Editor’s summary
The microbiota plays an important part in host defense by excluding pathogenic species in a process called colonization resistance. This property is elusive and not endowed by one or two species alone. Spragge et al. discovered that colonization resistance is a higher-order effect of a diverse community of bacteria underpinned by essential key species such as Escherichia coli (see the Perspective by Radlinski and Bäumler). In vitro and in vivo experiments showed that given the right composition, a diverse microbiota will collectively consume the nutrients that an incoming species requires to grow and establish in a host. Colonization resistance is predictable because if the symbiont community encodes many of the same (or similar) proteins as the pathogen, then it provides better colonization resistance and can potentially deliver health benefits to the host. —Caroline Ash
Structured Abstract
INTRODUCTION
The diverse bacterial species that colonize the human gut, which are collectively known as the gut microbiota, provide important health benefits. One of the key benefits is colonization resistance—the ability to restrict colonization of the gut by pathogens that can trigger disease. Multiple mechanisms have been found to influence the ability of the microbiota to provide colonization resistance, but these mechanisms are often context-specific and dependent on particular strains or species of bacteria. As a result, we lack general principles to predict which microbiota communities will be protective versus those that will allow pathogens to colonize.
RATIONALE
We used an ecological approach to study the colonization resistance provided by human gut symbionts against two important bacterial pathogens, Klebsiella pneumoniae and Salmonella enterica serovar Typhimurium. We studied colonization resistance provided by symbionts both alone and in combinations of increasing diversity to identify general patterns underlying colonization resistance, using both in vitro assays and in vivo work with gnotobiotic mice.
RESULTS
We cultured 100 human gut symbionts individually with K. pneumoniae and then S. Typhimurium and ranked the symbionts on the basis of their ability to provide colonization resistance. However, even the best-performing species provided limited protection against the pathogens in our assays. By contrast, when we combined species into diverse communities of up to 50 species, we found cases in which pathogen growth was greatly limited. The same patterns were observed when germ-free mice were colonized by a subset of these communities and challenged with a pathogen. Ecological diversity, therefore, was important for colonization resistance, but we also found that community composition was important. Both in vitro and in vivo, we found that colonization resistance rested upon certain species being present, even though these species offer little protection on their own. We were able to explain these patterns from the ability of some communities to block pathogen growth by consuming the nutrients that the pathogen needs. Nutrient blocking is thus promoted both by diversity and by the presence of certain key species that increase the overlap between the nutrient use of a community and a pathogen. As a result, the inclusion of a key species closely related to a pathogen can be central to making a community protective because it provides a higher degree of metabolic overlap. However, this alone is typically not sufficient. We found that the presence of additional, often distantly related species is also needed to ensure that nutrient blocking—and consequently, colonization resistance—occurs. Lastly, we used the nutrient-blocking principle to predict in silico more-protective and less-protective communities for a new target strain, an antimicrobial resistant Escherichia coli clinical isolate. We then tested the colonization resistance of these communities experimentally. This work revealed that we can successfully identify protective communities from a large number of possible combinations, using both phenotypic measures of metabolic overlap but also a more general measure of genomic overlap.
CONCLUSION
Our results support the idea that more-diverse microbiomes can provide health benefits, specifically that they can improve protection against pathogen colonization. We also find that colonization resistance is a collective property of microbiome communities; in other words, a single strain is protective only when in combination with others. Crucially, although increased microbiome diversity increases the probability of protection against pathogens, the overlap in nutrient-utilization profiles between the community and the pathogen is key. Our work suggests a route to optimize the composition of microbiomes for protection against pathogens.

Abstract
The human gut microbiome plays an important role in resisting colonization of the host by pathogens, but we lack the ability to predict which communities will be protective. We studied how human gut bacteria influence colonization of two major bacterial pathogens, both in vitro and in gnotobiotic mice. Whereas single species alone had negligible effects, colonization resistance greatly increased with community diversity. Moreover, this community-level resistance rested critically upon certain species being present. We explained these ecological patterns through the collective ability of resistant communities to consume nutrients that overlap with those used by the pathogen. Furthermore, we applied our findings to successfully predict communities that resist a novel target strain. Our work provides a reason why microbiome diversity is beneficial and suggests a route for the rational design of pathogen-resistant communities.


 (Eawag)
(Eawag) (Eawag)
(Eawag) (Eawag)
(Eawag)
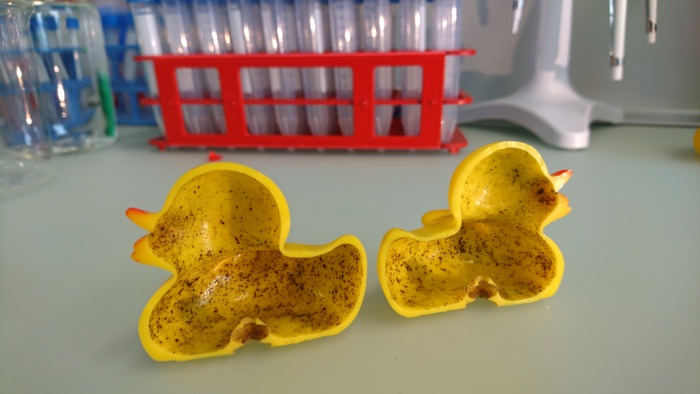
 The urinal project from 2015 / Credit: UWE Bristol News
The urinal project from 2015 / Credit: UWE Bristol News
