A new study on the efficiency of the so-called ‘artificial pancreas’ suggests it’s a huge leap in the right direction for people with diabetes who are in constant need of monitoring their blood glucose.
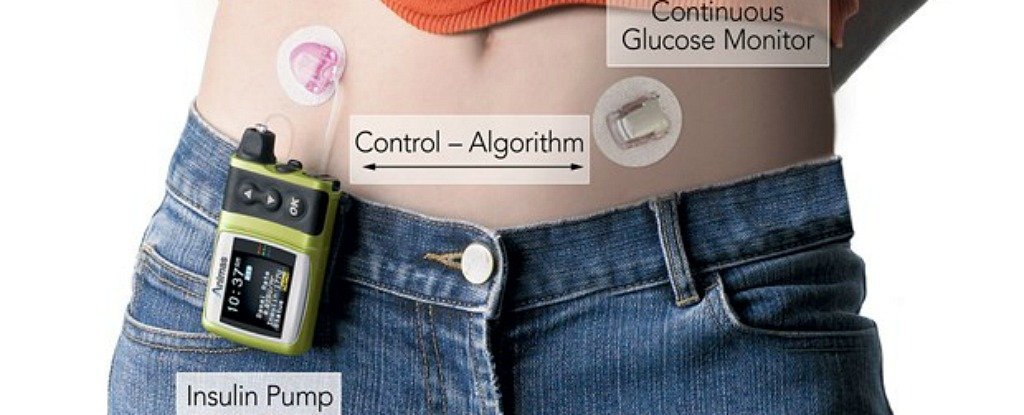
The technology works through a sort of closed loop system that monitors a person’s blood’s glucose while delivering doses of the right hormones – and for many this device is a dream come true.
In a systematic review of the evidence to date, a team led by researchers from the Aristotle University of Thessaloniki has evaluated 41 studies on the safety and efficacy of two types of artificial pancreas used by more than 1,000 volunteers.
The team found that volunteers trialling this class of device spent roughly 10 percent more time within a healthy range of blood glucose levels over any given 24 hour period.
That’s encouraging news, showing medicine is heading in the right direction, but more questions will need to be answered about balancing the risks, costs, and benefits of this amazing device.
Diabetes describes a class of conditions that make it difficult for the body to manage its sugar levels, either due to problems producing the insulin needed for cells to absorb glucose, such as type-1 diabetes, or resistance to insulin, like type-2.
This requires those with type-1 diabetes to check their blood levels and monitor their diet while potentially administering specially calculated doses of insulin.
While this sounds simple in principle, for millions of people this is a finicky task that can feel like balancing an egg in an earthquake, as a wide range of variables make it virtually impossible to maintain that perfect level of glucose.
Modern technology has helped in many ways, providing pumps that can accurately administer insulin and continuous monitoring devices that keep a careful minute-by-minute watch on blood glucose.
But these tools still require a human in between to make key judgements.
That’s what makes the ‘artificial pancreas’ tech so awesome – it aims to take the burden of decision making by having algorithms determine how much insulin or another balancing hormone called glucagon to inject in response to measurements of glucose in the blood.
While it’s not quite the same thing as a functional pancreas, for those with the condition it can reduce stress while providing some peace of mind at night.
A terrifying consequence of diabetes – especially among young people – is the risk of dying while asleep, possibly due to missing vital signs of critically low blood sugar.
It’s easy to see why many of those dealing with diabetes are keen to get their hands on this kind of tech, and this latest review shows it has potential to live up to its hype.
But the team conducting the research is also calling for higher quality studies – for example, none of the trials on young people with diabetes included children under five years old.
Three quarters of the trials evaluated were also just a week long, which provides limited information on the longer term effects of these closed-loop delivery systems.
What this means is we still have some way to go for artificial pancreas technology to conclusively prove its worth.
For policy makers, this is important stuff. New technology is often expensive, forcing many people to rely on insurance and government subsidies to afford these treatments.
If the evidence is scant on cost-benefit-ratios, only the wealthiest can afford that extra comfort. Importantly, without extensive studies, it’s possible some people with complications or slight variations in their condition might miss out on important caveats.
“Patients with particular problems, such as hypoglycaemia without warning symptoms, could benefit more,” says medical researcher Norman Waugh from the University of Warwick, whose commentary on the research calls for better studies.
“For children, we need data on parents’ quality of life. We need a trial of the dual insulin and glucagon system in cystic fibrosis related diabetes, where pancreatic and hepatic damage impairs responses to both hypoglycaemia and hyperglycaemia.”
Each year, research on this life-changing condition gives us hope of better ways to prevent, treat, or even cure diabetes.
We have every reason to celebrate the progress we make, but after the excitement dies down there is still a need to collect as much evidence as possible to make sure it really does live up to our expectations.
For all book lovers please visit my friend’s website.
URL: http://www.romancewithbooks.com
