), withdrawal of consent, or when discontinuation criteria were met. Dose interruptions and/or reduction and supportive therapy were permitted for clinically significant and/or unacceptable toxicity. For suspected ILD/pneumonitis, treatment was interrupted pending evaluation, and all events were followed until resolution (including after discontinuation) regardless of severity (Appendix 2).
End Points
The primary end point was investigator-assessed confirmed objective response rate (ORR), defined as the proportion of patients with a confirmed complete or partial response by RECIST 1.1 (Appendix 2). Secondary efficacy end points included duration of response (DOR; time from date of first documented response [complete or partial] until the date of documented progression or death in the absence of disease progression); disease control rate (percentage of patients with a best objective response of confirmed complete response or partial response, or with stable disease for at least 5 weeks after first dose); progression-free survival (PFS; time from first dose until date of objective disease progression or death regardless of withdrawal or receipt of another cancer therapy); and overall survival (OS; time from date of first dose until death due to any cause). An independent central review per RECIST 1.1 was performed and reported alongside the investigator-assessed results for secondary outcomes. Exploratory endpoints included subgroup analysis by HER2 status.
Secondary safety end points included the occurrence of adverse events (including drug-related adverse events, serious adverse events, and adverse events of special interest [ILD/pneumonitis and left ventricular dysfunction]) and changes in vital sign measurements and standard clinical laboratory parameters. Adverse events were coded and graded according to the Medical Dictionary for Regulatory Activities (version 26.0) and National Cancer Institute Common Terminology Criteria for Adverse Events (version 5.0). Potential cases of ILD/pneumonitis were evaluated by an independent adjudication committee.
Statistical Analysis
A sample size of 40 patients per cohort was determined to provide sufficient precision for the estimation of objective response in each cohort (eg, for ORR 35%, exact CI would be 20.6 to 51.7). Efficacy and safety results are presented by cohort and overall on the basis of the full analysis set (patients who received at least one dose of study medication). Outcomes are reported in all patients enrolled by local and central testing; subgroup analyses by HER2 status are reported as confirmed by central testing alone. Descriptive statistics were used to summarize each end point. Kaplan-Meier estimations were used to describe DOR, PFS, and OS. Exact 95% CIs for binomial proportions were calculated using the Clopper-Pearson method.
RESULTSChooseTop of pageAbstractINTRODUCTIONMETHODSRESULTS <<DISCUSSIONREFERENCES
Between October 7, 2020, and July 7, 2022, a total of 268 patients with HER2-expressing solid tumors were enrolled from >120 sites across 15 countries. Of them, 267 (99.6%) patients received at least one dose of study treatment and were included in the full analysis set; one patient withdrew before receiving treatment (Appendix Fig A1).
The median age was 62 (range, 23-85) years. Patients had received a median of two lines of prior therapy (range, 0-12; Table 1). Across all cohorts, 40.8% had received ≥three prior lines, and 14.2% had received prior HER2 therapy (trastuzumab [12.4%], pertuzumab [1.9%], zanidatamab [1.5%], trastuzumab emtansine [1.1%], trastuzumab duocarmazine [0.4%], and/or tucatinib [0.4%]). The other tumors cohort included patients with salivary gland cancer (n = 19), malignant neoplasm of unknown primary site (n = 5), extramammary Paget disease (n = 3), cutaneous melanoma (n = 2), oropharyngeal neoplasm (n = 2), adenoid cystic carcinoma, head and neck cancer, lip and/or oral cavity cancer, esophageal adenocarcinoma, intestinal adenocarcinoma, appendiceal adenocarcinoma, esophageal squamous cell carcinoma, testicular cancer, and vulvar carcinoma (all n = 1).
In total, 202 patients were enrolled on the basis of local HER2 testing, and 65 patients were enrolled on the basis of central HER2 testing. According to HER2 testing for eligibility, 111 patients were enrolled with IHC 3+ expression, 151 with IHC 2+ expression, and five with IHC 1+ expression (Table 1). On the basis of central testing, there were 75 patients with IHC 3+ expression, 125 with IHC 2+ expression, 25 with IHC 1+ expression, 30 with IHC 0 expression, and 12 patients were unknown, owing to unavailable/unevaluable samples for central testing (Appendix Table A1).
At data cutoff (June 8, 2023), the median follow-up duration across all cohorts was 12.75 months (range, 0.4-31.6); 235 patients had discontinued treatment (progressive disease [n = 167, 62.5%], any adverse event [n = 32, 12.0%], death during study [n = 18, 6.7%], patient decision [n = 11, 4.1%], investigator decision [n = 4, 1.5%], unknown [n = 2, 0.7%], lost to follow-up [n = 1, 0.4%]), and 32 (12.0%) patients remained on treatment. The median number of 21-day treatment cycles for all patients was eight.
Among the 267 patients, 99 patients (37.1%; [95% CI, 31.3 to 43.2]) had a confirmed objective response by investigator assessment. Investigator-assessed ORRs in all patients by cohort (Fig 1 and Appendix Table A2) were 57.5% for endometrial (95% CI, 40.9 to 73.0), 50.0% for cervical (95% CI, 33.8 to 66.2), 45.0% for ovarian (95% CI, 29.3 to 61.5), 39.0% for bladder (95% CI, 24.2 to 55.5), 30.0% for other tumors (95% CI, 16.6 to 46.5), 22.0% for biliary tract (95% CI, 10.6 to 37.6), and 4.0% for pancreatic (95% CI, 0.1 to 20.4). In patients with centrally confirmed HER2 IHC 3+ expression (n = 75), investigator-assessed ORRs by cohort (Fig 1) were 84.6% for endometrial (n = 13 [95% CI, 54.6 to 98.1]), 75.0% for cervical (n = 8 [95% CI, 34.9 to 96.8]), 63.6% for ovarian (n = 11 [95% CI, 30.8 to 89.1]), 56.3% for bladder (n = 16 [95% CI, 29.9 to 80.2]), 44.4% for other tumors (n = 9 [95% CI, 13.7 to 78.8]), 56.3% for biliary tract (n = 16 [95% CI, 29.9 to 80.2]), and 0% for pancreatic cancer (n = 2). In the pancreatic cohort, no objective response was observed in the first 15 patients, and the cohort was closed for further recruitment according to prespecified futility criterion, by which time 25 patients had been enrolled. Investigator-assessed ORRs by central IHC 3+/2+ status are provided in Figure 1A.
FIG 1.Investigator-assessed responses as per RECIST 1.1. (A) ORR across tumor cohorts, according to HER2 status by central testing. aResponses in the other tumors cohort include responses in extramammary Paget disease, oropharyngeal neoplasm, head and neck cancer, and salivary gland cancer. (B) The maximum change in tumor size, according to tumor type. Patients with IHC 3+ status (central testing) are marked with a dot. The other tumors cohort includes responses in extramammary Paget disease, head and neck cancer, oropharyngeal neoplasm, and salivary gland cancer. (C) DOR in patients with an objective response, according to tumor type. DOR was defined as the time from the date of first documented response (complete response or partial response) until the date of documented progression, or death in the absence of disease progression. Response was determined by investigator assessment according to RECIST 1.1 and required confirmation after the first observed response at least 4 weeks later. Censored patients are marked with a rounded dot, patients who stopped responding are marked with a triangular dot, and patients with a complete response are marked with a square dot. BTC, biliary tract cancer; DOR, duration of response; HER2, human epidermal growth factor receptor 2; IHC, immunohistochemistry; ORR, objective response rate.
Responses were observed in patients who received (n = 38; 36.8% [95% CI, 21.8 to 54.0]) or did not receive (n = 227; 37.4% [95% CI, 31.1 to 44.1]) prior HER2 therapy. Across all tumor types, 100 patients (37.5% [95% CI, 31.6 to 43.6]) had a confirmed ORR by independent central review. By cohort, ORRs by independent central review in all patients were 57.5% for endometrial (95% CI, 40.9 to 73.0), 37.5% for cervical (95% CI, 22.7 to 54.2), 42.5% for ovarian (95% CI, 27.0 to 59.1), 41.5% for bladder (95% CI, 26.3 to 57.9), 35.0% for other tumors (95% CI, 20.6 to 51.7), 26.8% for biliary tract (95% CI, 14.2 to 42.9), and 12.0% for pancreatic (95% CI, 2.5 to 31.2).
The investigator-assessed median DOR (Fig 1C and Appendix Table A2) across all cohorts was 11.3 months (95% CI, 9.6 to 17.8), ranging from 5.7 months in the pancreatic cohort to 22.1 months in the other tumors cohort; median DOR was not reached in the endometrial cohort. In all HER2 subgroups, the longest median DOR was in patients with IHC 3+ (22.1 months [95% CI, 9.6 to not reached]).
The investigator-assessed median PFS (Fig 2 and Appendix Table A2) was 6.9 months (95% CI, 5.6 to 8.0), ranging from 3.2 months in the pancreatic cohort to 11.1 months in the endometrial cohort. In all HER2 subgroups, the longest median PFS was in patients with IHC 3+ (11.9 months [95% CI, 8.2 to 13.0]). PFS by tumor cohort and HER2 status is provided in Figure 2 and Appendix Table A2.
FIG 2.Kaplan-Meier estimates of PFS, according to tumor type. (A) Endometrial cancer, (B) cervical cancer, (C) ovarian cancer, (D) bladder cancer, (E) other tumors, (F) biliary tract cancer, and (G) pancreatic cancer. IHC, immunohistochemistry; NR, not reached; PFS, progression-free survival.
Across all cohorts, the median OS (Fig 3 and Appendix Table A2) was 13.4 months (95% CI, 11.9 to 15.5; 66% maturity), ranging from 5.0 months in the pancreatic cohort to 26.0 months in the endometrial cohort. In all HER2 subgroups, the longest median OS was in patients with IHC 3+ (21.1 months [95% CI, 15.3 to 29.6]). OS by tumor cohort and HER2 status is provided in Figure 3 and Appendix Table A2.
FIG 3.Kaplan-Meier estimates of OS, according to tumor type. (A) Endometrial cancer, (B) cervical cancer, (C) ovarian cancer, (D) bladder cancer, (E) other tumors, (F) biliary tract cancer, and (G) pancreatic cancer. IHC, immunohistochemistry; NR, not reached; OS, overall survival.
Percentage change of target lesion size from baseline and a full breakdown of efficacy in the other tumors cohort are shown in Appendix Fig A2 and Appendix Table A3, respectively.
Among 267 treated patients (median follow-up of 12.75 months), ≥1 investigator-assessed drug-related adverse event was experienced by 226 (84.6%) patients (Table 2), with the most common being nausea (55.1%), anemia (27.7%), diarrhea (25.8%), vomiting (24.7%), and fatigue (24.7%). Grade 3 or higher drug-related adverse events occurred in 109 (40.8%) patients, with the most common being neutropenia (10.9%) and anemia (10.9%). Serious drug-related adverse events occurred in 36 (13.5%) patients. Drug-related adverse events led to discontinuation in 23 (8.6%) patients and dose reduction in 54 (20.2%) patients. Drug-related adverse events and non–drug-related adverse events resulting in death occurred in four (1.5%) and 19 (7.1%) patients, respectively. Adjudicated drug-related events of ILD/pneumonitis occurred in 28 (10.5%) patients, with the majority as low grade (grade 1, n = 7 [2.6%]; grade 2, n = 17 [6.4%]). There was one (0.4%) grade 3 event and three (1.1%) fatal adjudicated drug-related cases of ILD/pneumonitis, one each in the biliary tract, endometrial, and other tumors cohorts. Non-drug–related adverse events are provided in Appendix Table A4.
DISCUSSIONChooseTop of pageAbstractINTRODUCTIONMETHODSRESULTSDISCUSSION <<REFERENCES
In this phase II study, T-DXd demonstrated durable responses across multiple tumor types, alongside clinically meaningful PFS and OS in pretreated patients. The highest response rates and longest DOR, PFS, and OS were observed in tumors with IHC 3+ expression. Responses were also observed irrespective of prior HER2 therapy.
HER2 protein expression, gene amplification, and gene mutation have been identified as therapeutic targets in multiple tumor types.23 However, HER2-targeted therapy is not currently approved beyond breast, gastric, colorectal, and lung cancer.5,15,24 The tumor types investigated here were predefined on the basis of epidemiological frequency, prevalence of HER2 expression, and unmet medical need.2,5 Investigations are supported by phase I clinical data of T-DXd and encouraging results from the HERALD phase II basket trial which assessed T-DXd in advanced solid tumors with HER2 amplification.18,25
Of note are the magnitudes of benefit observed in the endometrial, cervical, and ovarian cohorts; the highest ORRs were observed in these cohorts across all studied tumor types (57.5% for endometrial, 50.0% for cervical, 45.0% for ovarian). To the best of our knowledge, this is the first report of a HER2-directed antibody-drug conjugate in these gynecological tumors. In the endometrial cohort, 77.5% of patients had ≥two prior lines of therapy. The ORR in patients with HER2 IHC 3+ expression was 84.6%. In all patients with endometrial cancer, median PFS and OS were 11.1 months and 26.0 months, respectively. The clinically significant response and survival rates observed in this study are encouraging for HER2-expressing endometrial cancers, which are typically associated with high risk for progression and poor survival rates.10 In the cervical cohort, 85.0% of patients had ≥two prior lines of therapy, and the ORR in patients with HER2 IHC 3+ expression was 75.0%. The median OS in this cohort was 13.6 months in all patients, not reached in IHC 3+ patients, and 11.5 months in IHC 2+ patients. These data are promising in a cohort with few treatment options and a typically low response rate to treatment.11 The median number of prior treatments in the ovarian cohort was three, and 35.0% of patients had five or more prior lines of therapy; the median OS was 13.2 months in all patients and 20.0 months in patients with HER2 IHC 3+ expression. The results from this study further support use of a HER2 antibody-drug conjugate for treating ovarian cancer, and the outcomes are promising for a disease subgroup with a high mortality rate.12,26
Although there was only one investigator-assessed responder in the pancreatic cohort (4.0%; closed to recruitment with 25 patients enrolled), when assessed by independent central review, three responses were observed (12.0%). PFS and OS results showed potential in the late-line pancreatic cancer setting; however, it is challenging to draw conclusions from this cohort owing to the low patient numbers, particularly in the IHC 3+ group.
Biliary tract cancer (BTC) is uncommon12 but has a high mortality rate13 and limited clinical benefit from second-line chemotherapy.27 The phase II trial of T-DXd in patients with unresectable or recurrent HER2-expressing BTCs showed promising activity in patients with HER2-positive (IHC 3+ and IHC 2+/in-situ hybridization+) BTC.28 The data in the DESTINY-PanTumor02 trial further support HER2 as a therapeutic target in BTC where an ORR of 56.3% and OS of 12.4 months were observed in patients with IHC 3+ tumors.
Safety findings for T-DXd in this trial were consistent with the established safety profile.15 A risk of pulmonary adverse events, primarily ILD/pneumonitis, has been observed in patients receiving T-DXd and is an important consideration for these patients.29,30 Although most cases of adjudicated drug-related ILD in this trial were low-grade and manageable and overall incidence was consistent with that in previous studies,31 three adjudicated drug-related ILD/pneumonitis-related deaths occurred. Multidisciplinary guidelines for diagnosing and managing T-DXd–related ILD/pneumonitis have been published.29 T-DXd–related ILD/pneumonitis can be safely managed with a multidisciplinary team, who should manage the ILD/pneumonitis jointly with the medical oncologist and may include a primary care physician, nurse practitioner, pulmonologist, pathologist, pharmacist, infectious disease specialist, and radiologist. Patients should be proactively monitored for ILD/pneumonitis, and suspected cases should be actively managed by a multidisciplinary team; T-DXd treatment should be interrupted in the event of grade 1 ILD/pneumonitis, and the event must resolve before treatment may resume.29
This tumor-agnostic biomarker-driven approach represents an innovative application of the principles of precision medicine.5 Despite the prospects of the tumor-agnostic strategy, only six drugs have received US Food and Drug Administration approval on the following basis: pembrolizumab for microsatellite instability high, mismatch repair deficient, or tumor mutational burden high tumors; dostarlimab for mismatch repair deficient tumors; larotrectinib or entrectinib for tumors with NTRK gene fusions; dabrafenib plus trametinib for tumors with BRAF V600E mutations; and selpercatinib for tumors with RET gene fusions.32 As with those studies, this trial has a clear rationale on the basis of preclinical/clinical data and demonstrates meaningful antitumor activity across endometrial, cervical, ovarian, bladder, biliary tract, and other tumor cohorts.
A tumor-agnostic investigative approach has some limitations, most notably the single-arm nature of the studies. It was not possible to include a single comparator, given the range of tumor types that were included. Another potential limitation is the few patients included with HER2 IHC 1+ tumors. The protocol allowed for recruitment of patients with HER2 IHC 1+ tumors once 3 of 15 responders within a cohort had been observed in centrally confirmed HER2 IHC 3+ or IHC 2+ tumors. However, only the cervical cohort prospectively opened enrollment to patients with IHC 1+ tumors as recruitment in other cohorts was complete by the time response rate data were available on the first 15 patients. There is limited evidence available from this study in HER2-low patients, a population of growing clinical interest after the approval of T-DXd in HER2-low breast cancer.15 The few responses in patients who were determined to be IHC 1+/0 on retrospective central testing suggest that further exploration in patients with IHC 1+ tumors is warranted beyond breast cancer.
In this global, multicenter phase II study, treatment with T-DXd demonstrated robust clinical activity providing durable clinical benefit for pretreated patients with selected HER2-expressing solid tumors. The observed safety profile, including ILD, was consistent with that in previously reported studies of T-DXd. These data provide clinical evidence for antitumor activity of T-DXd across multiple tumor types, suggesting potential tumor-agnostic activity in patients with HER2-expressing solid tumors.