When lung cancer is found early, before it has spread beyond the lungs, people usually have surgery to remove the tumor. For more than 25 years, the standard of surgical care for such patients—even those with very small tumors—has been to remove the entire large section, or lobe, of the lung that contains the tumor. This is done to reduce the chances of the cancer coming back.

But some lung surgeons have suggested that certain patients may do just as well or even better with an operation to remove only part of the affected lobe.
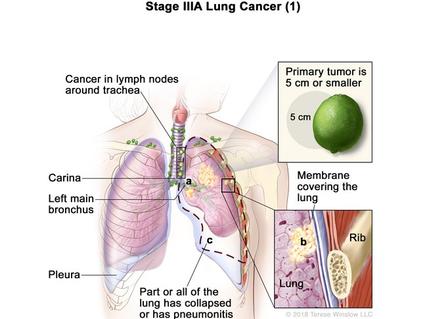
Now, results of a large international clinical trial show that, for certain people with early-stage non-small cell lung cancer (NSCLC), surgery to remove a piece of the affected lobe is as effective as surgery to remove the whole lobe.
In the trial, people with early-stage NSCLC who had the more limited surgery lived as long without their cancer coming back as those who had an entire lobe of the lung removed. In addition, the portion of people still living after 5 years was about 80% in both groups.
Results of the new study were reported February 9 in the New England Journal of Medicine.
The new findings signal “a tremendous change in how we approach this type of lung cancer,” said Nasser Altorki, M.D., chief of thoracic surgery at Weill Cornell Medicine and New York-Presbyterian Hospital, who led the trial.
“This groundbreaking study confirms the results of a similar large study from Japan” reported last year, said David Tom Cooke, M.D., chief of general thoracic surgery at UC Davis Health, who enrolled patients in the international study and performed surgeries on some participants.
Together, the two trials show that carefully selected patients “can benefit from having less of their lung tissue removed to give them the same chance of a cure,” Dr. Cooke said. And removing less lung tissue “might mean better lung function long term.”
Standards for lung cancer surgery have changed over time
Each lung is made up of large sections called lobes, with three lobes in the right lung and two in the left. Each lobe is further divided into several anatomical units called segments.
Surgery for lung cancer originally involved removing an entire lung. Removing a whole lobe is called a lobectomy. In sublobar surgery, sometimes called lung-sparing surgery, surgeons may remove an entire segment of a lobe, which is akin to removing a segment of an orange. Or they may remove only a wedge-shaped piece of the lung, which is like taking a bite out of the orange, Dr. Cooke explained.
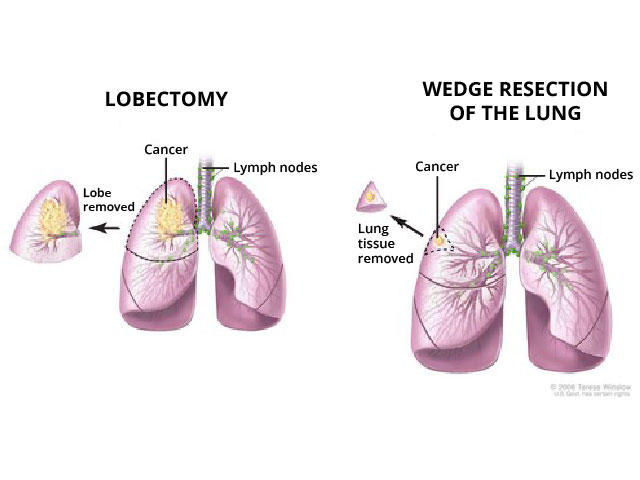
In 1995, results from a key clinical trial showed that, for people with early-stage NSCLC, removing a lobe was better than removing part of a lobe. Trial participants who had only part of the affected lobe removed were three times more likely than those who had a lobectomy have their cancer come back (recur).
“Thereafter, lobectomy was the standard of surgical care for this group of patients,” explained thoracic surgeon Valerie Rusch, M.D., of Memorial Sloan Kettering Cancer Center, in an editorial accompanying the new study results. Lung-sparing surgery, Dr. Rusch noted, was used only for patients with limited lung function.
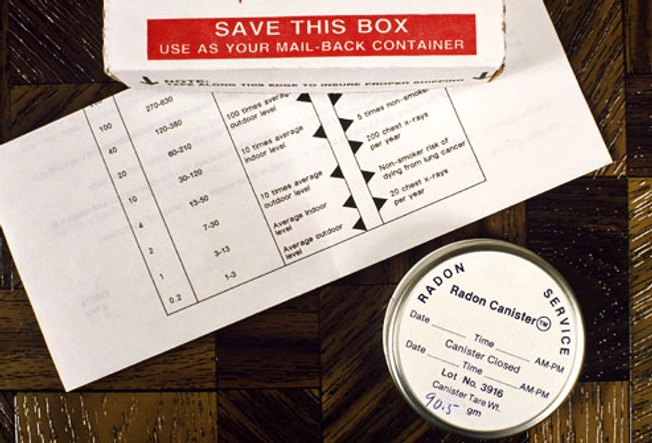
However, in recent decades, advances in imaging technology and new staging methods have enabled the detection and diagnosis of smaller, earlier-stage lung cancers, Dr. Altorki said. So, his team and others wanted to revisit the question of whether lung-sparing surgery may be a good option for some patients.
Surgeons had a choice of lung-sparing surgery type
For the trial—which was conducted by the NCI-supported Alliance for Clinical Trials in Oncology—Dr. Altorki and his colleagues enrolled 697 people with early-stage NSCLC from June 2007 to March 2017.
To participate in the trial, people had to meet stringent criteria. They had to have a single lung tumor that was 2 cm or less in size (about the diameter of a US penny), was in the outer third of the lung, and had not spread to nearby lymph nodes or elsewhere in the body. Participants also could not have been previously treated with chemotherapy or radiation therapy for the cancer.
Half of the participants were randomly assigned to have the entire lobe containing the tumor removed, and half were assigned to have lung-sparing surgery. For patients receiving lung-sparing surgery, each surgeon could decide whether to remove a segment of the lobe or only a wedge-shaped piece.
All participants were followed for at least 5 years, and the median follow-up time was 7 years. After 5 years, 63.6% of patients who underwent lung-sparing surgery and 64.1% who underwent lobectomy had not had their cancer come back. The 5-year overall survival in the two groups was 80.3% and 78.9%, respectively.
Similar but not identical studies
In the clinical trial from Japan, 5-year overall survival in both the lung-sparing surgery and lobectomy groups was more than 90%. The higher overall survival seen in that trial may be due to subtle differences between the two studies, such as the specific types of NSCLC that patients had, Dr. Rusch wrote.
Also noteworthy, in the Japanese trial all lung-sparing surgeries were done the same way, by removing a whole segment of the lung. Some surgeons think that surgery to take out a segment of the lobe, known as segmentectomy, “is a better operation” than removing a wedge-shaped piece, Dr. Cooke said, because segmentectomy also removes the associated lymph nodes in that portion of lung.
However, at least for patients with limited lung function, wedge surgery “is the most frequently practiced method of sublobar surgery in North America and Europe,” Dr. Altorki and his colleagues wrote. In their trial, which included sites in the United States, Canada, and Australia, about 60% of patients assigned to lung-sparing surgery underwent wedge surgery, making the trial “more representative of a ‘real-world’ setting,” they wrote.
One possible concern about the trial, Dr. Cooke said, is that it did not compare the two types of lung-sparing surgery directly. However, Dr. Altorki said, his team will soon have data to address this question.
Benefits of having less lung tissue removed
“Now that lung cancer screening for people at high risk is generally accepted, and as more people get screened, we expect that there will be more people who have these types of very early–stage tumors and who would benefit from sublobar surgery,” Dr. Altorki said.
“Although all these operations are now safe, lung-sparing surgery is associated with an even lower risk [of serious complications, including death], than lobectomy,” Dr. Rusch wrote.
Perhaps most important, removing less lung tissue is believed to preserve lung function. However, neither trial found clinically meaningful differences in lung function between people who had a lobectomy and those who had lung-sparing surgery.
That could be because the studies assessed lung function using instruments that measure the amount of air entering and leaving a person’s lungs, Dr. Cooke said. Neither trial included other, more sensitive measures of lung function or used standard tests to assess people’s aerobic fitness.
In addition, he noted, investigators did not ask patients to report how they felt after undergoing the two types of lung surgery.
Removing only a segment or a wedge offers another advantage for patients, Dr. Altorki said. People who are cured of their first non-small cell lung cancer are often at high risk of developing a second primary non-small cell lung cancer. And if a second lung cancer is found, people who initially had less lung tissue removed have more treatment options than those who had an entire lobe removed.
The era of precision lung cancer surgery
Despite these benefits, Dr. Altorki stressed, lung-sparing surgery won’t be the best option for everyone. “We need to do whatever is necessary to get a cure, or to get rid of the cancer and reduce the chance of recurrence as much as possible,” he said.
“When appropriate, lobectomy should still be performed,” Dr. Rusch wrote. “The era of ‘precision’ surgery for non-small cell lung cancer has arrived.”
Dr. Cooke compared the changing views on surgery for lung cancer to the evolution of surgical approaches for treating breast cancer. Over the years, breast surgeons have moved from doing radical mastectomies to lumpectomy or other breast-conserving surgery for some people with early-stage breast cancer.
When it comes to treating lung cancer, Dr. Cooke said, “We can’t stop here. The question now is, where does sublobar surgery fit in when we talk about precision medicine” for lung cancer? That could include treating people with immunotherapy or drugs that target specific genetic changes in a tumor before or after surgery, he said.
“This is an exciting time in the surgical care of patients with lung cancer, and it will be exciting to see where we go next,” Dr. Cooke added.