Rabies is an acute encephalitis caused by viruses in the genus Lyssavirus, family Rhabdoviridae, that is nearly uniformly fatal in unvaccinated hosts. Although the virus is present in animal reservoirs, infection in humans is rare in the United States, with only two cases reported in 20031,2 and no more than six cases reported in any year in the past decade.3 The primary mode of transmission is through the bite of an infected animal, most commonly a bat in the United States.4 Although transmission of rabies virus from corneal transplants has previously been described,5 to our knowledge, no cases ascribed to organ or vascular-tissue transplants have been reported.
In May 2004, physicians at a hospital in Texas diagnosed encephalitis in three recipients of a liver and two kidneys from a common organ donor. It was later discovered that encephalitis also developed in a fourth patient, who had received a vascular graft from the same donor during liver transplantation. All four patients became progressively obtunded, lapsed into coma, and died within 50 days after transplantation. The initial diagnostic evaluation revealed no cause of the encephalitis, and assistance was sought from the Centers for Disease Control and Prevention (CDC) and the Texas Department of State Health Services. We report the results of this investigation.
CASE REPORTS
Transplant Recipients
In May 2004, encephalitis was diagnosed in three recipients of a liver and two kidneys (Patients 2, 3, and 4 in Figure 1FIGURE 1The Clinical Course of Four Recipients of Rabies-Infected Tissue or Organs.) from a common organ donor. In all three patients, signs and symptoms of altered mental status and progressively worsening encephalitis developed within 30 days after transplantation. Major clinical events and immunosuppressive medications are summarized in Figure 1. All patients had rapid neurologic deterioration characterized by agitated delirium and seizures. Respiratory failure requiring intubation developed within 48 hours after the onset of neurologic symptoms. Examination of cerebrospinal fluid from the three patients showed pleocytosis, with an average of 18 cells per cubic millimeter (range, 7 to 35), and elevated protein levels (mean, 135 mg per deciliter; range, 17 to 331). Neurologic imaging in the week after the onset of symptoms showed no evidence of an acute cerebral process. Magnetic resonance imaging (MRI) performed later in the course of illness demonstrated diffuse signal abnormalities, most often in the temporal lobes, basal ganglia, brain stem, and hippocampi on T2-weighted and fluid-attenuated inversion recovery images (Figure 2FIGURE 2Axial Fluid-Attenuated Inversion Recovery MRI Scan Showing Profound Signal Abnormalities within the Bilateral Frontal and Temporal Lobes, Hippocampi, Basal Ganglia, and Medulla in Patient 2.). There was minimal enhancement after the administration of gadolinium. The patients died an average of 13 days after the onset of neurologic symptoms (range, 7 to 23).
Organ Donor
Four days before death, the organ donor was seen twice at an emergency department for nausea, vomiting, and difficulty swallowing. He was subsequently admitted to another hospital with altered mental status requiring intubation. Physical examination revealed a temperature of 38.1°C (100.5°F) and fluctuating blood pressures, including systolic measurements of more than 200 mm Hg. On admission, a urine toxicology screen was positive for cocaine and marijuana, and computed tomography of the brain demonstrated a subarachnoid hemorrhage. The hemorrhage progressed, and the neurologic symptoms, including seizures and coma, worsened. The patient was declared brain-dead within four days after presentation. Donor-eligibility screening and testing performed by an organ-procurement organization, including a review of premortem blood, urine, and sputum bacterial cultures, did not detect any signs or symptoms of infection precluding solid-organ donation. The patient’s kidneys, lungs, and liver were removed for transplantation; in addition, iliac arteries were harvested for potential use in vascular reconstruction during the liver transplantation. In part because of the positive toxicology result, nonorgan tissues (e.g., tendons) were not removed. During contact investigations conducted after the rabies diagnoses were made, friends of the donor indicated he had reported being bitten by a bat.
METHODS
Clinical and Epidemiologic Review
Medical records of the donor and infected transplant recipients were reviewed to characterize clinical courses and diagnostic evaluations. After the laboratory diagnosis of rabies infection in the three organ recipients, case finding was performed to search for other possible cases. Hospital autopsy records on patients with encephalitis were reviewed for pathological findings consistent with the presence of rabies. Also, charts of patients who had been on the same floor as a patient with rabies and who had also had a lumbar puncture or neurology consultation for altered mental status were examined for documented clinical findings consistent with the presence of rabies. Procedures for organ recovery and handling were also reviewed.
Laboratory Methods
Formalin-fixed, paraffin-embedded tissue specimens, obtained at autopsy, were stained with hematoxylin and eosin and various immunohistochemical stains according to a method described previously.6 For immunohistochemical assays, 3-μm tissue sections were deparaffinized, rehydrated, and digested in proteinase K. Tissue sections were incubated for 60 minutes at room temperature with a hyperimmune rabbit antiserum or mouse ascitic fluid with reactivity to rabies virus. After sequential application of the appropriate biotinylated linked antibody, avidin–alkaline phosphatase complex, and naphthol fast-red substrate, sections were counterstained in Meyer’s hematoxylin and mounted with the use of aqueous mounting medium. Serologic analyses, detection of viral antigen in tissue by means of fluorescence microscopy, and identification of rabies virus variants were performed as described previously.7,8 Controls included serum specimens from noninfected animals, tissues from humans with nonrabies encephalitides, and rabies-infected human tissues. Immunohistochemical assays for various other viral, rickettsial, and protozoan agents of encephalitis were also performed on tissues from recipients.
Vero E6 cells were inoculated with CSF and 10 percent tissue suspensions from three of the four rabies-infected recipients (Patients 2, 3, and 4). Suckling mice were inoculated intracranially and intraperitoneally with cerebrospinal fluid and 10 percent clarified homogenates of brain tissue, spinal cord, and kidney suspensions. Tissue cultures and suckling mice were observed daily for cytopathic effects and signs of illness, respectively. Tissues obtained from suckling mice that developed neurologic signs or died were fixed in 10 percent neutral buffered formalin or 2.5 percent buffered gluteraldehyde or were frozen for further evaluation. At 14 days, the Vero E6 cells were suspended in saline, fixed on glass slides, and tested for the presence of rabies virus antigen by means of a direct fluorescence antibody assay according to a previously described method.9 Immunohistochemical studies were performed as described above, and formalin-fixed tissues were embedded for examination by electron microscopy.
RESULTS
Review of Transplantation Records
All organs obtained from the donor were transplanted; the lung recipient died of intraoperative complications. Iliac arteries from the donor were not used during the liver transplantation in Patient 2 and were placed in a sterile container and stored for potential use in subsequent transplantation procedures. One day after the organs were transplanted, the iliac-artery segment was retrieved and used to construct a vascular graft for another liver-transplant procedure (in Patient 1).
Rabies Case Finding
In addition to the three initial cases noted by physicians, autopsy review identified a fourth patient (Patient 1 in Figure 1) in whom progressive, fatal encephalitis had developed after liver transplantation. This patient had received the vascular segment from the rabies-infected donor. A review of the medical records of patients who had been on the same floor as a patient with rabies and who had had a lumbar puncture or neurology consultation for altered mental status revealed no further cases of encephalitis consistent with the presence of rabies.
Pathological Findings
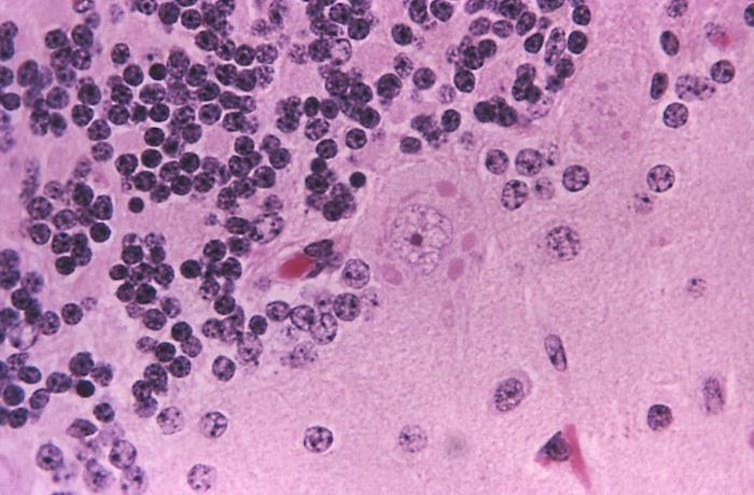
Histopathological evaluation of tissues from all four rabies-infected transplant recipients demonstrated diffuse, predominantly lymphohistiocytic, infiltrates and microglial nodules involving the cerebrum, brain stem, cerebellum, and spinal cord. Cytoplasmic inclusions consistent with Negri bodies were identified throughout the central nervous system (CNS), particularly in the Purkinje cells of the cerebellum and in neurons of the frontal cortex, thalamus, hippocampus, midbrain, and pons (Figure 3AFIGURE 3Histopathological Findings in Patient 4.). Lymphohistiocytic infiltrates involving the peripheral nerves, heart, and kidneys were also noted in some patients. Electron microscopy of the midbrain of Patient 4 demonstrated abundant rhabdovirus particles (Figure 3B). Intracytoplasmic rabies virus antigens were detected on immunohistochemical staining in neurons from multiple areas of the CNS (Figure 3C); in peripheral nerves of the transplanted kidneys, liver, and arterial graft (Figure 4FIGURE 4Immunohistochemical Staining (Red) of Rabies Virus Antigens in Peripheral Nerves of the Liver (Panels A and B), Kidney (Panel C), and Arterial-Graft Transplants (Panel D).); and in renal tubular epithelium, smooth muscle, histiocytes, and vascular endothelium. No tissues were positive for enteroviruses, human herpesviruses 1 and 2, West Nile and other flaviviruses, eastern equine encephalomyelitis virus, lymphocytic choriomeningitis virus, Cache Valley virus, henipaviruses, measles virus, spotted fever and typhus group rickettsiae, Toxoplasma gondii, or Trypanosoma cruzion immunohistochemical analysis. Direct fluorescence antibody staining also demonstrated rabies virus antigens in CNS tissues from all recipients.
Serologic Analyses and Viral Identification
Antibodies (IgM and IgG) reactive to rabies virus were present in the donor’s serum at the time of death. Antibodies were also present in three of the four recipients in samples obtained on postoperative days 35 and 36; both IgM and IgG antibodies were present in one kidney recipient (Patient 3) and the recipient of the donor’s liver (Patient 2), whereas only IgG antibodies were present in the patient who received the arterial segment (Patient 1). Antigenic typing revealed a previously characterized rabies virus variant associated with bats.
Cell Culture and Mouse Inoculations
All suckling mice had neurologic abnormalities or had died seven to eight days after inoculation. Thin-section electron microscopy of CNS tissue demonstrated rhabdovirus particles, and IHC testing detected rabies virus antigens in mouse CNS tissues. Cultures of Vero E6 cells inoculated with brain, spinal cord, and kidney from a kidney recipient demonstrated rabies virus antigen on staining with DFA.
DISCUSSION
This report describes the transmission of rabies virus through the transplantation of solid organs and vascular material. Four patients who received transplants — three organs and one vascular segment — from a donor with unrecognized rabies infection subsequently died of rabies. The transmission of rabies from corneal transplants has been described previously.5
Rabies is seldom included in the differential diagnosis of encephalitis in the absence of a documented exposure or suggestive history.8,10 The symptoms in the cases reported here, including fever, changes in mental status, and autonomic instability, were, in retrospect, consistent with a diagnosis of rabies. However, the diagnosis was complicated by the absence of a history of exposure at presentation and by the number of other potential causes of illness in these immunosuppressed patients. A history of a bat bite in the donor was discovered during contact interviews only after rabies had been diagnosed, and the investigation initiated. The diagnosis in the donor was further complicated by the presence of a subarachnoid hemorrhage in the setting of hypertension and a positive toxicology screen for cocaine. It is not known whether rabies infection was the cause of the subarachnoid hemorrhage, since this finding has not been noted in previous reports.11-13
Signs of rabies developed in all four transplant recipients within 30 days after infection. According to previous reports, symptoms developed within 30 days after an animal bite in only 25 percent of patients.10 It is unknown whether the shorter incubation period in these patients was due to the immunosuppression, the route of transmission, or both. The effect of immunosuppression on rabies infection is currently not well understood. In reports of rabies transmission from corneal transplants in patients who were not immunosuppressed and did not receive postexposure prophylaxis, symptoms developed an average of 26 days after transplantation,14-17 suggesting that implantation of material from infected donors may lead to a shorter incubation period. Three of our patients presented with commonly described symptoms of tremors and changes in mental status, whereas the fourth presented with abdominal and flank pain, which may have been neuropathic, and changes in mental status occurred about 48 hours later. The rapidly progressive encephalitis, with death occurring an average of 13 days after the onset of symptoms, is consistent with the course in other reports.4
There is only one reported case of recovery from clinical rabies by a patient who had not received preexposure or postexposure prophylaxis against rabies.18 However, administration of postexposure prophylaxis with rabies immune globulin and vaccine is highly effective in preventing infection after exposure. In a previous report, administration of postexposure prophylaxis probably prevented infection in a patient who had received a cornea from a donor with rabies.19
This report and another, describing the transmission of West Nile virus through solid-organ transplantation,20 underscore the potential for transmission of unexpected infectious diseases through organ transplantation. Recognition and prevention of transplant-transmitted infections may be improved in various ways, including enhanced donor screening and testing, the development of standardized procedures related to storage and use of donor vascular segments, as well as methods to track their use or nonuse, and enhanced means of detection and diagnosis of illnesses in recipients.
To minimize the risk of transmitting infections during organ transplantation, the Organ Procurement and Transplantation Network (OPTN) has established standards that require organ-procurement organizations to assess the risks of infectious diseases through screening questions and blood testing for selected bloodborne viral pathogens and syphilis.21 Questions about potential exposure to rabies are generally not included, and laboratory testing for rabies infection is not performed. Organs can be procured from donors who are febrile, provided that the medical director of the organ-procurement organization and the transplantation physicians agree that the cause of the fever does not pose an unacceptable risk to the recipient. Given the growing importance of emerging and reemerging infectious diseases, the ability of general improvements in the donor-screening process, rather than disease-specific measures, to increase organ safety should be evaluated. A proposed revision of OPTN policies would expand the list of potentially transmittable diseases and conditions that clinicians should consider in determining a donor’s eligibility.22 The revision emphasizes that when any of these conditions is known or suspected in a donor, this information should be conveyed immediately to the organ-procurement organization as well as to all transplantation centers that received organs from the donor.
The successful use of donor arterial conduits has been reported in liver transplantation23-26 and in the management of vascular complications in recipients of both hepatic transplants27,28 and renal transplants.29 As with organs, these vessel segments have the potential to transmit infection. A careful accounting of and an ability to track donated material, such as vessel conduits, are essential in efforts to link unexplained illnesses or deaths to a common organ donor and will increase the probability of quickly identifying all recipients who may be at risk from donor infections. Proposed revisions of the policies of both OPTN22 and the Joint Commission on Accreditation of Healthcare Organizations30 may help address the storage of vessel conduits and documentation of their use or nonuse.
Our investigation underscores the challenge in detecting and diagnosing infections that occur in recipients of organs or tissues from a common donor. The potential for disease transmission from a donor as a cause of illness or death may not be considered in the evaluation of an individual recipient. In this investigation, and in the previous report of the transmission of West Nile virus through transplantation, the ability to connect illnesses to a common organ donor was facilitated by the fact that multiple recipients were hospitalized at the same facility. Improved national detection of unexpected or serious outcomes among transplant recipients may facilitate the discovery of transplant-related transmission of emerging and unusual pathogens by allowing connections to common donors to be made. The ability to make retrospective diagnoses of infections in organ donors when unexplained deaths or illnesses occur in recipients is hampered by the limited availability of donor samples, particularly tissue; currently, only serum samples from organ donors are retained for any length of time. Investigations into possible transplantation-associated infections would be facilitated by the availability of selected, archived tissue samples from the donor and by autopsy reports and materials. An improved diagnostic ability may have important implications for other patients who received material from the donors and for contacts of the patients and donors.
As organ and tissue transplantation becomes more common, the potential risks of disease transmission may increase. Cases of transplantation-associated infections provide important opportunities to review practices in an attempt to enhance the safety of transplantation without affecting the organ supply. The Department of Health and Human Services, including the CDC, is working with other partners in the organ- and tissue-transplantation community to review donor-screening practices, the use of retained vascular segments, and surveillance of recipients for illness. Clinicians who care for organ-transplant recipients should continue to be aware of the potential for disease transmission through transplantation and the challenges in recognizing atypical presentations of infections in this immunosuppressed population. Clinicians should report unexpected outcomes or unexplained illnesses in transplant recipients to their local organ- and tissue-procurement organization.
We are indebted to the state health departments in Oklahoma and Alabama, to the Southwest Transplant Alliance, and to the staff of the Baylor University Medical Center for their assistance with this investigation.
Source: NEJM