Abstract
Background
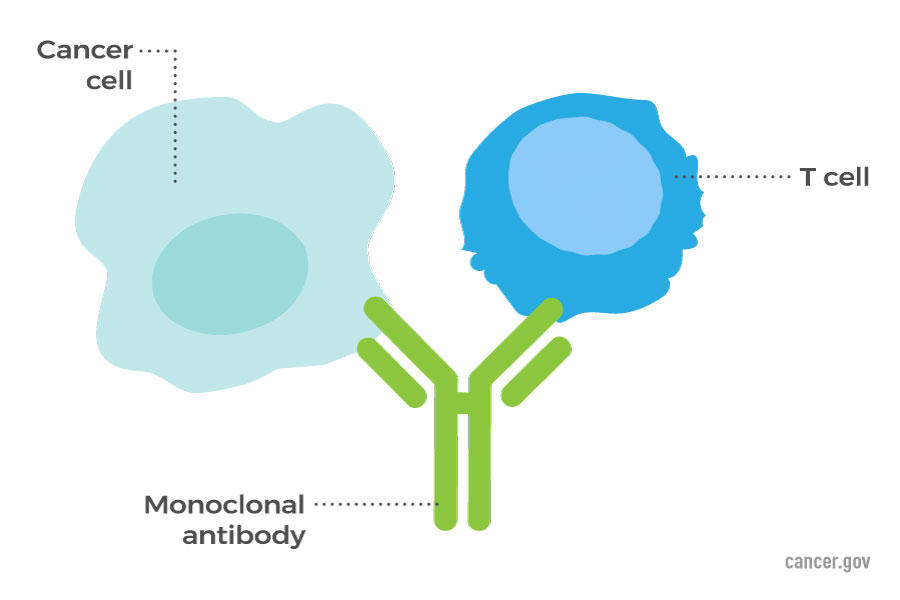
The use of monoclonal antibodies has changed the treatment of several immune-mediated inflammatory diseases, including psoriasis. However, these large proteins must be administered by injection. JNJ-77242113 is a novel, orally administered interleukin-23–receptor antagonist peptide that selectively blocks interleukin-23 signaling and downstream cytokine production.
Methods

In this phase 2 dose-finding trial, we randomly assigned patients with moderate-to-severe plaque psoriasis to receive JNJ-77242113 at a dose of 25 mg once daily, 25 mg twice daily, 50 mg once daily, 100 mg once daily, or 100 mg twice daily or placebo for 16 weeks. The primary end point was a reduction from baseline of at least 75% in the Psoriasis Area and Severity Index (PASI) score (PASI 75 response; PASI scores range from 0 to 72, with higher scores indicating greater extent or severity of psoriasis) at week 16.
Results
A total of 255 patients underwent randomization. The mean PASI score at baseline was 19.1. The mean duration of psoriasis was 18.2 years, and 78% of the patients across all the trial groups had previously received systemic treatments. At week 16, the percentages of patients with a PASI 75 response were higher among those in the JNJ-77242113 groups (37%, 51%, 58%, 65%, and 79% in the 25-mg once-daily, 25-mg twice-daily, 50-mg once-daily, 100-mg once-daily, and 100-mg twice-daily groups, respectively) than among those in the placebo group (9%), a finding that showed a significant dose–response relationship (P<0.001). The most common adverse events included coronavirus disease 2019 (in 12% of the patients in the placebo group and in 11% of those across the JNJ-77242113 dose groups) and nasopharyngitis (in 5% and 7%, respectively). The percentages of patients who had at least one adverse event were similar in the combined JNJ-77242113 dose group (52%) and the placebo group (51%). There was no evidence of a dose-related increase in adverse events across the JNJ-77242113 dose groups.
Conclusions
After 16 weeks of once- or twice-daily oral administration, treatment with the interleukin-23–receptor antagonist peptide JNJ-77242113 showed greater efficacy than placebo in patients with moderate-to-severe plaque psoriasis.