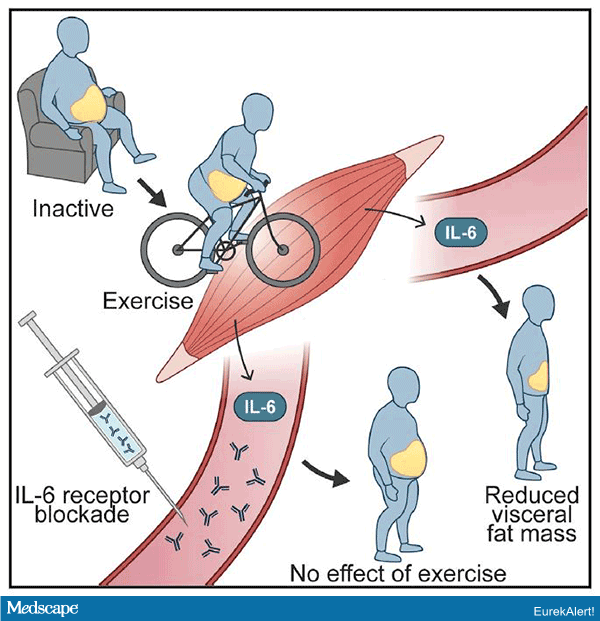
Three months of stationary-bike endurance exercise training decreased abdominal visceral fat in obese patients, but not when they were also receiving tocilizumab (RoActemra, Roche), an antibody that blocks interleukin-6 (IL-6) receptors, in a new exploratory trial.
“To our knowledge, this is the first study to show that IL-6 has a physiological role in regulating visceral fat mass in humans,” said lead author Anne-Sophie Wedell-Neergaard, MD, PhD student, University of Copenhagen, Denmark, in a statement from her institution, released to coincide with publication of the study in Cell on December 27.
“We all know that exercise promotes better health,” she continued, “and now we also know that regular exercise training reduces abdominal fat mass and thereby potentially also the risk of developing cardiometabolic diseases.”
According to Wedell-Neergaard, physicians should tell patients “when you start exercising, you may increase body weight due to increased muscle mass. So, in addition to measuring your overall body weight, it would be useful, and maybe more important, to measure waist circumference to keep track of the loss of visceral fat mass and to stay motivated.”
This study also “raises a potentially important side effect of IL-6 receptor antibodies, such as tocilizumab” (that is, they block the belly-shrinking effect of exercise in obese patients), the researchers note.
Tocilizumab also increased total cholesterol and LDL-cholesterol compared with placebo both in participants in the “exercise” or “no-exercise” groups.
However, it remains to be seen whether these effects are also true for non-obese patients.
IL-6 and Waist Slimming Effect of Exercise
Abdominal adiposity with visceral fat surrounding internal organs, Wedell-Neergaard and colleagues write, is associated with increased risk of cardiometabolic disease, cancer, dementia, and earlier death.
On the other hand, exercise stimulates lipolysis, which is often attributed to the effect of epinephrine.
The researchers hypothesized that IL-6, which is released by skeletal muscles during exercise, may play a role in exercise-induced reductions in abdominal visceral tissue mass.
To test this, they randomized 67 physically inactive adults at their center who had a waist circumference of ≥ 88 cm for women or ≥ 102 cm for men to one of four groups:
- No exercise plus placebo (18 patients)
- No exercise plus tocilizumab (18 patients)
- Exercise plus placebo (16 patients)
- Exercise plus tocilizumab (15 patients)
Exercise consisted of several 45-minute supervised exercise-bike endurance training sessions per week for 12 weeks.
Tocilizumab (8 mg/kg body weight diluted in saline) and saline placebo were given as three monthly injections infused over 1 hour.
Five patients in each no-exercise group and two patients in each exercise group dropped out or did not adhere to the study protocol, leaving 53 patients for the data analysis.
Patients were a mean age of 44 years and had a mean body mass index of 33 kg/m2. Three quarters (40/53) of participants were women.
Researchers measured visceral fat mass using MRI at the beginning and end of the study.
After 12 weeks, visceral fat mass was reduced by 225 g, or 8%, in the exercise plus placebo group compared with the no exercise plus placebo group.
The 8% reduction in visceral adipose tissue with exercise was lower than the 15% to 20% reductions reported in other studies, likely because of longer exercise sessions in the other studies, the researchers suggest.
There was no exercise-induced decrease in visceral tissue mass, however, when patients received the IL-6 blocker tocilizumab. Rather, visceral adipose tissue increased by 278 g more in the exercise plus tocilizumab group than in the exercise plus placebo group.
However, IL-6 blockade did not affect improvements in cardiorespiratory fitness, which were the same in both exercise groups.
This is an exploratory study, the authors caution, with a small number of participants. Nevertheless, the findings were consistent for both sexes.
In addition, chronic low-grade elevations of IL-6 are seen in patients with severe obesity, type 2 diabetes, and cardiovascular disease, the researchers note, so it is “likely that IL-6 may act differently in healthy and diseased people.”
Nevertheless, “this study has consolidated a physiological role of IL-6 as a lipolytic factor in humans with abdominal obesity and highlights a potentially important metabolic consequence of IL-6 blockade.”
“It remains to be clarified,” they conclude, “whether IL-6 regulates visceral adipose tissue mass in humans with all waist circumferences.”