Abstract
Background
Trastuzumab is the only first-line treatment targeted against the human epidermal growth factor receptor 2 (HER2) approved for patients with HER2-positive advanced gastric cancer. The impact of metabolic heterogeneity on trastuzumab treatment efficacy remains unclear.
Methods
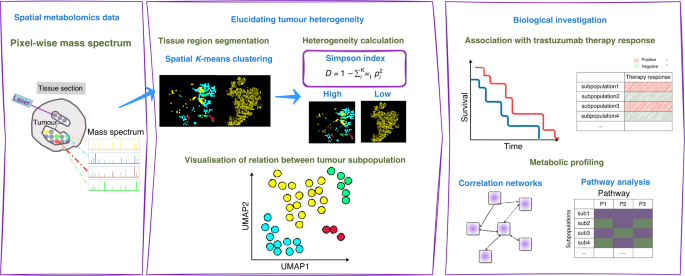
Spatial metabolomics via high mass resolution imaging mass spectrometry was performed in pretherapeutic biopsies of patients with HER2-positive advanced gastric cancer in a prospective multicentre observational study. The mass spectra, representing the metabolic heterogeneity within tumour areas, were grouped by K-means clustering algorithm. Simpson’s diversity index was applied to compare the metabolic heterogeneity level of individual patients.
Results
Clustering analysis revealed metabolic heterogeneity in HER2-positive gastric cancer patients and uncovered nine tumour subpopulations. High metabolic heterogeneity was shown as a factor indicating sensitivity to trastuzumab (p = 0.008) and favourable prognosis at trend level. Two of the nine tumour subpopulations associated with favourable prognosis and trastuzumab sensitivity, and one subpopulation associated with poor prognosis and trastuzumab resistance.
Conclusions
This work revealed that tumour metabolic heterogeneity associated with prognosis and trastuzumab response based on tissue metabolomics of HER2-positive gastric cancer. Tumour metabolic subpopulations may provide an association with trastuzumab therapy efficacy.
Background
Gastric cancer (GC) is currently the fourth most common cause of cancer-related deaths globally [1]. Trastuzumab, a recombinant humanised monoclonal antibody directed against the human epidermal growth factor receptor 2 (HER2), is the only targeted agent approved for the first-line treatment of patients with HER2-positive advanced GC [2]. Trastuzumab combined with platin–fluoropyrimidine chemotherapy improves survival outcomes in HER2-positive GC [2]. Nevertheless, only a subgroup benefits from the addition of trastuzumab to chemotherapy. The overall response rate of the combined therapy is less than 50%, indicating that a considerable proportion of HER2-positive cancers are resistant to HER2 inhibition [3]. Optimising the selection of HER2-targeted regimens by identifying patient subpopulations who would benefit from trastuzumab could be cost-effective and would spare some patients unnecessary exposure to ineffective treatments.
Molecular heterogeneity exhibits a variety of biological behaviours in cancers [4]. Exploring the patterns of molecular heterogeneity are necessary to design personalised targeted regimens to increase patient response [5,6,7,8]. GC has a high level of genomic and phenotypic variability even within individual tumours, and this underlying heterogeneity is considered as a major cause for the frequent failure of biomarker-based clinical trials [9,10,11]. High incidence of HER2 heterogeneity was observed in GC and it was associated with chemotherapy [12] and trastuzumab efficacy [13]. Several studies uncovered proteomic subpopulations that were linked to patient survival in GC [14,15,16]. Metabolic reprogramming has been recognised as one hallmark that can be used to prevent therapeutic resistance [17]. Metabolomics, a predictor of drug therapeutic response in cancers [18, 19], can generate metabolite profiles and also combine this information with changes in crucial metabolic pathways, such as Warburg effect, altered amino acid/lipid/drug metabolism, generation of drug-resistant cancer stem cells, and immunosuppressive metabolism [17]. Metabolite profile was considered an important factor besides HER2 status in assessing the initial response to trastuzumab treatment for GC patients [20, 21]. Specifically, one study revealed tumour metabolic heterogeneity within HER2/neu-positive and HER2/neu-negative GC cells [22]. Nonetheless, the impact of intratumoural and intertumoural metabolic heterogeneity on trastuzumab response in HER2-positive advanced GC remains unclear. Matrix-assisted laser desorption/ionisation–imaging mass spectrometry (MALDI–IMS) enables the imaging of different molecular classes in their histopathological context and thus the allocation of molecular profiles to specific tumour cell types [23,24,25]. This high cellular specificity is behind the increasing popularity of IMS and its proven ability to identify diagnostic and prognostic biomarkers [26,27,28]. Additionally, MALDI–IMS is an omics technique that allows for the global characterisation of the spatial metabolomics [29, 30], which offers an opportunity to demonstrate the drug-resistant tumour profile with metabolic heterogeneity and discovering the alteration in the tumour microenvironment [17]. Combined with statistical tools, MALDI-IMS constitutes a unique tool to reveal a priori tumour subpopulations that are not distinguishable using conventional histopathological methods, but which are molecularly distinct [31,32,33].
We apply spatial metabolomics and K-means clustering method to identify metabolically distinct tumour subpopulations of HER2-positive advanced GC from routinely preserved pretherapeutic biopsies, and assess their relationships with the response to trastuzumab treatment. The workflow of this study is shown in Fig. 1.
Discussion
In the present study, we discovered heterogeneity in a series of patients with HER2-positive advanced GC based on tissue metabolomics. We defined nine distinct metabolic subpopulations. Of the nine subpopulations, two subpopulations were associated with favourable prognosis and trastuzumab sensitivity, and one subpopulation was associated with poor prognosis and trastuzumab resistance. Additionally, tumour metabolic heterogeneity was associated with prognosis and trastuzumab response. To our knowledge, this study is the first to investigate the impact of metabolic heterogeneity on the trastuzumab treatment efficacy and survival in HER2-positive advanced GC. A higher degree of tumour metabolic heterogeneity associated with a better prognosis and trastuzumab sensitivity. This observation is in line with previous studies [12, 38]. One study described the high incidence of intratumoural HER2 heterogeneity in a large series of 322 patients with GC in detail by performing HER2 immunohistochemistry (IHC) and fluorescence in situ hybridisation (FISH) and evaluating the gene copy number individually in distinct areas with different IHC staining intensity. In addition, they further revealed that HER2 heterogeneous positivity was associated with longer survival than the homogeneous [12]. Another study consistently reported proteomic heterogeneity and their positive correlation with prognosis in HER2-positive breast cancer patients treated with trastuzumab [38]. Moreover, they revealed that high heterogeneity of tumours could reflect the presence of heterotypic components including infiltrating immune cells, which facilitated the response to treatment [38]. This could be the possible explanation of the observed correlation between a higher metabolic heterogeneity and a better outcome in HER2-positive advanced GC in the present study. Taken together, those studies together with us demonstrated the association of tumour heterogeneity of the molecular expression with trastuzumab response, indicating that molecular heterogeneity should be taken into consideration when clinical therapeutic decision of trastuzumab is made. The most significant pathways among nine tumour subpopulations were related to nucleotide metabolism and carbohydrate metabolism, which are revealed to be highly spatially organised and could be visualised as different molecularly defined regions. Major changes in nucleotides and nucleotide metabolism have been linked to patient survival. Typically, cancer cells have deactivated crucial DNA damage response signalling routes and often rewire their metabolism and energy production networks [39, 40]. Anabolic metabolism of DNA was identified as an important downstream effect of the HER2 oncogene in breast cancer [41]. In GC, one study characterised GC with metabolomic features and identified three tumour-specific subtypes. One tumour-specific subtype comprised enriched DNA metabolism, and it predicted a benefit when initiating trastuzumab therapy [20]. Another study identified DNA metabolism as a factor influencing response to HER2-targeted trastuzumab therapy, and the changes in DNA metabolism found in patient tissues were validated in a HER2-positive/sensitive and HER2-positive/resistant GC cell model [21]. The nucleotide metabolites GDP and GMP showed significant effect on survival in the GC patients treated with trastuzumab therapy [21]. This study is consistent and found that the subpopulation with downregulated nucleotide metabolism (subpopulation 4) was associated with a resistance to trastuzumab therapy.
Meanwhile, correlated metabolites within the trastuzumab-sensitive subpopulaiton 9 comprise different carbohydrate compounds, such as D-Glucosamine, D-Fructose 6-phosphate and D-Glucose 1-phosphate. These compounds are involved in different pathways contributing to tumour cell survival [42, 43]. D-glucosamine and and its derivatives have shown their anti-tumour effects on cell proliferation, cell death and angiogenesis in human bodies, although the precise function and mechanism remains to be clarified [43]. Additionally, carbohydrate metabolism is the major HER2-related altered metabolic pathway, and the association of glucose metabolism with HER2-positive breast cancer was confirmed [44, 45]. Gluconeogenesis in HER2-positive breast cancer was upregulated for energy supply, resulting in enriched consumption of related amino acids [46]. In particular, previous studies support our observation in the metabolite networks that the metabolites succinate, sn-glycerol 3-phosphate, 5’-Methylthioadenosine and diphosphate showed significant importance in distinguishing trastuzumab-sensitive and trastuzumab-resistant patients, which can be interpreted as the potential biomarkers for the trastuzumab therapy response [20, 21]. However, these new potential metabolite biomarkers and their related metabolisms have not yet fully investigated in GC. A greater understanding of these metabolite biomarkers in the future could reveal detailed insights into the molecular changes underlying GC disease, metabolic responses to treatments, and mechanisms leading to trastuzumab therapy response.
One challenge in identifying metabolic heterogeneity for their association with trastuzumab response is the limited number of tumour samples. All patients must have HER2 positivity, trastuzumab treatment, and adequate follow-up. Industry-sponsored controlled clinical trials do exist; however, the availability of these studies for independent research is unfortunately limited. Although the number of tumour samples is limited in the current study as well, the samples and associated data still offer some advantages. The tissue specimens in this study were collected from many sites. Furthermore, HER2 testing was centrally performed with the highest quality standards [34]. This ensured that the inclusion criteria were validated for each tumour sample. In conclusion, we demonstrated the importance of considering tumour metabolic heterogeneity in HER2-positive advanced GC for optimising patient management. Consequently, tumour metabolic heterogeneity showed an impact on trastuzumab efficacy and patient outcomes. These findings should be validated in larger independent cohorts, and additional molecular correlative analysis are warranted.