Sleep is known to play a key role in facilitating various physiological processes, while also contributing to the healthy functioning of the brain. Lack of sleep and poor sleep quality have been linked to various chronic health and mental health issues, including high blood pressure, depression, stroke, obesity, and heart disease.
Sleep disturbances have also been implicated in the development of neurodegenerative diseases. Interestingly, neurodegenerative diseases have also been associated with the dysfunction of microglia, the primary mammalian immune cells, yet the link between microglia and sleep has not been thoroughly studied yet.
Researchers at University of California Berkeley (UC Berkeley), Huazhong University of Science and Technology and other institutes in China recently carried out a study exploring the potential role of microglia in regulating sleep. Their findings, published in Nature Neuroscience, suggest that microglia regulate sleep by modulating the transmission of the neurotransmitter norepinephrine, which is known to contribute to arousal, attention and stress reactions.
“We show in mice that microglia can regulate sleep through a mechanism involving Gi -coupled GPCRs, intracellular Ca2+ signaling and suppression of norepinephrine transmission,” Chenyan Ma, Bing Li and their colleagues wrote in their paper.
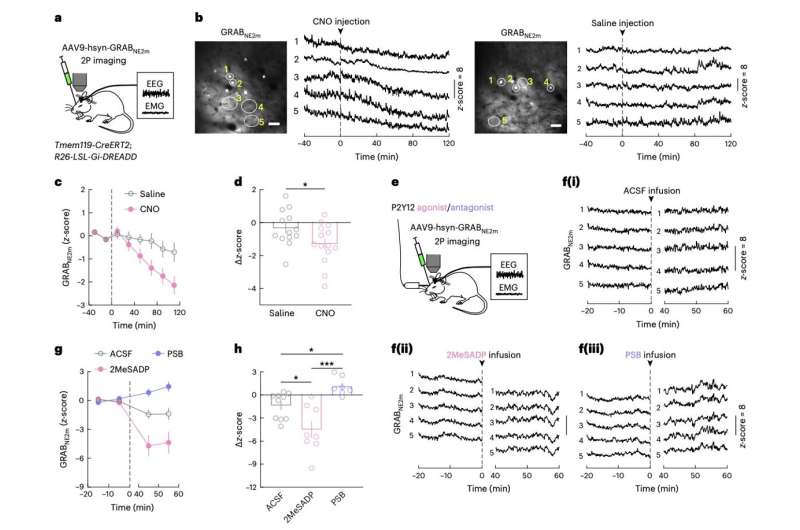
To investigate the role of microglia in sleep regulation, the researchers carried out a series of experiments on mice, using chemogenetic techniques to manipulate and image microglia signaling in their brain. Specifically, they selectively activated or blocked P2Y12, a Gi -protein-coupled ATP/ADP receptor that has been found to be central to the function of microglia.
The team observed the neural mechanisms that followed the experimental activation/blocking of P2Y12–Gi signaling and recorded the sleeping behavior of the mice. This allowed them to gather new insight about how microglia may regulate sleep in mice, and potentially also in humans and other mammals.
“Chemogenetic activation of microglia Gi signaling strongly promoted sleep, whereas pharmacological blockade of Gi -coupled P2Y12 receptors decreased sleep,” the researchers wrote.
“Two-photon imaging in the cortex showed that P2Y12–Gi activation elevated microglia intracellular Ca2+, and blockade of this Ca2+ elevation largely abolished the Gi -induced sleep increase. Microglia Ca2+ level also increased at natural wake-to-sleep transitions, caused partly by reduced norepinephrine levels. Furthermore, imaging of norepinephrine with its biosensor in the cortex showed that microglia P2Y12–Gi activation significantly reduced norepinephrine levels, partly by increasing the adenosine concentration.”
Overall, the results collected by Ma, Li and their colleagues suggest that microglia play a key role in the regulation of sleep. Specifically, these immune cells appear to regulate sleep via reciprocal interactions with the transmission of norepinephrine.
These initial observations could soon pave the way for further studies investigating the role of microglia in sleep regulation, focusing on norepinephrine transmission.
As microglia dysfunction and sleep disturbances have been linked to Alzheimer’s and other neurodegenerative diseases, this work may also broaden neuroscientists’ understanding of these diseases, potentially aiding the future development of new therapeutic strategies.
